Download PDF
There’s some comfort in numbers—at least when it comes to research. To date, most information about outcomes in pediatric cataract surgery has been based on case series. But a recent prospective observational registry study included 1,266 eyes in 994 children to create a focused snapshot of children who’d had cataract surgery during the preceding 45 days.1
The children, who had surgery at 61 centers in the United States, the United Kingdom, and Canada, were enrolled in the Pediatric Eye Disease Investigator Group (PEDIG) cataract surgery registry at any age from birth to less than 13 years old. The researchers recorded baseline characteristics as well as data on use and type of intraocular lenses (IOLs), refractive errors, operative and perioperative complications, and eye and systemic conditions.
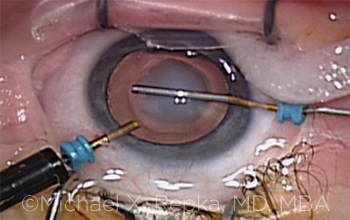 |
PEDIATRIC CATARACT SURGERY. Anterior capsulotomy being performed with a 25-gauge forceps in a young patient.
|
Age at surgery. Only one-third of cataract surgeries were performed in the first year of life, which initially seems surprising, said lead author Michael X. Repka, MD, MBA, vice chair for clinical practice at Wilmer Eye Institute, Baltimore. “In reality, however, many children are born with mild cataracts that worsen over time, or [they] develop cataracts during the first decade of life.” There was a family history of infantile cataract in nearly 20% of cases, although associated systemic conditions such as galactosemia were rare.
Treatment trends. Age also played a dramatic role in the use of IOLs, which were implanted in 59% of all eyes, he said. “It’s almost as though a switch was turned on at the first birthday,” said Dr. Repka, explaining that only 8% of eyes underwent IOL surgeries in the first year of life, whereas implants became nearly universal thereafter, especially after 2 years of age. In children who received an implant, the prediction error of the implanted IOL was less than 1.00 D in about half the eyes, but greater than 2.00 D in 15% of eyes.
Dr. Repka said that the study’s observations may reflect practice patterns influenced by publication of data from the Infant Aphakia Treatment Study. In that trial, which included only infants with unilateral cataracts, the researchers found that use of IOLs at less than 1 year of age was associated with the need for more surgery and provided no better vision than the use of aphakic contact lenses.2
Complications rare. In this registry study, intraoperative complications occurred in 5% of the participants, with the most common being posterior capsule rupture in eyes undergoing primary IOL placement. The most common postoperative complications were increased intraocular pressure and cloudy cornea.
The low rate of complications is particularly reassuring, said Dr. Repka, given that this cohort reflects outcomes attained in a community setting, rather than in a randomized trial with defined protocols.
More to come. The researchers are now preparing 1-year data, and they plan to continue follow-up for 5 years to provide information about longer-term complications and the accuracy of current IOL prediction formulas, as well as visual outcome data for both unilateral and bilateral cataract surgery—with and without IOL implantation. “With the size of this cohort,” said Dr. Repka, “we hope to be able to shed significant light on outcomes across many age ranges.”
—Annie Stuart
___________________________
1 Repka MX et al. Ophthalmology. 2016;123(12):2462-2473.
2 Plager DA et al. Ophthalmology. 2011;118(12):2330-2334.
___________________________
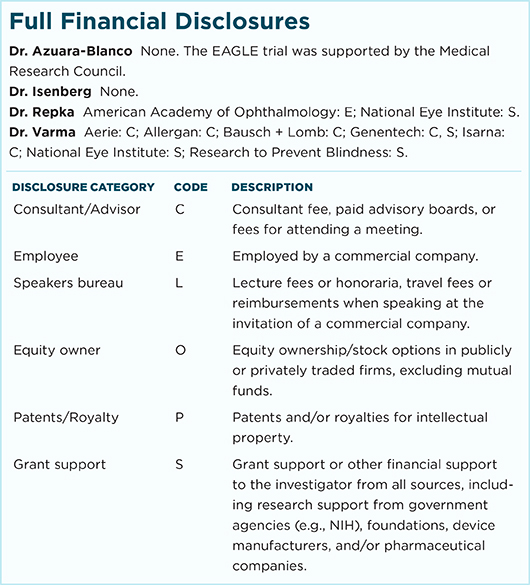
Relevant financial disclosures—Dr. Repka: National Eye Institute: S.
For full disclosures and disclosure key, see below.
More from this month’s News in Review