By Bradley Sifrig, BS, Valentina P. Lozano, MD, Meggen A. Walsh, DO, and David M. Mills, MD
Edited by Steven J. Gedde, MD
Download PDF
Probably just another orbital cellulitis,” thought the on-call ophthalmology resident when contacted by the emergency department (ED) about a patient with a 1-week history of orbital pain, swelling, and visual loss. However, that proved not to be the case when 52-year-old Joseph Johnson* presented to the ED from a local correctional institution after his pain became intolerable.
A week earlier, Mr. Johnson had been seen at an outside facility where he had a workup of unknown scope. He said that he been scheduled to get “further testing.” However, he was unable to follow up there after being transferred to a different correctional institution as the result of a hurricane.
History
Mr. Johnson had a medical history of hypertension, type 2 diabetes mellitus, chronic obstructive pulmonary disease, and asthma. His only medication was metformin.
Symptoms. When asked for further information about his ocular symptoms, Mr. Johnson told us that the swelling around his right eye had started about 6 months ago and had slowly worsened over time. He had also noticed some mild visual loss and pain in his right eye during that period.
In the past week, however, the swelling had increased significantly, and his condition had rapidly progressed to the point where he could no longer see with his right eye, and the pain was unbearable. Mr. Johnson also reported some subjective fevers, chills, and night sweats along with right cheek numbness and headaches, all of which had started within the past week.
We Get a Look
As soon as we entered Mr. Johnson’s room, it was evident that we were dealing with something more complex than “just another orbital cellulitis.”
Exam findings. On external examination, Mr. Johnson had marked periorbital swelling and erythema of his right upper eyelid, along with proptosis, ptosis, and chemosis protruding between his lids. There was obvious crusted discharge and dried blood along the eyelid margins and the surrounding skin.
He had no light perception in the right eye and 20/30 visual acuity in the left eye. His intraocular pressures were 45 mm Hg and 18 mm Hg, respectively. His right pupil was fixed at 5 mm and nonreactive, whereas the left pupil was 3 mm and reactive.
We performed a limited anterior segment exam. We noted diffuse chemosis, conjunctival injection, a hazy cornea, a deep anterior chamber, and no obvious hypopyon or hyphema. Dilated fundus exam was not performed at the time, given Mr. Johnson’s alarming symptoms and the potential need for emergent surgical intervention.
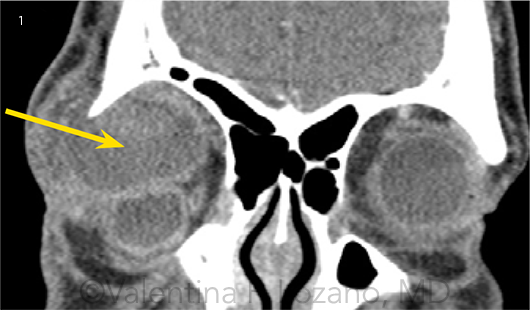
Imaging. We ordered a stat computed tomography (CT) scan, which showed a large extraconal mass measuring 3.7 × 3.4 × 2.5 cm anteriorly in the right orbit (Fig. 1). There was difficulty localizing the lacrimal gland on the CT, and it was unclear whether the gland was a part of the lesion or was only displaced.
Initial procedures. Bedside incision and drainage were performed, but no purulent discharge or other fluid was obtained. We then proceeded to lateral canthotomy and cantholysis, which decreased the intraocular pressure to 28 in the right eye but only partially relieved Mr. Johnson’s pain.
 |
|
CT IMAGING. (1) Coronal view shows a large extraconal mass measuring 3.7 × 3.4 × 2.5 cm anteriorly in the right orbit.
|
Differential Diagnosis and Next Steps
Our initial differential diagnosis of Mr. Johnson’s orbital swelling was broad and included infectious, neoplastic, traumatic, autoimmune, and idiopathic etiologies. We considered infectious causes, specifically abscess, but the CT did not show the expected degree of soft tissue swelling, and the incision and drainage had failed to yield purulent matter. He had no history of ocular trauma, making a traumatic etiology unlikely. The unilateral presentation with a lack of systemic symptoms was not consistent with an autoimmune etiology.
Homing in on the cause. We thought that the timeline of his disease progression, along with the CT scan showing an extraconal mass, made neoplasm the most likely diagnosis. Therefore, we narrowed our differential to focus on neoplastic etiologies, including lacrimal gland tumors, vascular tumors, neural tumors, mesenchymal tumors, lymphoproliferative disorders, and metastatic disease.
Mr. Johnson had experienced a slowly increasing periorbital swelling with an acute and severe worsening of symptoms. The acute-on-chronic nature of his presentation led us to further refine our differential to fast-growing orbital tumors as well as orbital tumors that commonly undergo spontaneous hemorrhage. Thus, lymphangiomas, adenocystic adenocarcinomas, and cavernous hemangiomas were all high on our list.
Emergent treatment. At this point, Mr. Johnson was still in significant pain following lateral canthotomy and cantholysis. The decision was made to proceed emergently to the operating room for an anterior orbitotomy with exploration and partial mass excision. In the OR, the mass had the gross appearance of necrotic tissue with intermixed blood clots. Frozen sections were sent to pathology to assist with final diagnosis.
What the Tests Revealed
Pathology findings. Pathology of the mass revealed spindle-shaped tumor cells with elongated nuclei forming bundles. Additionally, there were several areas of ischemic-like necrosis with some cystic degeneration.
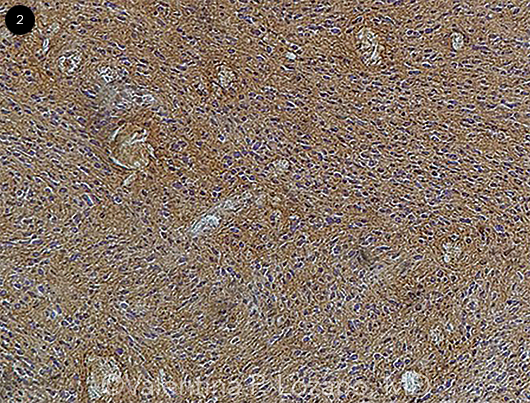
No mitotic figures were seen in any of the samples. The tumor was diffusely positive for S-100 immunohistochemical (IHC) stain, signifying that the lesion most likely had a neural crest origin (Fig. 2). IHC stains for SMA (smooth muscle marker), STAT-6 (solitary fibrous tumor marker), and ERG (vascular maker) were all negative. The morphology of a low-grade spindled lesion with strong, diffuse S-100 positivity led us to the unexpected diagnosis of an orbital schwannoma.
Magnetic resonance imaging. MRI was obtained a few days after Mr. Johnson had partial excision of the mass. T1-weighted images without contrast showed that the largely cystic-appearing portion of the mass was probably related to blood products in evolution, based on the increased signal intensity.
After contrast administration, the lesion appeared to be predominantly cystic centrally with an enhancing rim. The MRI image showed that the orbit had been adequately decompressed, and the globe appeared more normal when compared with the presurgical CT image. Given the histologic diagnosis of a schwannoma, the MRI findings were consistent with some degree of bleeding into the schwannoma, which likely caused Mr. Johnson’s acute orbital symptoms.
Diagnosis confirmed: schwannoma. Oncology specialists were consulted during Mr. Johnson’s presentation, and they agreed with the diagnosis of schwannoma. They recommended further surgical excision to achieve negative margins if possible, depending on the extent of tumor.
Mr. Johnson’s tumor pathology showed no areas of increased mitotic activity or other signs of malignancy. In the absence of malignant features, there is limited to no role for chemotherapy or targeted agents in management of schwannoma. Therefore, Mr. Johnson’s further treatment will be predominantly surgical, with probable postoperative radiation therapy.
 |
|
PATHOLOGY FINDINGS. A pathology slide of Mr. Johnson’s orbital mass shows diffuse positivity for S-100 immunohistochemical staining.
|
Discussion
Orbital schwannomas are rare and have been shown to account for only 0.7% to 2.3% of biopsy-proven orbital tumors. Schwannomas originate through hyperplasia of Schwann cells, the myelin-producing cells of the peripheral nervous system. Most orbital schwannomas arise from sensory nerves, particularly branches of V1.
Orbital schwannomas have also been reported to originate from V2, from cranial nerves in the orbit, and from the nerves that innervate the extraocular muscles. Extremely rarely, optic nerve schwannomas have been reported; according to the proposed mechanism, the lesion arises from autonomic perivascular nerves surrounding the optic nerve sheath.1
Characteristics of orbital schwannomas. These lesions are almost always unilateral, benign, and noninvasive. They have a slow rate of growth and commonly present with an insidious onset of orbital swelling.
Early manifestations of orbital schwannoma include gradual proptosis and lid swelling. Late manifestations include diplopia, restricted ocular motility, mild impairment in visual acuity, and symptoms of optic nerve compression.
Unusual aspects of Mr. Johnson’s case. Our patient’s orbital schwannoma was highly unusual in presenting with an acute onset of orbital swelling, severe orbital pain, and total loss of vision in the affected eye. This acute presentation is in marked contrast to the typical chronic, indolent nature of orbital schwannomas, and it can be explained by an acute hemorrhage occurring in the otherwise chronically enlarging tumor.
On reviewing the literature, we found only 2 similar reported cases of hemorrhage into an orbital schwannoma.2,3 However, in those cases, despite the hemorrhage, both patients had a more chronic presentation of orbital swelling, making Mr. Johnson’s case unique.
Patient’s Progress
At the most recent evaluation, approximately 4 months after his initial presentation, Mr. Johnson had not regained functional vision in the right eye. The tumor appears to have been appropriately debulked, as his intraocular pressure has remained normal. However, further resection will be necessary, as he had only partial resection of the schwannoma.
Mr. Johnson is currently undergoing evaluation by ophthalmology in cooperation with the neurosurgery and otolaryngology departments. His case will be discussed at a tumor board so that the appropriate surgical approach can be determined, based on the extent and involvement of the tumor. The tentative plan is for exenteration of the right orbit with probable postoperative radiation therapy.
___________________________
* Patient name is fictitious.
___________________________
1 Sweeney AR et al. Surv Ophthalmol. 2017;62(1):43-57.
2 Gündüz K et al. Ophthal Plast Reconstr Surg. 2011;27(3):e51-54.
3 Pushker N et al. Br J Ophthalmol. 2011;95(8):1168, 1180-1181.
___________________________
Mr. Sifrig is a third-year medical student, Dr. Lozano is an ophthalmology resident, Dr. Walsh is a neuropathology fellow, and Dr. Mills is a professor of oculoplastic surgery; all 4 are at the University of Florida in Gainesville. Relevant financial disclosures: None.