By Emily B. Worrall, BS, BA, and Hoon C. Jung, MD
Edited By: Ingrid U. Scott, MD, MPH, and Sharon Fekrat, MD
Download PDF
As the tools and techniques of cataract surgery continue to advance, there is increasing impetus to improve the outcomes of this already successful procedure. Quality of life and spectacle independence are being added to the traditional measures of success: safety, improved vision, short operating times, and absence of postoperative complications.
Today, numerous options for treatment and correction are available, with differing risks and benefits. More than ever, the optimal surgical techniques and intraocular lens (IOL) selection depend on the individual patient’s ocular pathology, anatomy, history, and visual needs.
The surgeon’s responsibility is to bring clinical experience and scientific evidence to bear on the discussion with the patient to arrive at realistic postsurgical visual goals and a clear rationale for IOL selection. Successful cataract surgery begins with agreement between the doctor and patient on these key points, well before the procedure.
Among the growing number of options that are intended to decrease spectacle dependence—including mono-vision, mini-monovision, accommodative IOLs, corneal inlays, and bioptic refinements—multifocal IOLs (MF-IOLs) continue to play an important role.
One approach to consider is mixing and matching different types of IOLs, including monofocal and multifocal lenses. Although such “blended vision” presents challenges, it provides an opportunity for success in selected cases.1
Earlier attempts at mixing and matching to achieve good blended vision were likely hampered by limited IOL options. Now, however, a wide array of designs and add powers has expanded the possibilities for refractive correction.
 |
|
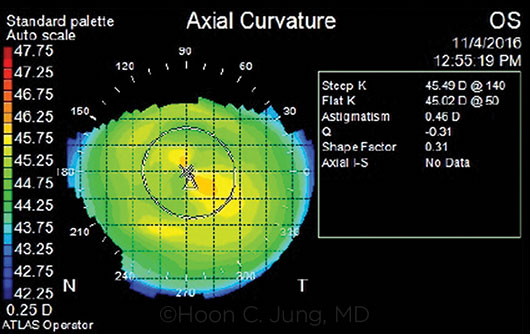
CORNEAL TOPOGRAPHY. Preoperative topography shows minimal astigmatism in the left eye of the patient described in the case example.
|
Patient and IOL Selection
The following considerations may help guide patient selection and IOL choice for successful refractive outcomes.
Corneal shape and power analysis. Screening for corneal irregularities using topography, tomography, or other advanced imaging is recommended in patients considering MF-IOL correction. In addition, careful attention to optical axes such as angle kappa can help decrease postoperative patient dissatisfaction.2
Role of eye dominance. If contemplating the use of monovision or blended vision with mixed IOLs, the surgeon should test for eye dominance. Targeting the nondominant eye for the nearer focal point should be considered.
Aberrations. Characterizing corneal aberrations is helpful when selecting IOLs. Eyes with highly aberrated corneas are not good candidates for MF-IOLs.
It is important to differentiate between aberrations related to the cornea itself and those generated by the entire optical system, including the influence of the lens and cataract. A hard contact lens trial may help determine the contribution of corneal aberrations to the patient’s decreased vision, although visual disturbances are often the result of the combined effects of the lens and cornea.
Analysis of corneal aberrations may guide the decision to implant a monofocal IOL with aspheric offsets (zero or negative) to neutralize spherical aberrations. An aspheric monofocal IOL may afford the best quality for distance vision in the dominant eye. However, it may be advantageous to preserve some spherical aberration in the nondominant eye by selecting a traditional nonaspheric IOL or other design matched with the individual cornea. This combination may increase depth of focus and thereby decrease spectacle dependence for near tasks.3
Tear film. The tear film should be assessed carefully. Tear deficiency or abnormalities can affect both preoperative analysis and postoperative patient satisfaction.
Macular status. Because even subtle maculopathy can impair the visual outcome with MF-IOLs, optical coherence tomography may be used to rule out any relevant macular conditions.
Comorbidities. MF-IOLs should not be placed in eyes with significant ophthalmic comorbidities such as retinopathy, corneal disease, uveitis, and optic neuropathy. This remains a fundamental tenet of cataract surgery.
Chromophores. Introduction of chromophores into IOLs to block certain wavelengths of the electromagnetic spectrum has had variable market penetrance, and the literature continues to weigh the risks and benefits.4
In cases of bilateral cataract surgery, implanting IOLs with different chromophores should be strictly avoided. If one eye is treated before the other, it is important to review the surgical record or IOL card to avoid implantation of a different chromophore IOL in the second eye; otherwise, the eyes will perceive color differently.
In addition, MF-IOLs redistribute energy to different areas of the retina, and chromophores that block specific wavelengths of light reduce the total energy transmitted through the optical system. Thus, patients seeking high visual performance in low-light conditions may not be ideal candidates for MF-IOLs with chromophores.
Blended Vision: Case Example
A 78-year-old man presented with blurry vision in his left eye. He had undergone cataract extraction 10 years earlier in his dominant right eye and received a +22.0 D SN6AD3 (Alcon) MF-IOL implant with a +4.0 D add. The patient reported general satisfaction with the right eye for distance vision; however, he was dissatisfied with intermediate and near vision in the right eye as well as the compromised vision at all ranges in the left eye. He requested cataract surgery and IOL implantation in his left eye to improve his ability to work on the computer, with the goal of achieving spectacle independence.
The patient’s uncorrected distance visual acuity (UCDVA) was 20/20-1 in the right eye and 20/60-1 in the left eye, with a best-corrected distance visual acuity of 20/40, with –0.75 + 1.25 × 140 manifest refraction. There were no other relevant ocular health issues. Corneal topography (Fig. 1) and biometry were obtained in preparation for cataract surgery in the left eye.
The surgeon and patient discussed the chance that spectacles could still play a role in achieving optimal visual acuity. Together, they decided on an MF-IOL with the base sphere targeted for emmetropia at distance and a lower- power reading add (+2.5 D) than in the right eye.
Uncomplicated surgery was performed in the left eye using topical anesthesia and a superior clear corneal approach. An SV25T0 (Alcon) MF-IOL with power of +21.0 D was implanted. Seven weeks postoperatively, the patient’s UCDVA was 20/15-2 with J1 vision with both eyes open at a comfortable reading distance. He achieved spectacle independence at near, intermediate, and distance vision, with improvement in activities of daily living.
|
Excimer Enhancements
Access to an excimer laser, either co-located or used in agreement with a nearby refractive center, will allow the surgeon to make bioptic refinements. This is helpful in enhancing correction for a known condition such as preoperative astigmatism and in addressing postoperative refractive ametropia. The option of possible laser correction should be discussed with the patient, and any necessary arrangements should be made, before cataract treatment.
Special Clinical Scenarios
Corneal refractive surgery. Cataract patients who have had previous corneal refractive surgery present a challenge. Given that keratorefractive procedures frequently increase corneal aberrations, the surgeon should exercise caution in using MF-IOLs in these individuals, especially those who had correction of large refractive errors.
Unilateral cataracts. Implantation of an MF-IOL for unilateral cataract has been an area of active debate.5 Unilateral cataracts are less common than bilateral and may justify extra screening for conditions such as amblyopia (e.g., in the setting of polar cataracts) and trauma, which can damage zonules. MF-IOLs should be avoided in eyes with zonular insufficiency, as decentration of the IOL can degrade visual performance significantly. Potential acuity meter testing or pinhole-assisted methods are useful for screening if amblyopia is a concern.
The fellow eye may not require cataract surgery for years or decades. Thus, the patient should be instructed on the importance of safeguarding the IOL identification from the first surgery in case of a later procedure.
Conclusion
MF-IOLs can play an important role in decreasing spectacle dependence, although traditional contraindications remain a limiting factor. Blending of near and intermediate add powers with MF-IOLs should be considered in appropriate candidates seeking the broadest range of vision.
___________________________
1 Bilbao-Calabuig R et al. J Refract Surg. 2016;32(10):659-663.
2 Tchah H et al. Int J Ophthalmol. 2017;10(2):241-245.
3 Zheleznyak L et al. Invest Ophthalmol Vis Sci. 2013;54(5):3157-3165.
4 Brøndsted AE et al. Acta Ophthalmol. 2017;95(4):344-351.
5 Hayashi K et al. J Cataract Refract Surg. 2013;39(6):851-858.
___________________________
Ms. Worrall is a third-year medical student at University of Washington School of Medicine, Seattle Foundations Site, in Seattle. Dr. Jung is assistant professor of ophthalmology at the University of Washington and VA Puget Sound Health Care System, in Seattle. Financial disclosures: None.