Download PDF
The first retrospective review of its kind suggests that patients may safely continue novel oral anticoagulants (NOACs) during vitreoretinal surgeries—procedures that carry inherent risk for hemorrhagic complications.1 “Regardless, every situation requires individualization and careful consideration of the patient’s medical history and overall health,” said coauthor Harpreet S. Walia, MD, who is a vitreoretinal surgeon with Georgia Retina in Atlanta.
Benefits and indications. Dr. Walia and lead author M. Gilbert Grand, MD, evaluated the effects of 4 NOACs—rivaroxaban (Xarelto), apixaban (Eliquis), dabigatran (Pradaxa), and prasugrel (Effient)—which offer several benefits over older types of antithrombotics, including a rapid onset of action, few drug interactions, and no need for routine coagulation monitoring. Over time, vitreoretinal surgeons are likely to encounter increasing numbers of patients taking these drugs.
In the study, the NOACs were used most often to prevent thromboembolism after angioplasty (57.6%), followed by reduction of stroke risk and systemic embolism in patients with nonvalvular atrial fibrillation (36.4%). Other patients were on the drugs for recurrent deep vein thrombosis (DVT) or for DVT prophylaxis after hip surgery.
Comparable hemorrhage rates. The researchers compared 36 eyes of 33 patients on 1 of the 4 NOACs against 65 control eyes, all of which underwent vitreoretinal surgery at the Retina Institute in St. Louis from 2012 to 2015. Performed mostly under local regional anesthesia, the procedures included 3-port, 23-gauge pars plana vitrectomy, scleral buckling, or a combination of both. Patients were followed postoperatively for a minimum of 3 months.
No eyes in either group experienced perioperative complications of retrobulbar, suprachoroidal, or subretinal hemorrhage, said Dr. Walia. Four eyes in the NOACs group experienced postoperative vitreous cavity hemorrhage: 2 of them required additional surgery for retinal detachment, and 2 resolved without intervention. In the control group, 6 eyes experienced postoperative vitreous cavity hemorrhage, of which 4 required reoperation. There was no significant difference between the groups in rate of hemorrhage.
“Although we were pleasantly surprised by the results,” said Dr. Walia, “these results are consistent with those described in the literature for other antithrombotics such as warfarin, aspirin, and clopidogrel.”
Further Reading
Ophthalmologists in other subspecialties must also grapple with the question of NOAC use. For a discussion of considerations in oculoplastic surgery, see “Perioperative Management of Antithrombotics,” EyeNet, April 2016.
|
Caveats. Dr. Walia emphasized the need to confer with the patient and prescribing physician about the seriousness of the patient’s thrombogenic condition as well as the nature of the ophthalmic condition and imminent surgery. For example, stopping anticoagulants for elective surgeries, such as cataract or epiretinal membrane, may be more practical than for emergency surgeries such as retinal detachment or endophthalmitis, he said. “In cases like these, we don’t have the luxury to stop these drugs prior to surgery.”
Ophthalmologists have not yet reached consensus on this issue, said Dr. Walia. However, he said, when combined with other data—including metadata comparing NOACs and other antithrombotics—results from this study show that the visual risks of continuing NOACs during vitreoretinal surgery are low, especially when compared with the risks of discontinuation.
—Annie Stuart
___________________________
1 Grand MG, Walia HS. Retina. 2016;36(2):299-304.
___________________________
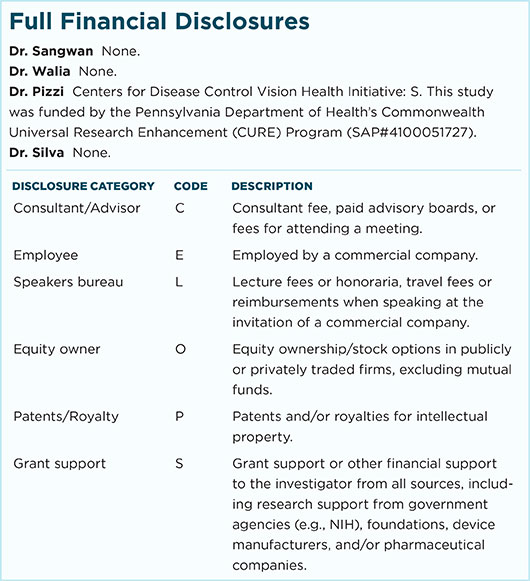
Relevant financial disclosures—Dr. Walia: None.
For full disclosures and disclosure key, see below.
More from this month’s News in Review