Download PDF
At age 83, Mae Morris* was happy with her intraocular lenses (IOLs), which were implanted during 2 uncomplicated cataract surgeries performed when she was in her mid-70s. One day, however, she suddenly noticed a gray “curtain” obstructing the vision in her right eye. She consulted her optometrist, who diagnosed retinal hemorrhages and referred her to our medical retina clinic.
We Get a Look
Mrs. Morris’ best-corrected visual acuity was 20/25 in both eyes, and she had no afferent pupillary defects. Her ocular motility was full and symmetric, and the confrontation visual fields were similarly full, but Mrs. Morris told us that she noted a graying of her vision inferotemporally in her right eye. Her intraocular pressure was 17 mm Hg in both eyes.
The slit-lamp exam showed no conjunctival injection and only rare anterior chamber cells in the right eye. The irides were normal without rubeosis, transillumination defects, or nodules.
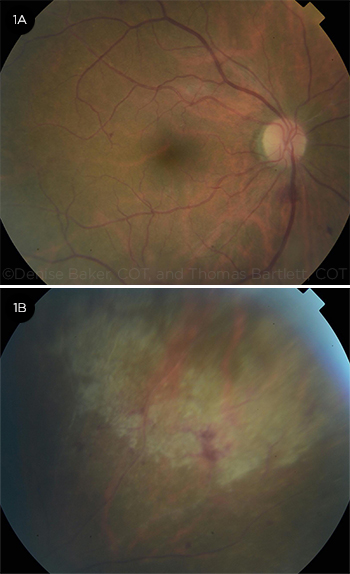
The dilated funduscopic exam of Mrs. Morris’ right eye showed mild vitreous cell and haze, a normal optic disc, scattered retinal hemorrhages, and a focal area of retinal whitening in the posterior pole (Fig. 1A). We also observed a focal area of hemorrhagic retinitis in the superonasal midperiphery without retinal breaks (Fig. 1B). The dilated exam of her left eye showed a clear vitreous, a normal optic nerve, and normal vessels. There was a small, old chorioretinal scar located superiorly in her left eye, but we did not identify any hemorrhages, retinitis, or retinal breaks. Optical coherence tomography of the macula was normal in both eyes.
 |
|
INITIAL EVALUATION. Fundus photos of the right eye showed a small white lesion superior to the fovea and a few posterior pole hemorrhages (1A) and a focal area of hemorrhagic retinitis superonasally (1B).
|
Pinning It Down
Differential diagnosis. The differential included atypical vascular occlusion, infectious retinitis, and acute retinal necrosis (ARN). We also considered cytomegalovirus (CMV) retinitis, HIV retinopathy, and syphilis. We discussed these possibilities with Mrs. Morris, who reported no recent travel, new sexual partners, or other significant life changes. She did have a long history of rheumatoid arthritis (RA) and was on regular anti-inflammatory therapy, which included 7.5 mg of oral prednisone each day and 10 mg of oral methotrexate once a week.
Mrs. Morris told us that she had previously received anti–tumor necrosis factor alpha (TNF-α) agents, including injections of etanercept (Enbrel) and intravenous (IV) infusions of infliximab (Remicade) for her RA. Because these drugs were not particularly helpful at controlling her symptoms, she was given a short trial of oral tofacitinib citrate (Xeljanz). This medication was started 3 months before she presented and stopped 1 month later (that is, 2 months prior to presentation), due to gastrointestinal side effects.
Because of the possibility of ARN, we performed a diagnostic anterior chamber paracentesis of Mrs. Morris’ right eye. We sent the aqueous fluid to be evaluated for herpes simplex virus 1 and 2 (HSV-1, -2), varicella-zoster virus (VZV), and CMV. We administered ganciclovir (Cytovene) 2 mg/0.1 mL into her right eye via intravitreal injection, and we asked Mrs. Morris to return the next day so that we could determine the appropriate systemic antiviral therapy.
The aqueous results confirmed that Mrs. Morris had CMV.
Clinical Course
The next day, when Mrs. Morris returned for follow-up, she was admitted to the hospital. She was given IV valganciclovir (Valcyte), and the oral prednisone and oral methotrexate were discontinued. The laboratory workup included a complete blood count (CBC), which showed mild leukopenia; the Western blot test for HIV, which was negative; and a blood test for CMV DNA, which was detectable at a low level (<137 IU/mL). Mrs. Morris then received an intravitreal injection of foscarnet (Foscavir) 2.4 mg/0.1 mL into her right eye.
Over the next few days, Mrs. Morris continued to receive IV valganciclovir twice a day on an inpatient basis. She was then discharged from the hospital and transitioned to twice-daily outpatient IV valganciclovir infusions. She had eye examinations every 3 to 4 days and received alternating intravitreal injections of ganciclovir 2 mg/0.1 mL and foscarnet 2.4 mg/0.1 mL. (One of these medications was injected every 3 to 4 days, but the same medication was injected only once a week.)
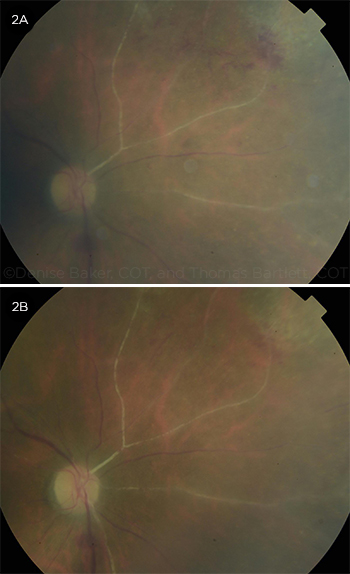
After 3 weeks of treatment, Mrs. Morris’ retinitis was improving (Fig. 2A), her serum CMV level became undetectable, and she was transitioned to oral valganciclovir. She developed some anterior chamber and vitreous cells as her immune system responded to the intravitreal and systemic antiviral therapy. (This mild inflammatory response was also related to immune recovery, as her oral prednisone and oral methotrexate had been discontinued 3 weeks prior.) A topical steroid eye drop (prednisolone acetate) was used cautiously for the relative immune recovery uveitis, and she was subsequently switched to the more potent difluprednate (Durezol) for the uveitis.
Mrs. Morris was restarted on a low dose (5 mg) of oral prednisone for her RA, and she has been monitored carefully since then. She continues to require difluprednate drops for the mild immune recovery uveitis in her right eye. The visual field defect persists in the right eye, but Mrs. Morris’ RA and eyes are stable (Fig. 2B).
 |
|
IMPROVING. After 3 weeks, early vascular sclerosis and improved focal retinitis were evident (2A). Follow-up imaging showed more extensive vascular sclerosis but healed retinitis (2B).
|
Discussion
CMV retinitis is most commonly seen in patients who are immunosuppressed, typically because they are infected with HIV or are undergoing chemotherapy.
Signs and symptoms. The presentation of CMV retinitis is often subtle, with symptoms of floaters or hazy vision. Examination may reveal one of several variable presentations, including focal retinitis, frosted branch angiitis, or perivascular hemorrhagic retinitis.
Diagnosis. Local diagnostic evaluation should include an ocular fluid sample, typically aqueous aspiration with PCR (polymerase chain reaction) evaluation for CMV DNA.1 Diagnostic anterior chamber paracentesis is a relatively safe and low-risk procedure,2 and it can help in making the diagnosis. At the time of the paracentesis, an intravitreal injection of ganciclovir 2 mg/0.1 mL may be given to cover all 4 possible viral etiologies (CMV, HSV-1, HSV-2, and VZV). If there is suspicion of aggressive ARN, treatment with IV acyclovir or valaciclovir (Valtrex) should not be delayed (see below).
The systemic evaluation typically includes testing for HIV and syphilis, a CBC, and a CD4 count as appropriate. Blood levels of CMV may not necessarily reflect the extent of retinitis and should not be used alone to rule out or follow CMV retinitis.2
Treatment. Management of CMV retinitis is typically coordinated with an infectious disease specialist and includes treatment for HIV with highly active antiretroviral treatment (HAART) if applicable. Systemic therapy consists of 900 mg of IV valganciclovir administered twice daily for 3 weeks, followed by maintenance therapy with 900 mg/day of oral valganciclovir for months, as needed.
Local ocular therapy includes intra-vitreal injections of ganciclovir 2 mg/ 0.1 mL or 2.4 mg/0.1 mL twice weekly for 3 weeks for an induction phase, and then once-weekly maintenance injections of ganciclovir or foscarnet for up to several months.1
Weekly dilated eye exams are necessary in the induction phase to ensure adequate response to the local and systemic antiviral therapy and to evaluate for any retinal breaks or involvement of the fellow eye.
Prognosis. Outcomes are variable and depend on the extent of retinitis and any associated retinal holes or detachments, as well as complications of intraocular inflammation such as epiretinal membrane formation.
Long-term follow-up is paramount.3 Surveillance must be continued until the CD4 count normalizes in HIV-positive patients, until any immune recovery uveitis is treated, or if immunosuppression is initiated or resumed.
A note on ARN. It is critical to consider ARN. This disease entity has a more rapid clinical course, typically is associated with more aggressive ocular inflammation in patients who are immunocompetent, and can be diagnosed via clinical examination and aqueous sample for HSV-1, HSV-2, and VZV (the most likely viral causes).
Although both ARN and CMV retinitis can be treated locally with intravitreal injections of ganciclovir and foscarnet, the systemic antiviral treatments are different. ARN related to HSV and VZV can be treated with oral or IV acyclovir/valaciclovir, but CMV retinitis must be treated with oral and/or IV valganciclovir.
Solving the Mystery
As Mrs. Morris did not have HIV or cancer, we hypothesized that the 1-month use of oral tofacitinib citrate increased her relative immunosuppression just enough to allow for the indolent development of CMV retinitis in her right eye. Tofacitinib citrate is an oral Janus kinase (JAK) inhibitor approved in the United States for the treatment of adult patients with moderate to severe RA who either cannot tolerate methotrexate or had an inadequate response to it. It can be used in combination with methotrexate or other nonbiologic disease-modifying antirheumatic drugs (DMARDs). The drug reduces the activity of inflammatory lymphocytes, thus improving rheumatoid inflammatory symptoms.4
Tuberculosis and other opportunistic infections, including CMV retinitis, have been reported in patients treated with tofacitinib.5 As the use of this medication—as well as others in its class—grows in clinical use, it is critical that ophthalmologists be aware of the potential ocular opportunistic infections in patients who take these drugs.
___________________________
*Patient name is fictitious.
___________________________
1 Smith BT, Regillo CD. “How to Treat Cytomegalovirus Retinitis.” EyeNet Magazine. 2005;9(9):37-39.
2 Smith IL et al. J Infect Dis. 1999;179(5):1249-1253.
3 Leeamornsiri S et al. J Ophthalmic Inflamm Infect. 2013;3(1):52.
4 Rawlings JS et al. J Cell Sci. 2004;117(Pt 8):1281-1283.
5 Winthrop KL et al. Ann Rheum Dis. 2016;75(6):1133-1138.
___________________________
Dr. Yamanuha is a retina specialist with the Mayo Clinic Health System in La Crosse, Wis., and assistant professor of ophthalmology at the Mayo Clinic in Rochester, Minn. Relevant financial disclosures: None.