Artificial Intelligence Predicts Visual Outcomes in Neovascular AMD
By Jean Shaw
Selected By: Andrew P. Schachat, MD
Journal Highlights
Ophthalmology Retina, January 2018
Download PDF
Schmidt-Erfurth et al. set out to evaluate the ability of machine learning to predict functional outcomes in patients treated with ranibizumab for neovascular age-related macular degeneration (AMD).
They found that, according to their artificial intelligence (AI) algorithms, best-corrected visual acuity (BCVA) at month 3 was the strongest predictive factor of functional outcomes at the 1-year mark. In addition, they found that currently used morphological features were of limited value in predicting BCVA outcome.
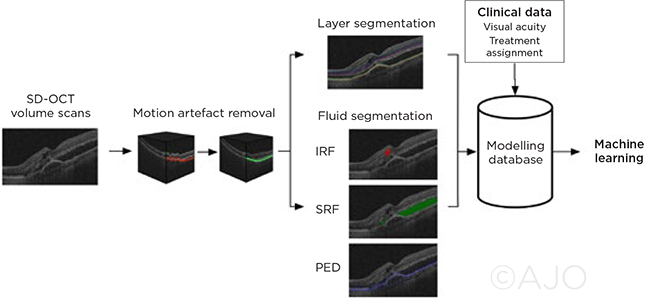 |
MACHINE LEARNING. This diagram of the computational image analysis image pipeline illustrates the steps in data assessment. IRF = intraretinal fluid; SRF = subretinal fluid; PED = pigment epithelial detachment.
|
For this post hoc analysis of a clinical trial database, the researchers evaluated data from 614 patients who participated in the HARBOR trial. (During HARBOR, patients received intravitreal injections of ranibizumab monthly or on a pro re nata basis for 12 months; in addition, they were evaluated monthly via spectral-domain optical coherence tomography [SD-OCT] imaging.) The researchers used AI algorithms to first correlate OCT parameters observed at baseline to the corresponding visual function at months 1, 2, and 3 and then to predict the patients’ final BCVA at 1 year.
They found that the correlation between predicted and final 12-month BCVA scores was loose at baseline—but by month 3, individual BCVA levels reached a solid predictive power for month 12.
However, fluid-based morphological features proved to be largely irrelevant for predicting therapeutic response, the researchers said.
The latter finding implies that classic exudative features—such as fluid within and underneath the retina—may be of limited value in explaining visual function in wet AMD and in providing individual patients with a visual prognosis, the authors said, and they added that this should prompt researchers to search for additional markers, such as a disruption of the external limiting membrane.
The original article can be found here.