By Shaheen C. Kavoussi, MD, Maxwell Elia, MD, Eric Baylin, MD, Flora Levin, MD, and J. Javier Servat, MD
Edited by Sharon Fekrat, MD, and Ingrid U. Scott, MD, MPH
Download PDF
Balloon catheter dilation, or dacryoplasty, of the nasolacrimal duct is performed mainly to relieve congenital nasolacrimal duct obstruction (NLDO) in patients for whom probing and irrigation has failed. The most common cause of congenital NLDO is the persistence of an embryonic membrane at the valve of Hasner at the distal nasolacrimal duct where it enters the nose under the inferior turbinate. Stenosis of the entire duct or a portion of the duct can also occur. In our experience, balloon dacryoplasty is an excellent, minimally invasive way to achieve lacrimal system patency in the appropriately selected patient with congenital NLDO.
Clinical Evaluation
Congenital NLDO presents a challenge to parents and physicians. Although the majority of cases resolve during the first year of life with conservative management consisting of massage and topical antibiotics, those that do not will need additional intervention.
What to look for. External examination of a child with suspected NLDO may reveal crusting of the eyelashes, copious mucopurulent discharge, and a medial canthal mass. In further evaluating the patient, the clinician should note the frequency and character of tearing. Constant mucopurulent discharge suggests complete NLDO, while intermittent discharge associated with an upper respiratory tract infection may suggest local, transient obstruction caused by swelling of the mucosa around the inferior turbinate.
Other conditions causing epiphora (molluscum contagiosum, epiblepharon, entropion, and congenital glaucoma) should be considered during the initial evaluation. Children with malformations of the head and face are particularly at risk for congenital NLDO. Other structural anomalies of the lacrimal system may accompany congenital NLDO, such as atresia or agenesis of the puncta or canaliculi, or the presence of accessory canaliculi or supernumerary ducts.
Blockage proximal to the lacrimal sac usually produces epiphora without mucus discharge, since there is no connection with the mucus-secreting cells of the lacrimal sac. In contrast, gentle digital pressure over the lacrimal sac may produce mucopurulent reflux through the puncta in cases of NLDO.
Testing for obstruction. The dye disappearance test is helpful in determining patency of the lacrimal system. The presence of fluorescein in the tear lake five minutes after instillation suggests obstruction. Comparing the amount of fluorescein in both eyes is especially useful in identifying unilateral obstruction.
Indications for Procedure
The two main indications for balloon dacryoplasty are failed probing and restenosis after silicone intubation. Although this procedure is typically performed in children older than 12 months, we occasionally perform it in younger children who have recurrent episodes of dacryocystitis. In our experience, the success rate of balloon dacryoplasty is higher in children who have only failed probing compared with those who have also failed silicone intubation.
 |
|
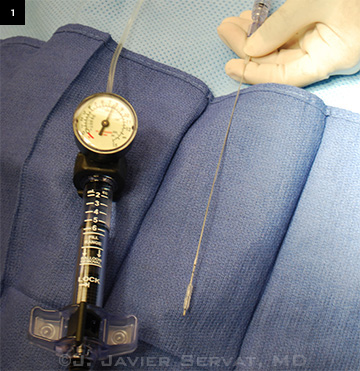
INSTRUMENTATION. The catheter is lubricated, and the system is primed with balanced salt solution.
|
Surgical Steps
The procedure is performed under general anesthesia. We do not use preoperative antibiotics (topical, oral, or intravenous). Intraoperatively, a single dose of intravenous dexamethasone (0.05 mg/kg) is given.
Probing. Both the superior and inferior puncta are dilated with a punctal dilator. The canaliculi are then probed using a size 0 Bowman probe that has been coated with lacrimal lubricant. The probe is passed through the superior canaliculus and the lacrimal sac toward the nose until further progress is prevented by a tight membrane; this blockage often can be both heard and felt. Further advancement breaks through into the nasal cavity. Next, a larger-gauge probe (size 3 or 4) is passed from the nostril into the nose to meet the first probe. The inferior canalicular system is probed in a similar manner.
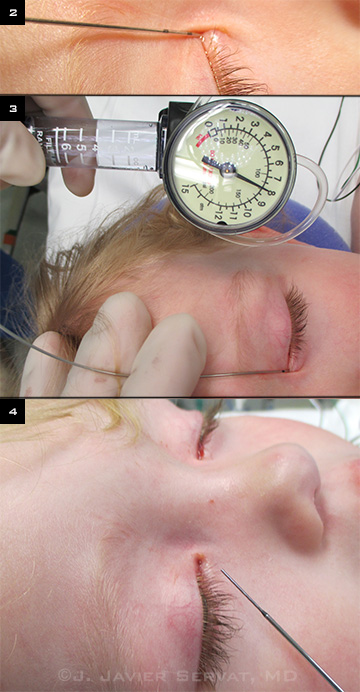
Catheter insertion. The size of the catheter depends on the patient’s age. We prefer to use a 3-mm lacrimal catheter in patients 2 years of age and older. The smaller 2-mm catheter is reserved for younger patients. The catheter system is primed with balanced salt solution (BSS), and the catheter is lubricated and inserted into the upper lacrimal system and advanced into the nose (Fig. 2). Once in place, it can be grasped via the nostril to test its position by gently rocking the catheter back and forth.
First-position inflation. Next, the surgeon notes the black measurement lines on the catheter and holds it steady at the 15-mm position while the manometer is inflated to 8 atmospheres (atm) of pressure (Fig. 3). This position places the balloon at the entry of the nasolacrimal duct into the nose at the level of the valve of Hasner. Inflation at this position is maintained for 90 seconds. While the balloon is inflated, the surgeon gently pulls on the tube to ensure that the catheter remains firmly in position. A slipping movement may represent balloon malfunction or leakage, and in such cases, the apparatus should be replaced. After 90 seconds, the balloon is deflated, then reinflated to 8 atm for 60 additional seconds, then deflated again.
Second-position inflation. Next, the catheter is retracted 5 mm, to align it at the level of the nasolacrimal duct. The same steps are repeated: Inflate the balloon to 8 atm for 90 seconds, deflate, inflate for 60 seconds, and deflate again.
Retraction. The catheter is then gently removed from the system by twisting in a counterclockwise manner while retracting. This twisting motion minimizes trauma to the surrounding outflow system. After catheter removal, the outflow system is irrigated with BSS (Fig. 4). We typically do not insert silicone tubes after our balloon dacryoplasty.
 |
|
SURGICAL STEPS. (2) The catheter is inserted into the upper lacrimal system, as the surgeon watches the black measurement lines (15 mm for the valve of Hasner and 10 mm for the lacrimal sac/duct junction). (3) The manometer is inflated to 8 atmospheres of pressure. (4) After catheter removal, the outflow system is irrigated with balanced salt solution.
|
Postoperative Considerations
Antibiotic/steroid (tobramycin/dexamethasone) drops are instilled into the eye at the end of the case and three times daily for one week postoperatively. The procedure is typically tolerated well without the need for oral pain medications postoperatively.
Balloon Dacryoplasty in Adults
Some investigators have used balloon dacryoplasty in combination with silicone intubation or as part of an endoscopic balloon-assisted dacryocystorhinostomy (DCR) in adults. When combined with silicone stenting, the balloon dilation procedure is similar to that described above. However, adding balloon dacryoplasty to endoscopic DCR in adults requires inserting a much larger catheter (9 mm) trans-nasally under endoscopic guidance to expand the nasal osteum. Long-term data supporting the additional benefit of balloon dilation in either procedure in adults are limited.
Key Points
Balloon catheter dilation is a valuable tool in the treatment of congenital NLDO. While probing alone has a high success rate, balloon dacryoplasty is a useful alternative in cases of failed probing, which is more likely to occur in children older than 19 months.1,2 Balloon dacryoplasty has similar efficacy to monocanalicular stenting in children with congenital NLDO.3 However, a major advantage of balloon dacryoplasty is that no silicone tube is left in the lacrimal system, eliminating any concern about the child removing or dislocating the tube.4
___________________________
1 Repka MX et al. Arch Ophthalmol. 2009;127(5):633-639.
2 Cha DS et al. Korean J Ophthalmol. 2010;24(5):261-266.
3 Goldstein SM et al. Ophthal Plast Reconstr Surg. 2004;20(5):352-357.
4 Maheshwari R. J Pediatr Ophthalmol Strabismus. 2009;46(4):215-217.
___________________________
Dr. Kavoussi and Dr. Elia are residents in ophthalmology, and Dr. Levin is an assistant professor of ophthalmology, at Yale University. Dr. Baylin and Dr. Servat are with Oculofacial Plastic Surgeons of Georgia. The authors report no related financial interests.