Download PDF
The Boston Type I Keratoprosthesis (BI-KPro) is an artificial cornea device. It is implanted as a treatment for many severe, recalcitrant corneal disorders that are not amenable to traditional corneal transplantation such as penetrating keratoplasty (PK). Although the device was initially rejected by ophthalmologists because of its high rate of complications, modifications to the mechanical design, as well as the development of antibiotic prophylaxis regimens and large-diameter bandage contact lenses, have allowed the BI-KPro to become a viable option for preserving or restoring vision.
The BI-KPro was first developed by Claes H. Dohlman, MD, PhD, at the Massachusetts Eye and Ear Infirmary in the 1960s, but it was not approved by the U.S. Food and Drug Administration until 1992.1 Since its approval, the BI-KPro has become more widely adopted in the United States and globally and is now considered a standard of care for the treatment of many otherwise blinding corneal diseases.
The Boston KPro is available in 2 variants, Type I and Type II, both of which contain an optic, as well as a front plate and a back plate, between which a donor corneal graft is placed. Type I is much more commonly used, as its implantation procedure more closely resembles PK surgery. It is available in both adult and pediatric sizes.
In contrast, Type II implantation surgery requires permanent tarsorrhaphy, with the anterior nub of the device protruding through the eyelid.2 The Type II KPro is used only for end-stage conditions such as severe chemical burns and ocular cicatricial pemphigoid. The limited clinical indications and the need for specialty training to implant and manage it postoperatively account for its less frequent use compared with the Type I device.2,3
Modifications
The design of the BI-KPro has been modified since its approval to reduce complications. In 1996, 8 holes were added to the back plate, allowing nutrients from the aqueous to flow through to support the health of donor graft stroma and keratocytes2; the current design features 16 holes in the adult size. In 2004, a titanium locking C-ring was added to reduce the incidence of intraocular disassembly of the device.2 In 2007, the design was once again improved by replacing the threaded screws with a threadless design, simplifying assembly and minimizing damage to donor epithelium.2 More recently, the material of the back plate was changed to titanium to reduce the risk of retroprosthetic membrane (RPM) formation and keratolysis.2 The current model of the BI-KPro utilizes a click-on mechanism to secure the donor cornea between the front plate and the back plate.
In addition, an adjunctive therapy—the indefinite use of large-diameter bandage contact lenses (BCLs) after implantation—has helped to reduce the incidence of ocular surface problems and to increase patient comfort. BCLs may be tinted to match the patient’s iris color and obscure the view of the back plate.
These improvements have contributed substantially to the increased utilization of the BI-KPro since 2002, when fewer than 50 procedures had been performed. By 2009, 1,161 procedures had been done; and, by 2014, at least 9,000 BI-KPro devices had been implanted worldwide.2
Indications
Initially, the Boston KPro was indicated for patients requiring PK following a previous corneal graft failure. The indications have been expanded and now include, but are not limited to, ocular trauma, herpetic keratitis, limbal stem cell deficiency, aniridia, Stevens-Johnson syndrome, silicone oil keratopathy, and congenital corneal opacification.2 These indications encompass conditions in which traditional PK is likely to fail owing to infectious, inflammatory, or neovascular causes.
Implantation Procedure
Assembly. BI-KPro implantation involves incorporating the KPro into the host’s cornea by suturing a donor cornea/KPro complex into the host corneal rim. First, the prosthetic device must be assembled. Using a trephine, the surgeon punches a hole in the donor corneal graft, allowing the graft to be slid over the KPro. Next, the back plate is placed in position, and the system is secured by the titanium snap ring.
Insertion. The patient’s eye is then prepared for insertion of the prosthesis. The cornea is trephinated with a radius slightly smaller than that of the assembled prosthesis. Bleeding vessels are cauterized before the corneal button is completely removed. Vitrectomy should be performed if the vitreous is exposed, and the lens may be removed in phakic patients. The prosthesis is then placed into the opening created in the patient’s cornea and secured with 16 10-0 or 12 9-0 nylon sutures.4
Long-term care. Patients require ongoing care, including lifelong prophylactic use of topical antibiotics and, in many cases, topical steroids.
Patients should be cautioned to contact their physician immediately if they experience any change in vision, eye pain, red eye, loss of peripheral vision, or light sensitivity.
Outcomes
A retrospective chart review of 75 BI-KPro procedures reported that most patients (95%) who received the device experienced visual improvement in the first 6 months, with 28 (37.3%) achieving full functional vision, defined as Snellen acuity ≥20/40.5 In fact, another study reported that some patients attained at least a short-term recovery of 20/20 vision.2
A critical requirement for maintaining a good visual outcome is device retention, which was reported to be greater than 90% over 5 years, regardless of the original indication for KPro implantation.5 In the late postoperative period, there was mild to severe loss of best-corrected visual acuity in a significant proportion of patients because of complications related to the BI-KPro. One-third of patients experienced severe vision loss over the long term as a result of device extrusion or vitreoretinal or optic nerve complications.5
Common Complications of Boston Type I Keratoprosthesis
|
| KPro Complications |
Management |
| Retroprosthetic membrane |
Topical steroid or Nd:YAG laser membranotomy; surgical membrane removal if necessary |
| Glaucoma |
Glaucoma medication ± drainage device insertion |
| Infectious endophthalmitis |
Intravitreal antibiotic injections ± pars plana vitrectomy |
| Sterile vitritis |
Peribulbar steroid injection + topical steroid |
| Corneal melting (keratolysis) |
KPro replacement or full-thickness graft |
Complications and Their Management
Advances in postoperative care, coupled with mechanical improvements in the device, have helped to reduce severe complications that limited the early adoption of the BI-KPro. However, some serious issues remain. RPMs and elevated intraocular pressure (IOP) constitute the most common anterior segment complications, while endophthalmitis and vitritis account for the majority of posterior segment complications.2
RPMs. Many studies have found the most common postoperative complication in both Types I and II keratoprosthesis surgery to be the formation of RPMs.3 Treatment for RPM includes increased topical steroid administration, Nd:YAG laser membranotomy, and—if those measures fail—surgical removal of the membrane.2
Glaucoma. Lee et al. found glaucoma to be the second most commonly reported postoperative complication.2 The rigidity of the KPro front plate limits the ability of physicians to measure IOP via applanation tonometry.1 Thus, they have relied on finger palpation, an inaccurate method that has prompted investigations into other, more objective methods of measuring IOP.1 Glaucoma medication may be prescribed to reduce IOP.5 A glaucoma drainage device may also be inserted at the time of BI-KPro implantation or postoperatively in an attempt to prevent the development of glaucoma in patients who had not been diagnosed with it preoperatively.3
Endophthalmitis. Infectious endophthalmitis, a devastating complication, occurs at a higher rate with keratoprosthesis implantation than with other ocular surgeries; Goins et al. reported a long-term rate of 9.3%.5 It is treated with intravitreal antibiotic injections, but some patients may require pars plana vitrectomy as well.2
Vitritis. Postoperative sterile vitritis is a major concern, as it causes rapid deterioration of visual acuity. It is treated with peribulbar steroid injection followed by topical steroid application.2
Corneal melting. Although the incidence of postoperative corneal melt (keratolysis) has decreased since the introduction of back-plate fenestrations to allow nutrient circulation, it remains one of the most common causes of device extrusion and loss.2,6
The prophylactic use of oral tetracyclines has been shown to be insufficient in preventing corneal melt.6 Once corneal melting has been diagnosed, the definitive treatment options are limited to KPro replacement or exchange for a full-thickness graft.6
Other medications, such as prostaglandin analogues, angiotensin-converting enzyme (ACE) inhibitors, and statins, have been considered in the treatment of corneal melt. However, there is currently not enough evidence to determine their efficacy.6
Conclusion
The BI-KPro has been shown to offer many patients with corneal blindness the possibility of a life-changing recovery in visual acuity. Ongoing advances in technology and materials are expected to further improve efficacy and safety. However, lifelong follow-up of the patient is critical to monitor for complications and preserve visual gains.
___________________________
1 Salvador-Culla B, Kolovou PE. J Funct Biomater. 2016;7(2):1-11.
2 Lee WB et al. Ophthalmology. 2015;122(7):1404-1511.
3 Lee RZ et al. Ophthalmology. 2017;124(1):27-35.
4 Dohlman CH et al. Expert Rev Ophthalmol. 2006;1(1):41-48.
5 Goins KM et al. Cornea. 2016;35(9):1165-1174.
6 Bouhout S et al. Ocul Immunol Inflamm. Published online Jan. 12, 2017.
___________________________
Mr. Goel is a medical student at University of Southern California (USC) Keck School of Medicine, Los Angeles. Dr. Hemmati is adjunct assistant clinical professor of ophthalmology, at the Roski Eye Institute, USC Keck School of Medicine. Relevant financial disclosures: None.
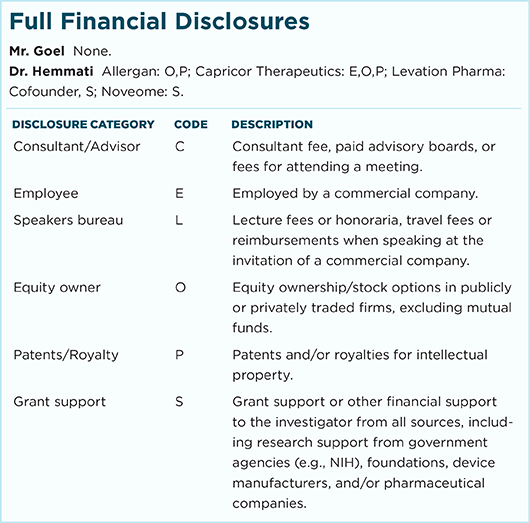
For full disclosures and the disclosure key, see below.