Download PDF
Providing treatment while protecting quality of life.
The aging ophthalmology patient population can present a vivid study in contrasts between physician and patient. Charles C. Wykoff, MD, PhD, for example, is of the younger generation of retina specialists. Anti-VEGF agents were introduced to clinical practice for the treatment of age-related macular degeneration (AMD) when Dr. Wykoff was a resident.
Today, in his practice with the Retina Consultants of Houston, he treats many elderly patients. Five of his AMD patients are over 100 years old, and “many more” are in their 90s—a phenomenon Dr. Wykoff finds remarkable. “This is a very special group of people who have taught me that, in many cases, age is largely a state of mind,” he said. “Indeed, age in and of itself is not a limiting factor to being able to both tolerate and benefit from intravitreal injections. If the injections will help to maintain a good quality of life, then the older patients want to receive them.”
The Silver Tsunami
Dr. Wykoff’s experience mirrors a demographic reality: America is aging rapidly. Hilary A. Beaver, MD, of the Blanton Eye Institute at Houston Methodist Hospital, cites the fastest-growing cohort in the country, known as the “extreme elderly” or the “oldest old.” This patient population, aged 85 and older, is projected to rise from 6.2 million in 2014 to 19 million in 2050.1
Ophthalmologists are second only to geriatricians in the number of patients over 65 that they see, said Dr. Beaver, who serves as chair of the Academy’s Committee on Aging. “This actually shouldn’t be surprising, given that our highest volume of patient visits involves cataract, glaucoma, AMD, and diabetic retinopathy—all diseases of aging. Young internal medicine and family practice residents who rotate through my practice have observed that we have an ‘old waiting room.’”
A Unique Set of Treatment Challenges
While the extreme elderly eye does not differ much physiologically or anatomically from the eyes of Baby Boomer patients now in their 60s and 70s, other extenuating factors can make treating this ophthalmic population challenging.
Chronic illnesses. In many instances, extremely elderly patients are coping with a long history of chronic comorbid conditions in addition to their ocular issues. “We need to keep in mind their other medications and long prior medical history, especially if we are taking someone to surgery with a pacemaker or an automatic defibrillator. Our anesthesiology preop clinic is particularly attuned to this,” said neuro-ophthalmologist Bradley J. Katz, MD, PhD, of the Moran Eye Center at the University of Utah.
Dementia. The practical mechanics of treatment may, of necessity, be different for patients who have Alzheimer disease or other dementias. With regard to intravitreal injections, for instance, patients “may move suddenly, be unable to cooperate, or be able to look only in a certain direction,” Dr. Wykoff said. “We must adapt to each unique situation to deliver the injections.”
For dementia patients who need a surgical procedure, Dr. Katz recalled the time he arranged for the wife of one of his patients with dementia to accompany him to the operating room (following strict sterilization procedures). “While this nontraditional approach is against protocol, her presence [as she held his hand] was the best anesthesia we could have chosen,” he said.
Hearing. Patients in their 80s and 90s have a much higher incidence of hearing impairment, which can lead to problems communicating in both the examination and the operating rooms. “We need to be sure the patient understands what we say when we talk about diagnosis and treatment,” Dr. Katz said. He added, “It is particularly challenging in the operating room. Patients have to remove their hearing aids, so we find ourselves shouting instructions when we need them to comply with a request.”
Eye Conditions of the Oldest Old
A number of eye conditions are more common in older patients. While the following is by no means a comprehensive list, here are some to consider.
Alzheimer’s visual variant. Although Alzheimer disease typically presents with memory problems, some patients have the visual variant. In these cases, the initial manifestation of the disease involves trouble with their vision.
These patients present with vague complaints, Dr. Katz said, such as blurred vision, difficulty reading, or a sense that words are jumping around on the page. However, their visual acuity is normal, and their eye exams are usually unrevealing. These patients can “see” fine, but they cannot comprehend or decipher the images.
“The problem is with higher cortical function—the visual parts of the brain that make sense out of the images that are sent from our eyes,” Dr. Katz explained. “If you suspect a patient has this problem, there’s a quick screening test you can use that was developed by neuro-ophthalmologist Jonathan D. Trobe, MD.2 If a patient fails this screening test, they should be referred to a neurologist who specializes in cognitive disorders or Alzheimer disease for further evaluation.”
AMD. Many AMD patients who begin intravitreal anti-VEGF injections in their late 70s will live many more years. The long-term use of these drugs can involve clinic visits and injections month after month, year after year, which can become a logistical challenge.
While anti-VEGF drugs can prevent scarring of the retina, researchers still need to focus their efforts on treatments that do not require frequent visits and injections, said Neil M. Bressler, MD, at the Wilmer Eye Institute in Baltimore.
“Even if we can stop this scarring, the underlying pathology of AMD [drusen] inevitably leads to atrophy of the macula,” Dr. Bressler said. “In fact, some of the oldest old patients may never develop the neovascular form of AMD, but they eventually will develop atrophy. And we have no idea how to stop the development or growth of atrophy—it doesn’t occur quickly, but once it starts, it continues slowly but surely.”
 |
|
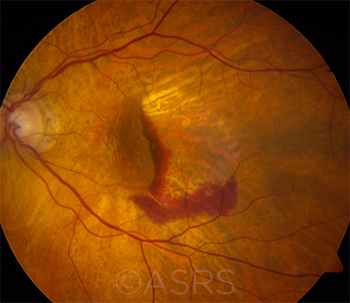
AMD. This 76-year-old patient with wet AMD could live another 10, 15, or more years.
|
Giant cell arteritis. While giant cell arteritis (GCA) is relatively rare, it can cause blindness very quickly in both eyes if not treated rapidly. “One of my teachers in Iowa called GCA the only true eye emergency,” Dr. Katz said. “It is a disease of age, and we should always be on the lookout for it, especially in patients in their 80s and 90s.”
In addition to myalgias in the large muscle groups and fatigue, 2 telltale signs of GCA are scalp tenderness and jaw claudication. “In patients with GCA, it is important to start high-dose steroids immediately to save vision,” Dr. Katz said. “This approach is highly effective at preventing vision loss,” but the high-dose regimen of prednisone, along with a long taper, exposes the patient to serious systemic effects.
Dr. Katz recommended staying in close touch with a rheumatologist throughout treatment, adding that the search continues for effective immunomodulatory drugs to serve as an alternative to prednisone in the management of these patients.
 |
|
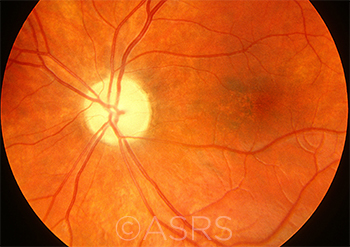
GCA. Arteritic anterior ischemic optic neuropathy and choroidal ischemia in a patient with GCA.
|
Optic atrophy. A decline in optic nerve fibers occurs over time as we age. A marked difference can be observed between adults in their 50s and 60s and those in their 80s and 90s, said neuro- ophthalmologist Michael S. Lee, MD, of the University of Minnesota.
Optic atrophy in the extreme elderly can be caused by a long list of factors, which creates a diagnostic challenge. Potential causes include tumors, other compressive abnormalities, and toxic exposures to medications or chemicals. Nutritional deficiencies can also play a role, and a history of chronic diarrhea, colon surgery, gastric bypass surgery, or other risk factors for vitamin B12 deficiencies (including alcoholism) are worth investigating.
Dr. Lee said that when exploring possible causes of progressive optic atrophy in his patients, he usually considers “SLSL” (sarcoid, lupus, syphilis, and Lyme disease). “I know that syphilis is not necessarily associated with elderly patients,” he said, “but sexually transmitted diseases are becoming more common in nursing homes. While older patients might balk at the possibility, it is a treatable cause of vision loss.” And some older patients may have chronic syphilis, which was acquired decades earlier.
As for exposure to chemicals, one of Dr. Lee’s optic atrophy patients had been stripping varnish in a poorly ventilated room and progressively lost vision; another older female patient who worked with stained glass and had been exposed to soldering fumes over many years also experienced progressive vision loss.
The clinical workup depends on whether changes in acuity are progressive or stable. Ordering magnetic resonance imaging (MRI) of the orbit with and without contrast and fat suppression “is a reasonable first step in diagnosis,” Dr. Lee said. “If the gadolinium-enhanced MRI cannot be tolerated by an elderly patient, a contrast CT could also be done.”
 |
|
OPTIC ATROPHY. The list of potential causes is long and includes nutritional deficiencies, chemical exposure, and tumors.
|
Sagging eye syndrome. Ironically, it was a pediatric ophthalmologist (Joseph L. Demer, MD, PhD) who first described “sagging eye syndrome,” a leading cause of strabismus in older adults.3
Connective tissue structures act as pulleys to constrain the paths of the lateral rectus extraocular muscles (EOMs). When the pulleys sag, the eyes turn in, causing double vision. In his research, Dr. Demer found that “widespread pulley displacement and EOM elongation, associated with lateral rectus–superior rectus band rupture, causes acquired vertical and horizontal strabismus.”
Dr. Katz has found himself diagnosing this syndrome more frequently among his adult patients. “An increasing number of patients in their late 60s and older are presenting with complaints of double vision. It turns out that many of these patients have sagging eye syndrome,” he said.
“The beauty of the syndrome is that we don’t need expensive imaging or blood tests to determine the cause,” Dr. Katz added. “It takes a minute to figure it out and is very easy to treat by placing a prism in the patient’s glasses.”
He cited an older patient who was worked up by a neurologist for a global muscle weakness. The patient complained of double vision, and the neurologist referred him to Dr. Katz. “I observed that he had ptosis and a superior sulcus deformity. After completing my measurements, I confirmed that the patient had sagging eye syndrome, a condition not related to his other neurological problems. I gave him a pair of glasses with a prism in it, and his double vision cleared.”
 |
|
SAGGING EYE. This 77-year-old presented with a complaint of intermittent, binocular, horizontal diplopia that was present only at distance. After an extensive evaluation that included neuroimaging, she was given a prescription for ground-in prism for her sagging eye syndrome.
|
Ethical and Practical Considerations
While “no one is too old to benefit from treatment, and patients in their 90s could live another 5 to 10 years,” as Dr. Bressler said, a variety of ethical and practical points must be addressed.
Treatment plans. Ophthalmologists should work with the patient and family to establish an appropriate treatment plan. For instance, “When you are taking care of a 92-year-old patient with mild to moderate glaucoma, how aggressive do you want to be?” asked Dr. Katz. “What are the odds these patients are going to live another 10 years? And do they want to be bothered with using eye drops 2 times a day or coming in constantly for pressure checks?”
“We need to consider age, costs, and inconvenience, remaining aggressive enough to keep them sighted but trying not to decrease their quality of life,” Dr. Beaver said. “Maintaining vision is a huge quality of life issue, and cataracts are a good example. Some patients make it into their 90s before they need cataract surgery. Working with the patient, we must weigh the benefits of eyesight with the risks associated with anesthesia and recovery.”
Informed consent. This process is crucial and can be particularly challenging with elderly patients, Dr. Wykoff noted. Even though a patient may appear to understand what the physician is saying, actual decisions regarding diagnostics and management options may need to involve a medical power of attorney, family member(s), and/or other supporting people. It is important to identify the person responsible for making decisions regarding health care, he said, and the ophthalmologist “needs to be sure that true informed consent is being obtained appropriately.”
Presurgical discussions for patients in this age group may involve discussion of DNR (do not resuscitate) orders so the ophthalmologist can honor a patient’s wishes in cases of cardiac arrest, Dr. Beaver said.
It’s also important to note that this cohort of patients is less apt to ask for a second opinion than are younger patients, Dr. Lee said. In addition, a recent study found that only 16% of seniors with an average age of 75 obtained health information on the Internet.4 Both of these factors can play a role in the informed consent process.
Practical challenges. Elderly patients may also struggle with a number of basic physical and logistical challenges, Dr. Wykoff said. For example, postoperative positioning following surgical repair of retinal detachments or macular holes may be problematic for patients with spine or neck conditions. In addition, it may be difficult to obtain a standard ophthalmic coherence tomography (OCT) or MRI image in some patients with orthopedic conditions because of positioning issues.
Dr. Beaver observed that elderly patients may face impediments getting to and from appointments, may experience problems opening small bottles of eyedrops due to arthritic hands, and may waste drops because tremors make it difficult to aim for the eye. Treatment costs may also be prohibitive for some.
But “despite their medical problems, for these elderly individuals, every day is a good day, and they are eager to make the best of whatever they have got,” she said. “Our goal is to help them to maintain their vision as long as possible.”
Key Aid: Low Vision Rehab
Gwen K. Sterns, MD, at Rochester General Hospital in New York, has been a member of the Academy’s Committee on Aging for several years, including serving as its chair. Dr. Sterns’ interest in low vision rehabilitation was sparked when she worked with low vision pioneer Eleanor E. Faye, MD, during her residency, and she has been an advocate ever since.
Dr. Sterns, who has seen an increasing number of extreme elderly patients over the years, observed that they want to remain as independent as possible for as long as possible. “They want to read their bills and the newspaper, be able to change their thermostat, hold a book or tablet without help, continue to differentiate their pills, and even use a computer,” she said. “Ophthalmologists should be sensitive to this need for independence.”
Low vision rehabilitation plays a key role in helping the oldest old maintain their vision, Dr. Sterns said. “When a patient breaks a leg or receives a hip replacement, he is sent to rehabilitation,” she said. “When seniors experience low vision problems due to aging, disease, or treatment issues, ophthalmologists should refer their patients for rehabilitation as well. It will help them maintain their independence and, in turn, enhance their quality of life.”
Key Resources
Comprehensive overview. The Academy’s Committee on Aging has developed a wide-ranging collection of materials that includes online podcasts, resident lectures, and resources from the American Geriatrics Society (AGS), including the AGS Delirium Guidelines.
Low vision resources. The Academy’s SmartSight materials, including the Vision Rehabilitation Preferred Practice Pattern, can be accessed online.
|
Unexpected Benefits
“One of the things I do with my older patients is to be frank and open and to have a sense of humor,” Dr. Beaver said. And as it has turned out, taking the time to help older patients—and to carefully explain their diagnosis and treatment options—is one of the most rewarding parts of her practice, she said. “I get to know them and their entire family, and they are so appreciative.”
Dr. Wykoff’s experience has been much the same. Many of his elderly patients “want to share their perspectives on life and want the best possible vision,” he said. “Some of these older patients are exceptionally appreciative of the care they receive. I enjoy getting to know the families, and it’s great to see grandchildren and great-grandchildren bringing patients in for visits.”
Dr. Beaver concluded, “We all have a vested interest in the future of ophthalmic care for the extreme elderly. Not only will we be taking care of an increasing number of these patients, but one day, if we are lucky, we will become one of them.”
___________________________
1 Older Americans 2016: Key Indicators of Well-Being. Accessed Sept. 20, 2016.
2 Trobe JD, Butter CM. Arch Ophthalmol. 1993;111(6):815-818.
3 Chaudhuri Z, Demer JL. JAMA Ophthalmol. 2013;131(5):619-625.
4 Levine D et al. JAMA. 2016;316(5):538-540.
Case Report: 92 Years Young
By Paul T. Finger, MD, and Carina T. Sanvicente, MD
In 1995, Mrs. Gisela Dollinger was a healthy 92-year-old Holocaust survivor who was referred to our center for treatment of a choroidal melanoma in her left eye. This T2-sized choroidal melanoma (according to the American Joint Committee on Cancer staging system) was located anterior to the equator, and it was 5.9 mm in thickness and 10 mm in largest basal diameter. Mrs. Dollinger’s initial visual acuity (VA) was 20/25 in both eyes. A metastatic survey was normal.
Mrs. Dollinger lived alone. She played bridge with her friends every day and got around New York City by walking and by taking buses and taxis by herself. When we discussed treatment options with her and her niece, she initially didn’t want to pursue any intervention. She said, “I’m 92, I don’t feel anything, how long do you expect me to live?” Given the tumor’s size and location, Dr. Finger knew she would have an excellent result and said, “You have no other problems, so you could live for 10 more years and with good vision in the treated eye. I don’t want you to die from metastatic melanoma.” She responded in her old-world way: “Dr. Finger, for you, I’ll do it.” Soon after, she underwent palladium-103 plaque brachytherapy.
Mrs. Dollinger’s results surpassed all expectations with no change in vision for another 9 years. During that time, she continued playing bridge, reading The New York Times, and, most important, maintaining her independence.
Unfortunately, at age 101, Mrs. Dollinger started to show symptoms of AMD. Four years later, at age 105, her vision in her good (noncancerous) eye dropped from 20/40 to 20/125 due to wet AMD. Although her vision in this eye was rescued to a mean 20/63 with periodic intravitreal anti-VEGF therapy, delivered over several years, it became increasingly difficult for her to keep up the frequency of her injection visits. She developed irreversible changes of the macula and became legally blind in that eye. Meanwhile, the left eye (the one with the choroidal melanoma) became her better eye with a VA of 20/40. (Eventually, AMD also affected the left eye. Even so, her VA in that eye was 20/50 until 2011.)
Mrs. Dollinger returned for her last visit with us in October of 2012. At that time, she was 110 years old. Her VA was 20/200 in her right eye and 20/100 in the left. Periodic bouts of pneumonia had kept her cycling in and out of the hospital. Still mentally sharp, she lamented that she was no longer able to play bridge and that her hearing had diminished. However, she continued to enjoy spending time with her family. Mrs. Dollinger died in March of 2014, at the age of 111. Her final words to her grandnephew were “I’ve had a very good life.”
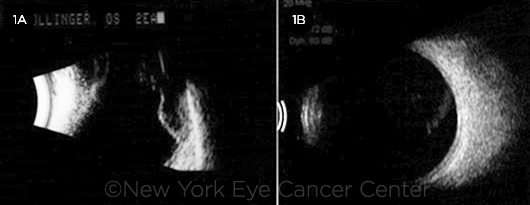
MELANOMA. Ultrasound imaging before (1A) and 9 years after (1B) treatment of Mrs. Dollinger’s choroidal melanoma.
Age Versus Treatment?
Uveal melanoma patients often ask about how their age affects their diagnosis and treatment. We tell them that the median age is 60 years and the incidence tends to drop off after 69.5 However, an increasing number of patients older than 90 years are presenting. When they ask if their advanced age will protect them from metastasis, we note that the answer is, unfortunately, no.1
Some patients also ask about their life expectancy. As a reference, the U.S. Census Bureau suggests that the average 92-year-old patient will live an additional 4.3 years and will most likely die from heart disease, cancer, or stroke.2
Cases like Mrs. Dollinger’s will likely become more prevalent as our population grows older, and we, as physicians, must be prepared. In this particular case, we had an autonomous, lucid, 92-year-old woman presenting with a life- and sight-threatening condition. She was treated with a safe intervention.
However, not all cases involving the oldest old will be as easily resolved. As technology enhances the way we take care of patients, more will be offered to extend the life of elderly patients; and with that in mind, we should try to individualize care. Mrs. Dollinger initially thought that her age precluded a fight to live longer. But with help, her life and the vision of what became her better functioning eye were preserved for 18 years, and she died of natural causes.
___________________________
1 Collaborative Ocular Melanoma Study Group. Arch Ophthalmol. 2006;124(12):1684-1693.
2 Retirement & Survivors Benefits Life Expectancy Calculator. Accessed Sept. 12, 2016.
___________________________
Dr. Finger is director of The New York Eye Cancer Center in New York City. Relevant financial disclosures: Dr. Finger’s research is supported in part by The Eye Cancer Foundation.
Dr. Sanvicente is a third-year ophthalmology resident at Hospital Banco de Olhos in Porto Alegre, Brazil. Relevant financial disclosures: None.
|
Ophthalmologists Get Older, Too
Patients are not the only ones who are aging—the Baby Boomer generation of ophthalmologists is growing older as well. And while many are slowing down in their practices, they are often not ready to fully retire.
In addition to focusing on the care of older patients, the Academy’s Committee on Aging is involved in the well-being of older ophthalmologists. Last month, at AAO 2016 in Chicago, the Committee on Aging and the Senior Ophthalmologist Committee held a session on exploring global opportunities for retiring ophthalmologists.
Cochaired by Drs. Sterns and Beaver, the session featured presentations on providing clinical care in underserved areas, especially countries that may not have access to technology. “Our senior ophthalmologists can bring their skills in conventional extracapsular cataract surgery to those areas that do not have access to modern phacoemulsification,” Dr. Beaver said.
Other areas of need for senior ophthalmologists include teaching residents the “lost art” of refracting and becoming involved in the growing field of telemedicine. “Our physicians are working longer and are in better health,” Dr. Sterns said. “They want to stay involved, and this is the ideal way to use the knowledge they gained in the early years of their practice. It’s a way to give back.”
|
Meet the Experts
Hilary A. Beaver, MD Associate professor of clinical ophthalmology at Weill Cornell Medical College in New York and associate clinical member at Houston Methodist Hospital’s Research Institute in Houston. Relevant financial disclosures: None.
Neil M. Bressler, MD The James P. Gills Professor of Ophthalmology and chief of the Retina Division at the Wilmer Eye Institute in Baltimore and editor of JAMA Ophthalmology. Relevant financial disclosures: Bayer: S; Genentech/Roche: S; Novartis: S; Regeneron: S.
Bradley J. Katz, MD, PhD Professor of ophthalmology & visual sciences and adjunct professor of neurology at the University of Utah in Salt Lake City. Relevant financial disclosures: None.
Michael S. Lee, MD Director of the ophthalmology residency program, professor and director of neuro-ophthalmology, and Mackall-Scheie Research Chair in Ophthalmology; professor of neurology; and professor of neurosurgery at the University of Minnesota in Minneapolis. Relevant financial disclosures: Neuro-Ophthalmix: O,P; Quark Pharmaceuticals: S.
Gwen K. Sterns, MD Chair of ophthalmology at Rochester General Hospital, clinical professor of ophthalmology at the University of Rochester Medical School, and medical director of the Association for the Blind and Visually Impaired-Goodwill in Rochester, N.Y.; a member of Prevent Blindness Scientific Committee; and a member of the Academy’s Senior Ophthalmologist Committee. Relevant financial disclosures: None.
Charles C. Wykoff, MD, PhD Codirector of clinical research at Retina Consultants of Houston, vice-president of the Greater Houston Retina Research Foundation, Deputy Chair for Ophthalmology at Houston Methodist Hospital’s Blanton Eye Institute, and assistant clinical member of Houston Methodist Hospital’s Research Institute; assistant professor of clinical ophthalmology at Weill Cornell Medical College in New York. Relevant financial disclosures: None.
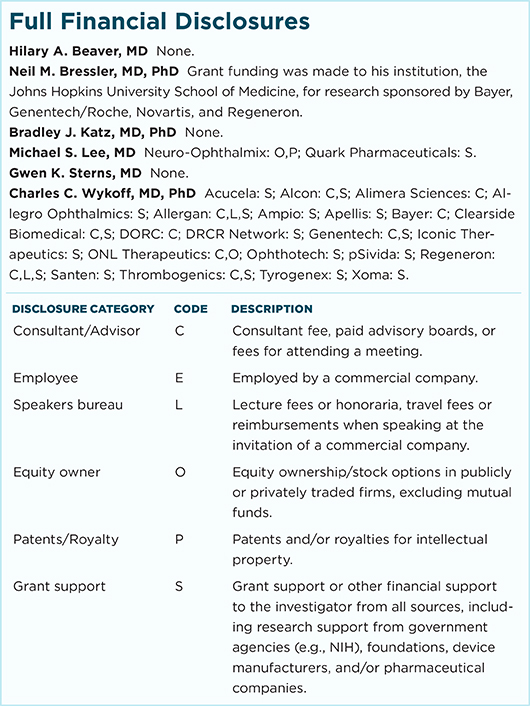
For full disclosures and the disclosure key, see below.
|
Photo Credits
(Page numbers refer to print edition.)
Page 48. This image was originally published in the ASRS Retina Image Bank. Christopher T. Cessna, DO, and Denise Miller, RD. Pigment Epithelial Detachment With Rip. Retina Image Bank. 2013; Image Number 9825. © The American Society of Retina Specialists.
Page 49. This image was originally published in the ASRS Retina Image Bank. Homayoun Tabandeh, MD. Anterior Ischemic Optic Neuropathy and Choroidal Ischemia. Retina Image Bank. 2014; Image Number 14624. © The American Society of Retina Specialists.
Page 50. This image was originally published in the ASRS Retina Image Bank. Henry J. Kaplan, MD, and Niloofar Piri, MD. Optic Atrophy. Retina Image Bank. 2013; Image Number 6269. © The American Society of Retina Specialists.
|