Download PDF
Matthew Sax,* a 30-year-old engineer, started to be bothered by a gray spot that appeared in his vision in his left eye. Initially, the spot was small and Mr. Sax almost didn’t notice it. Over the next few days, however, as the spot grew bigger and darker, he knew it was time to get it checked out.
We Get a Look
Presentation. When Mr. Sax presented to our urgent care ophthalmology clinic, he complained of a blurry spot in the center of his vision in his left eye. He told us that he was not experiencing any pain.
History. Mr. Sax told us that there had been no trauma to the eye, he had no history of eye infections, and he hadn’t undergone any eye surgeries. He had no significant past medical history and did not take any medications.
He mentioned that he recently recovered from a viral episode that he had contracted from his 2-year-old son. The illness began with flu-like symptoms and a fever of 102.5 degrees Fahrenheit. Two days after his fever broke and he began feeling better, a maculopapular rash broke out on his hands, he developed sores in his mouth, and he noticed the spot in his vision. On the day that he presented to our clinic, he still had residual lesions on his hands that appeared hyperpigmented and erythematous.
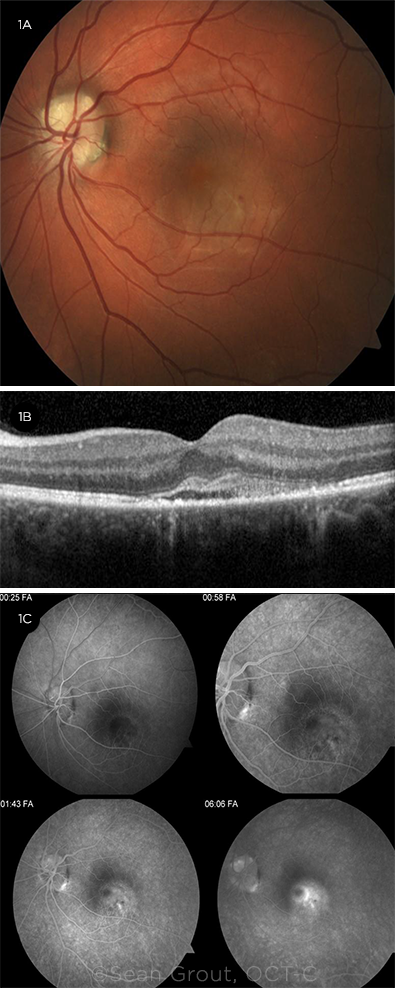
Exam. His BCVA was 20/20 in the right eye and 20/200 in the left. His IOP was 12 mm Hg in the right eye and 13 mm Hg in the left. We noted no afferent pupillary defect or any ocular motility disturbances. The slit-lamp examination showed no evidence of anterior chamber inflammation or vitritis. The fundus examination showed a normal disc in the right eye and an incidental finding of an optic disc drusen in the left eye. In his right eye, the retina appeared normal; in his left, we noted macular thickening with focal intraretinal hemorrhages along the inferotemporal arcade (Fig. 1A).
 |
|
HIS LEFT EYE AT INITIAL PRESENTATION. (1A) Fundus photography showed a scalloped appearance of the optic disc at the inferotemporal disc margin, and the macula was thickened with focal intraretinal hemorrhages along the inferotemporal arcade. (1B) OCT showed a pocket of SRF with hyperreflective debris involving the fovea. (1C) FA showed early hypofluorescence in the inferotemporal macula followed by late stippled hyperfluorescence and a pooling pattern corresponding to the area of the SRF.
|
Tests
Spectral-domain OCT (SD-OCT) was normal in his right eye. SD-OCT of the left eye showed a pocket of subretinal fluid (SRF) involving the fovea with hyperreflective debris in the subretinal space (Fig. 1B).
Fluorescein angiography (FA) of the left eye showed early hypofluorescence in the inferotemporal macula followed by late stippled hyperfluorescence and a pooling pattern corresponding to the area of the SRF (Fig. 1C).
Differential Diagnosis
Clinically, Mr. Sax presented with unilateral acute onset of SRF. For the differential diagnosis, we considered central serous chorioretinopathy (CSR), choroidal neovascularization (CNV), unilateral acute idiopathic maculopathy (UAIM), or an inflammatory process, such as Vogt-Koyanagi-Harada (VKH) disease. However, he didn’t have any anterior chamber or vitreous inflammation that would have been suggestive of VKH.
UAIM. UAIM was the leading diagnosis based on the clinical and imaging findings. UAIM typically follows a viral infection, making Mr. Sax’s recent illness a key piece of information when considering our differential.
CSR. CSR seemed less likely because of the turbidity of the SRF (see the hyperreflective debris in Fig. 1B) and the intraretinal hemorrhage, neither of which are typically seen with that diagnosis. Indeed, Mr. Sax had no prior episodes of CSR and no history of recent steroid use, which is a risk factor for CSR.
CNV. His FA characteristics did not show a leakage pattern consistent with CNV, nor did OCT show a retinal pigment epithelial detachment, thus ruling out CNV.
Lab Results
Several cases in the literature have associated UAIM with hand, foot, and mouth disease (HFMD), which is an infection caused by coxsackievirus. Given Mr. Sax’s history of flu-like symptoms and rash, we ordered serology testing for antibodies to coxsackievirus types A and B.
The testing was positive for coxsackievirus B antibodies, confirming our suspicions.
Treatment
After discussing the differential diagnosis and informing Mr. Sax that his condition would likely self-resolve, we decided that conservative management with close follow-up was the most appropriate management.
 |
|
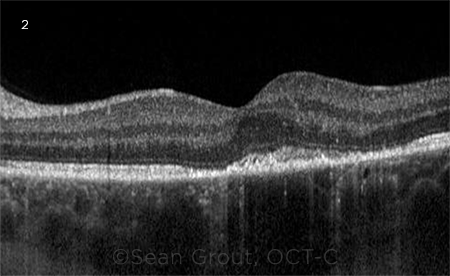
FOLLOW-UP. (2) One week after we first saw Mr. Sax, OCT demonstrated near resolution of SRF in the left eye. However, persistent subretinal hyperreflective material and disruption of the ellipsoid and photoreceptors remained.
|
Discussion
UAIM was first described in 1991 by Yannuzzi et al. in a case series of nine middle-aged, healthy White patients, who presented with unilateral acute central vision loss and corresponding neurosensory detachment in the macula. Additional clinical findings relating to UAIM may include turbid subretinal exudates, papillitis, and intraretinal hemorrhages.1
The pathogenesis of UAIM is unknown. It presents as an inflammatory maculopathy that affects the outer retina and retinal pigment epithelium (RPE). The majority of patients are reported to have a flu-like prodrome prior to their visual complaints. Several case series have suggested that viral etiologies may lead to UAIM.2 By far, the most common viral etiology involves infection with a strain of coxsackievirus, a single stranded RNA enterovirus known to cause HFMD.3
Without treatment, the natural course of UAIM leads to a rapid, spontaneous improvement in vision and corresponding resolution of the neurosensory detachment. Several authors have explored a role for empiric corticosteroid therapy4 or injection with intravitreal anti-VEGF agents5 as first-line treatment. However, this remains controversial given the good visual outcomes achieved with observation alone.
As further cases of UAIM are reported in the literature, more will be learned about its pathogenesis and the associated viral etiologies. This should allow clinicians to more accurately diagnose, suggest treatments for, and manage this rare disease.
 |
|
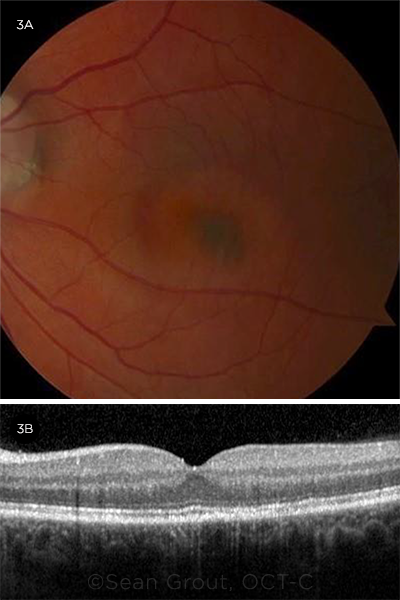
Two months after the initial presentation, (3A) fundus photography showed a hyperpigmented scar in the inferonasal fovea, and (3B) OCT demonstrated improvement in foveal contour and ellipsoid integrity with mild RPE mottling in the area of resolved SRF.
|
Our Patient’s Course
Mr. Sax returned to our clinic one week later. Although he reported no significant improvement in the vision of the left eye, BCVA in that eye was 20/60.
The examination showed resolution of the intraretinal hemorrhages. On OCT, there was near resolution of the SRF, but we noted persistent subretinal hyperreflective material and disruption of the ellipsoid and photoreceptors (Fig. 2). Given the improvement, we elected to continue conservative management.
Two months following his initial presentation, Mr. Sax came to the clinic reporting an incremental improvement in his vision. BCVA in his left eye was 20/20. On examination of the macula, there was a hyperpigmented circular lesion inferonasal to the fovea, which corresponded to a scar on his fundus photo. OCT demonstrated improvement in foveal contour and ellipsoid integrity with mild RPE mottling in the area of resolved SRF.
___________________________
* Patient name is fictitious.
___________________________
1 Yannuzzi LA et al. Arch Ophthalmol. 1991;109(10):1411-1416.
2 Freund KB et al. Arch Ophthalmol. 1996;114(5):555-559.
3 Duman R et al. Int Ophthalmol. 2016;36(3):445-452.
4 Agrawal R et al. J Ophthalmic Inflamm Infect. 2015;5:2.
5 Mylonas G et al. Eur J Ophthalmol. 2018;28(2):256-258.
___________________________
Dr. Blahnik is a research fellow in the Department of Ophthalmology at the University of North Carolina (UNC), Chapel Hill. Dr. Huynh is in private practice in Southern California. Dr. Zhang is an assistant professor of ophthalmology and vitreoretinal surgeon at UNC, Chapel Hill. Financial disclosures: None.