By Meron Haile, MD, and Rona Z. Silkiss, MD
Edited by Sharon Fekrat, MD, and Ingrid U. Scott, MD, MPH
Download PDF
Blepharochalasis syndrome was first described by G.J. Beer in an 1817 textbook and was named by Ernst Fuchs in 1896.1 It is a condition of the eyelids consisting of episodic inflammation and chronic skin changes. It is usually bilateral and tends to manifest in the upper eyelids, although unilateral cases as well as those affecting the lower eyelids exclusively have also been reported.
Little is known about the epidemiology of this disorder, as most of our current knowledge comes from published case reports. According to a review published in 2009, the average age of onset is around 11 years old.2 It is suspected that this condition occurs with similar frequency in males and females; however, more cases have been reported in females to date.
Etiology
There are multiple theories regarding the etiology of blepharochalasis. Unlike dermatochalasis, which is often the competing diagnosis and is an involutional change to the eyelid skin, blepharochalasis is thought to be a manifestation of angioneurotic edema. Puberty and hormonal changes may play a modulatory role in the disease. Attacks have also been reported to follow bee stings, crying, physical activity, wind exposure, or stressful events.2 In most cases, however, no trigger can be identified.
Pathologic findings. Case reports involving histologic examination of eyelid tissue have suggested that lymphocytic infiltration of the dermis and loss of elastic fibers might be characteristic findings. Loss of collagen in the dermis has also been reported, and the size and number of capillaries may be increased.
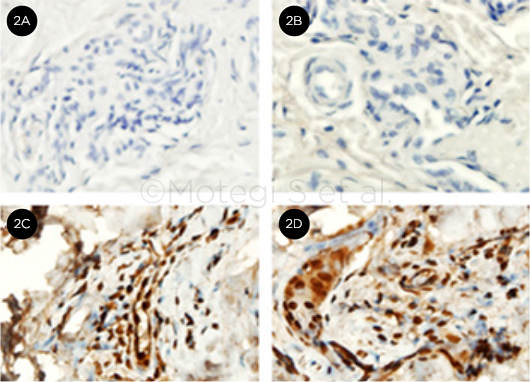
Immunohistochemical analysis of excised eyelid skin was also positive for matrix metalloproteinases (MMP)-3 and -9 in one study.3 Another study demonstrated the presence of IgA around atrophic elastic fibers.4 These findings suggest that there may be a concomitant inflammatory process accompanying the extravasation of fluid and localized edema occurring at the capillary level.
Systemic associations. No clear systemic associations are known. However, a link has been suggested to Ascher syndrome. In that rare condition, the upper eyelids and lips become swollen, sometimes in conjunction with euthyroid goiter.
 |
|
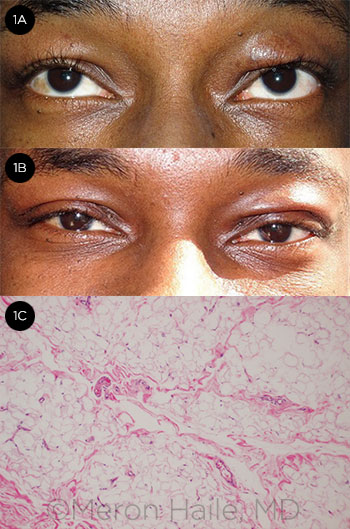
BEFORE AND AFTER. (1A) 26-year-old man with blepharochalasis. Bronze deposits are present bilaterally on the upper eyelids, accompanied by asymmetric swelling. (1B) Same patient 1 week after bilateral upper blepharoplasty. (1C) H&E stain of right upper eyelid tissue excised during the procedure. There is no evidence of active inflammation, which may indicate disease quiescence and ideal timing for surgery.
|
Signs and Symptoms
Patients will often complain of episodic, painless eyelid swelling. Erythema is sometimes present. Flares usually last 2 to 3 days and may occur several times a year. The frequency of attacks typically dwindles as the patient ages, with the peak of disease activity occurring in the teenage years. The skin stretches and becomes atrophic over time, sometimes within less than a decade after onset of the disease. This often makes young patients appear much older than their actual age.
Classic findings on physical examination include “cigarette paper” skin that appears thin and finely wrinkled, edema (which may be asymmetric), bronze deposits, subcutaneous telangiectasia, lid laxity and malposition (including entropion and ectropion), proptosis, orbital fat and lacrimal gland prolapse, and a pseudoepicanthal fold. Firm palpation of the affected eyelid generally does not cause pitting.
Staging. Stages of this disease have been described, and the presence or absence of some aforementioned findings may help differentiate among these stages. During the earlier active phase, nonpitting edema of the eyelids is most prominent. This phase may be further subdivided into hypertrophic and atrophic variants. In the hypertrophic variant, weakness of the orbital septum allows orbital fat to prolapse forward, giving the orbit a fuller appearance. In the atrophic variant, the globes may appear more hollow due to fat atrophy. During the late phase, the lids become lax and thin; and the disease may be called quiescent when no flares have occurred for 2 or more years.1
Differential Diagnosis
Blepharochalasis can easily be mistaken for dermatochalasis. The important distinguishing features of blepharochalasis include subcutaneous telangiectasia, episodic edema, and cigarette paper skin, which are absent in dermatochalasis. Also, in contrast to patients with blepharochalasis, who generally begin to have symptoms in childhood or adolescence, patients with dermatochalasis usually note eyelid laxity beginning at around the fourth decade.
Other diagnoses to consider include floppy eyelid syndrome (especially in overweight males with obstructive sleep apnea), thyroid eye disease, orbital inflammatory disease, dacryoadenitis, hereditary angioedema, and lacrimal gland tumor. Contact dermatitis should be considered when erythema is coupled with pruritus, as the latter is not usually associated with blepharochalasis.
 |
|
IMMUNOHISTOCHEMISTRY. IHC analysis is negative for IgG (2A) and MMP-2 (2B), but shows positive staining for MMP-3 (2C) and MMP-9 (2D).
|
Diagnosis
Blepharochalasis is a clinical diagnosis based on history and examination findings. No diagnostic laboratory tests are currently available. Serum C1 inhibitor levels and activity may be checked in order to differentiate between blepharochalasis and hereditary angioedema, as these levels should be low in the latter but not the former.2 Although biopsies of eyelid skin to look for the aforementioned histologic and immunohistochemical findings may be helpful in establishing a diagnosis, they are not part of any diagnostic criteria; moreover, biopsied tissue may appear normal in some patients.
Complications
Eyelid skin laxity; ptosis, usually secondary to levator dehiscence but with preserved levator function; herniation of the orbital lobe of the lacrimal gland; prominent eyelid vascularity; and orbital fat pad atrophy have been reported.1
Treatment
There are no standardized treatment protocols for blepharochalasis.
Medical. Systemic and topical steroids, antihistamines, and anti-inflammatory medications do not appear to be effective in treating flares or in changing the overall course of the disease. Some case reports have suggested that oral doxycycline or oral acetazolamide combined with topical hydrocortisone may be promising options, but these drugs have not yet been studied in clinical trials as treatments for blepharochalasis.5,6
Surgical. Surgical options for the complications discussed above include blepharoplasty, levator aponeurosis dehiscence repair, eyelid tightening, canthal tendon reattachment, and fat grafting. Surgeons should be conservative when excising prolapsed orbital fat, given that fat atrophy is part of the natural history of this disease.
It is also important to note that ptosis repair in these patients tends to yield a high rate of overcorrection. Therefore, the surgeon caring for a blepharochalasis patient may consider undercorrection in his or her surgical approach and plan. If lateral canthal tendon laxity requiring repair is present, it should be corrected before the ptosis is repaired, as there is a risk of “temporal peaking” when the aponeurosis is advanced.2
Prognosis
Because surgical interventions cannot address the underlying pathophysiology of the disease, many of the complications such as ptosis and drooping eyelid skin may recur after surgical correction. This is especially the case if patients had surgery before the disease became quiescent.7
Some case reports have documented recurrence of ptosis after only a few years in patients who underwent surgical correction early in their second decade. It is recommended that surgeons defer these interventions until the patient has been free of flares for 6 months to a year.1,2 These patients should be counseled appropriately so that they understand the limitations of surgery and the potential need for additional surgeries in the future.
___________________________
1 Kotlus BS et al. Blepharochalasis syndrome. Accessed July 8, 2016.
2 Koursh DM et al. Surv Ophthalmol. 2009;54(2):235-244.
3 Motegi S et al. J Dermatol. 2014;41(6):536-538.
4 Grasseger A et al. Br J Dermatol. 1996;135(5):791-795.
5 Karaconji T et al. Ophthal Plast Reconstr Surg. 2012;28(3):e76-78.
6 Lazaridou MN et al. Clin Ophthalmol. 2007;1(3):331-333.
7 BCSC Section 7: Orbit, Eyelids, and Lacrimal System. San Francisco: AAO; 2014.
___________________________
Dr. Haile is an ophthalmology resident, and Dr. Silkiss is chief of oculoplastics; both are at California Pacific Medical Center, San Francisco. Relevant financial disclosures: None.