By Eva Devience, MD, and F. Lawson Grumbine, MD
Edited By Steven J. Gedde, MD
Download PDF
After returning from a beach getaway, Carol Cooke,* a 35-year-old woman, felt irritation and a gritty sensation in her left lower eyelid. Remembering that a chalazion had been removed in that location 6 months previously, she booked an appointment for a chalazion consultation with our oculoplastics service.
We Get a Look
Ms. Cooke’s first visit with us was uneventful. Apart from the gritty sensation and chalazion removal, she had no ocular symptoms and no significant ocular or medical history. Her medications included sumatriptan, as needed, for migraine and oral contraceptives. Uncorrected visual acuity was 20/20 in each eye. Her pupils were equal, round, and reactive. There was no afferent pupillary defect. Her ocular movements were full and without pain. Intraocular pressure was 18 mm Hg in each eye.
On slit-lamp examination, her right eye was normal. Her left eye showed mild meibomian gland disease and a 3-mm subconjunctival white lesion in the fornix. The overlying conjunctiva was intact. No ulcerations or discharges were seen. The rest of her left eye exam was unremarkable.
Initial Misdiagnosis
At the time of her chalazion removal 6 months earlier, the outside physician ordered a biopsy, which confirmed the diagnosis of chalazion. With a small, white, postprocedural subconjunctival lesion in the setting of a biopsy that was negative for malignancy, our working diagnosis was a scar. We discussed with Ms. Cooke that a scar should improve or at least remain unchanged over time. We arranged for follow-up in a few weeks, with plans for repeat biopsy if the lesion had grown larger.
However, she returned 2 weeks later complaining of a rapidly enlarging mass with yellow crusting and discharge. The mass was now 1.3 × 1.0 cm in the anterior orbit, eroding through the conjunctiva. Her bulbar conjunctiva was now edematous and injected (Fig. 1). Her motility remained full, and there was no globe displacement.
 |
|
GROWING QUICKLY. The second time we saw Ms. Cooke, we had to rethink our initial working diagnosis. The mass had grown, and her bulbar conjunctiva had become edematous and injected.
|
Differential Diagnosis
Given the atypical presentation and rapidly progressive nature of the lesion, our concern was for an aggressive neoplasia, although an infectious or inflammatory process was also in the differential. Her history of chalazion and the lesion’s proximity to the lid margin made us consider sebaceous cell carcinoma, although the intact eyelid margin made it less likely. There were no eyelid or local skin lesions to suggest basal or squamous cell carcinoma of the eyelid. If the primary tumor had arisen from the conjunctiva, the ulcerated lesion would certainly raise concerns for ocular surface squamous neoplasia (OSSN), the most common malignant neoplasm of the conjunctiva; however, the orbital location was quite atypical, as intraorbital spread is an uncommon initial presentation. Another possibility was lymphoma, in which the tumors are typically salmon colored and can be a sign of systemic lymphoma. Finally, vascular tumors may occur after chalazion excision.
A Repeat Biopsy
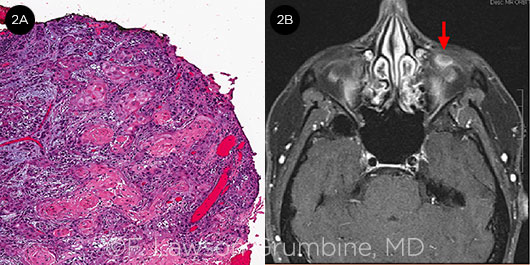
An incisional biopsy of the mass showed moderately differentiated squamous cell carcinoma (Fig. 2A). Magnetic resonance imaging (MRI) of the orbits with contrast was ordered to define the extent of the lesion (Fig. 2B). This demonstrated a 1.5 × 1.0 × 0.7–cm contrast-enhancing mass abutting the globe. Given that HIV/AIDS is a risk factor for OSSN, we ordered an HIV test, which was negative.
 |
|
WE GATHER THE EVIDENCE. (2A) A biopsy revealed keratinizing squamous cells invading the underlying stroma. (2B) An MRI scan demonstrated a contrast- enhancing intraconal lesion (arrow) adjacent to the inferior left globe.
|
Treatment
A few days later, we performed an anterior orbitotomy for tumor excision with margins. While excising margins, it was noted that the tumor was tightly adherent to the eyelid, so we also performed a wedge resection of the piece of eyelid at the anterior margin, followed by a membrane graft reconstruction. Ms. Cooke’s pathology revealed a 1.3 × 0.9 × 0.3–cm gross squamous cell carcinoma specimen, most likely of conjunctival origin. All of her margins (including her eyelid) were negative.
Postoperatively, we had extensive discussions with Ms. Cooke about the next steps. Although her tumor was completely excised with negative margins, we were concerned about microscopic residual tumor cells, because it had already seeded deeper into the anterior orbit by the time she presented to us. After a multidisciplinary tumor board discussion with radiation oncology, we offered Ms. Cooke electron beam radiation as adjuvant therapy. This has a shallower penetration than conventional X-rays, affording the ability to deliver high-dose radiation to the anterior orbit while sparing the retina and optic nerve. Based on pretreatment simulations, the predicted side effects were dermatitis, conjunctival scarring, and cataract that may occur 2 to 3 years afterward. Her visual acuity should be otherwise preserved.
About the Diagnosis
A wide spectrum of disease. OSSN is an umbrella term for a spectrum of dysplastic and malignant epithelial lesions of the conjunctiva and cornea. OSSN lesions involving only the epithelium may be termed conjunctival squamous neoplasia.1 Risk factors include ultraviolet light exposure, human papilloma virus (type 16) infection, HIV/AIDS, and xeroderma pigmentosum.
Histology determines the OSSN spectrum:
- Grade 1, conjunctival epithelial dysplasia: Dysplastic cells are confined to the basal layers of the epithelium.
- Grade 2, carcinoma-in-situ: The lesion involves the full thickness of the epithelium.
- Grade 3, squamous cell carcinoma: Invasive disease is present.
Presentation. The most common presentation of OSSN is an elevated, vascularized lesion in the limbal region of older patients. Ms. Cooke’s orbital mass was an unusual presentation.
Treatment. OSSN is typically treated with wide surgical excision and, to reduce recurrence, adjunctive techniques (e.g., application of alcohol or cryotherapy). One should refrain from direct manipulation of the tumor to avert microscopic seeding to other ocular structures (“no touch” technique).
Recently, there has been a paradigm shift in the treatment approach to OSSN.2 Clinicians may now use topical chemotherapy as both adjunctive and primary therapy. Topical mitomycin C, 5-fluorouracil, and interferon alfa have been shown to be effective. Galor et al. advocated adjuvant interferon therapy in patients with high-risk characteristics after surgery—namely, positive margins, tarsal involvement, or recurrent disease.2 Radiation therapy or enucleation remains reserved for those with intraocular or orbital invasion and systemic metastasis, which fortunately are uncommon in OSSN.1
Recurrence. Positive surgical margins have long been identified as a risk factor for recurrence, with some series showing that excised lesions with negative surgical margins had a recurrence rate of 5%, compared with 53% for those with positive margins.3
Patient’s Progress
Ms. Cooke chose to undergo electron beam radiation adjuvant therapy after excision, and she has done well thus far. She developed mild radiation dermatitis of the eyelid, but her vision has remained 20/20 and her oral mucous membrane graft has remained intact. There have been no signs of recurrence. She is also undergoing a genetics consultation, given her relatively young age at the time of diagnosis.
Reviewing her outside hospital records, we wondered whether she had had a chalazion at all. We obtained her initial pathology slides, which were first read by a general pathologist. A second evaluation by an ocular pathologist was read as conjunctival squamous cell carcinoma. Most likely, the “chalazion” removal seeded this carcinoma into the deeper orbit where it grew into an orbital mass. Ms. Cooke’s case is a reminder to question a prior diagnosis if the presentation is atypical or there is concern for a malignant lesion.
___________________________
* Patient name is fictitious.
___________________________
1 Kim JW, Abramson DH. Clin Ophthalmol. 2008;2(3):503-515.
2 Galor A et al. Ophthalmology. 2012;119(10):1974-1981.
3 Erie JC et al. Ophthalmology. 1986;93(2):176-183.
___________________________
Dr. DeVience is a second-year ophthalmology resident and Dr. Grumbine is an oculoplastics surgeon and assistant professor; both are at the University of Maryland in Baltimore. Relevant financial disclosures: None.