Download PDF
Make your diagnosis in the comments, and look for the answer in next month’s Blink.
Last Month’s Blink
Bilateral Acute Macular Neuroretinopathy
Written by Joana Roque, MD, Susana Henriques, MD, and Graça Pires, MD. Photo by Joana Roque, MD. All are at Hospital Prof. Doutor Fernando Fonseca, Lisbon, Portugal.
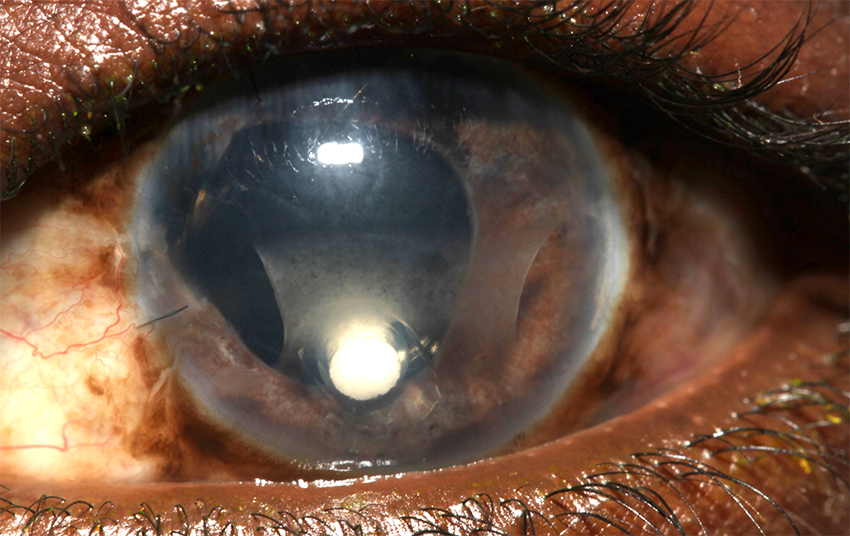
A healthy 17-year-old boy presented with a two-day history of bilateral paracentral “shadows” in his vision, which appeared five days after a flulike illness. Although his visual acuity was preserved bilaterally (20/20), Amsler grid testing confirmed the presence of several bilateral paracentral scotomas.
At presentation, fundus examination showed discrete pigmented perifoveal lesions, associated with perifoveal areas of hyperreflective and thickened outer nuclear layer (ONL) as seen on spectral-domain optical coherence tomography (SD-OCT). These findings, together with his previous illness, suggested a diagnosis of acute macular neuroretinopathy (AMN). A nasopharyngeal swab was positive for influenza type B, a common condition associated with AMN. He also had coexisting Streptococcus group A pharyngitis, which has not been linked to AMN.
Within two weeks, the lesions became more evident, particularly on infrared reflectance (IR) imaging. IR images show dark petaloid perifoveal lesions typical of AMN (Figs. 1A, 2A), corresponding to areas of thickened ONL and focal disruption of ellipsoid and interdigitation zones on SD-OCT (arrows, Figs. 1B, 2B).
At the four-month follow-up, the patient still had visual complaints, and there were areas of outer retinal thinning on SD-OCT.
About AMN
AMN is a rare condition characterized by the sudden onset of one or more paracentral scotomas. A flulike illness precedes the development of AMN in a significant proportion of cases. However, the pathophysiology remains unclear, and numerous other associations have been identified. At presentation, fundus examination may not be sufficient for diagnosis. SD-OCT and, especially, IR imaging have greater accuracy in detecting the typical retinal lesions.
___________________________
Further Reading: See “The Case of a High School Graduate With a New Blind Spot” (Morning Rounds, October 2019).
Read your colleagues’ discussion.
| BLINK SUBMISSIONS: Send us your ophthalmic image and its explanation in 150-250 words. E-mail to eyenet@aao.org, fax to 415-561-8575, or mail to EyeNet Magazine, 655 Beach Street, San Francisco, CA 94109. Please note that EyeNet reserves the right to edit Blink submissions. |