By Nika Bagheri, MD, Shreya Baid, and Ninel Z. Gregori, MD
Edited by Sharon Fekrat, MD, and Ingrid U. Scott, MD, MPH
Download PDF
First described in 1908 by Scottish ophthalmologist George Coats, Coats disease is characterized by retinal vascular abnormalities, exudates, and hemorrhage. Onset of symptoms typically occurs before age 15, with cases that involve leukocoria and strabismus presenting much earlier than those with subjective visual loss alone.1 Coats disease tends to be unilateral. Although it does not have specific racial or ethnic associations, it preferentially affects males.
Initially, vascular abnormalities include telangiectasia, aneurysmal dilations, and increased tortuosity in the equatorial and peripheral retina, more commonly affecting the inferior and temporal quadrants. As the disease progresses, there is increased intraretinal and subretinal exudation, which may lead to exudative retinal detachment. Patients may develop choroidal or retinal neovascularization and rubeosis, which can lead to hemorrhage, glaucoma, and loss of the eye.
Etiology
Genetics. Coats disease is a nonhereditary ocular disease. Although the exact underlying mechanism remains unknown, a somatic missense mutation of the Norrie disease protein (NDP) gene on chromosome Xp11.2, causing a deficiency of the norrin protein product, has been proposed.2 Norrin has been implicated in normal retinal vasculogenesis. The high male-to-female ratio (3:1) may result from partial escape due to X inactivation in females.2
Pathophysiology. The classic histopathological processes of Coats disease include breakdown of the blood-retina barrier at the level of the vascular endothelium, as well as loss of pericytes and endothelial cells. Subsequent leakage into the vessel wall, vessel wall thickening, saccular and fusiform aneurysms, and vessel obliteration occur.3 Exudates in the intra- and subretinal space contain blood, lipid, cholesterol crystals, lymphocytes, and fibrin.3
Vascular endothelial growth factor (VEGF), which plays an important role in the formation of normal retinal vessels and vascular permeability, is elevated in Coats disease.4,5
Complications. Exudative retinal detachment frequently occurs, with infiltration of lipid-laden macrophages in the subretinal space. Gliosis also develops in the nontelangiectatic retinal regions, and advanced macular disease may be associated with gliotic submacular nodules.3 Chronic exudative retinal detachment can involve the anterior segment secondarily and lead to painful neovascular glaucoma, blindness, and sometimes enucleation.6
Diagnosis
Because Coats disease encompasses a wide clinical spectrum, the diagnosis should take into account age, family history, laterality, and stage of presentation. In addition to the clinical examination, fluorescein angiography, ultrasound, and/or computed tomography imaging are useful modalities when the diagnosis is challenging.5
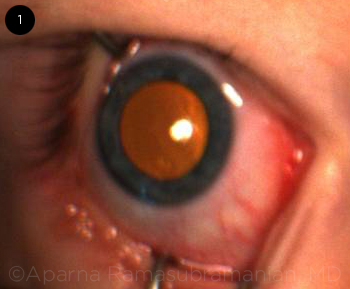
Differential diagnosis. In a young child with retinal detachment causing leukocoria (Fig. 1), the differential includes retinoblastoma, persistent fetal vasculature, familial exudative vitreoretinopathy (FEVR), retinopathy of prematurity, and toxocariasis.3,5
In an older patient with prominent exudates and telangiectasia, the differential includes FEVR; uveitis and vasculitis; vasoproliferative tumors and hamartomas; and retinal vascular diseases such as macular telangiectasia type 1, vein occlusion, and, rarely, retinal artery macroaneurysm.
 |
|
PUPIL IN COATS’ PATIENT. Retinal exudation can give the appearance of xanthocoria, a more yellow variant of leukocoria.
|
Staging
Shields et al. have proposed a staging system to describe the severity of Coats disease based on the appearance of telangiectasias, exudation leading to retinal detachment, and secondary complications.6 These stages help guide the clinician in choosing management options and evaluating the prognosis.
- Stage 1: Retinal telangiectasias only
- Stage 2a: Telangiectasias and extrafoveal exudation
- Stage 2b: Telangiectasias and foveal exudation
- Stage 3a: Subtotal exudative retinal detachment
- Stage 3b: Total exudative retinal detachment
- Stage 4: Total detachment with secondary glaucoma
- Stage 5: Advanced end-stage disease
Case Study: Coats Disease in a Young Adult
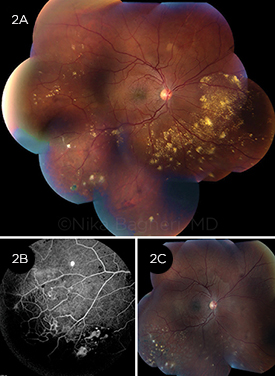 A 24-year-old man presented with blurry vision, photopsias, and floaters in the right eye for the past 2 months. Best-corrected visual acuity was 20/20 in both eyes. (2A) Fundus photograph of the right eye revealed peripheral exudates associated with telangiectatic vessels and focal areas of gliosis. (2B) Fluorescein angiography of the right eye periphery demonstrated “light bulb” telangiectasias, hairpin loops, areas of hypofluorescence consistent with exudates, and areas of hyperfluorescence consistent with leakage from abnormal vasculature. The left eye was unremarkable. Our patient was diagnosed with stage 2A disease and received sectoral photocoagulation in the inferotemporal quadrant. (2C) Fundus photograph of the right eye after sectoral laser photocoagulation shows improvement in exudation. The patient is stable with visual acuity of 20/20 in both eyes at 6-month follow-up. A 24-year-old man presented with blurry vision, photopsias, and floaters in the right eye for the past 2 months. Best-corrected visual acuity was 20/20 in both eyes. (2A) Fundus photograph of the right eye revealed peripheral exudates associated with telangiectatic vessels and focal areas of gliosis. (2B) Fluorescein angiography of the right eye periphery demonstrated “light bulb” telangiectasias, hairpin loops, areas of hypofluorescence consistent with exudates, and areas of hyperfluorescence consistent with leakage from abnormal vasculature. The left eye was unremarkable. Our patient was diagnosed with stage 2A disease and received sectoral photocoagulation in the inferotemporal quadrant. (2C) Fundus photograph of the right eye after sectoral laser photocoagulation shows improvement in exudation. The patient is stable with visual acuity of 20/20 in both eyes at 6-month follow-up.
|
Treatment
Treatment of Coats disease varies based on the severity of the disease. Mild cases can be observed, but if exudation, or retinal or subretinal fluid, is present, the mainstay of treatment is laser ablation or cryotherapy in areas of telangiectasia and nonperfusion.5
Laser. Thermal laser photocoagulation has historically been the most effective treatment. The goal of laser ablation in Coats disease is to obliterate abnormal vasculature and eliminate hyperpermeability of aneurysms.6 Laser can be used for direct photocoagulationof vascular abnormalities even if subretinal fluid is present.
Cryotherapy. Cryotherapy is typically indicated if peripheral retinal telangiectasia with significant exudative retinal detachment impedes adequate laser photocoagulation.5
Surgery. If total exudative retinal detachment, nonclearing vitreous hemorrhage, and/or secondary complications are present, surgery may be needed for retinal reattachment or enucleation.5,6
Adjuvant therapy. Recently, anti- VEGF agents have been found to be effective in reducing subretinal fluid and exudation. For example, a retrospective review by Villegas et al. reported on 24 children who presented with exudative retinal detachment, vascular telangiectasia, and retinal ischemia and were treated with photocoagulation and intravitreal bevacizumab. All cases had complete resolution of the detachment and anatomic improvement of the retina.7
However, vitreoretinal fibrosis and associated tractional retinal detachment may develop following anti- VEGF treatment.8 More studies are needed to further evaluate the efficacy of anti-VEGF agents either as adjuncts or monotherapy.4
Prognosis
The prognosis depends on disease severity at presentation. When mild, Coats disease typically progresses gradually, and treatment can often lead to restoration of vision. Patients who present at a younger age (less than 5 years of age) have been reported to undergo a more rapid decline, while those older than 10 years have a more insidious course.1 Risk factors that predispose to visual decline include postequatorial, diffuse, or superior location of telangiectasia and exudation; failed resolution of subretinal fluid after treatment; presence of retinal macrocysts; presence of retinal detachment at presentation; and involvement of the macula.5,6 Secondary complications include glaucoma, rubeosis iridis, phthisis bulbi, cataract, and uveitis. Patients with advanced disease may develop a painful blind eye necessitating enucleation.
___________________________
1 Morris B et al. Eye. 2010;24(12):1797-1801.
2 Black GC et al. Hum Mol Genet. 1999;8(11):2031-2035.
3 Ghorbanian S et al. Ophthalmologica. 2012;227(4):175-182.
4 Chaudhary KM et al. J Pediatr Ophthalmol Strabismus. 2013;50(1):11-19.
5 Sigler EJ et al. Surv Ophthalmol. 2014;59(1):30-46.
6 Shields JA et al. Am J Ophthalmol. 2001;131(5):572-583.
7 Villegas VM et al. Clin Ophthalmol. 2014;8:973-976.
8 Ramasubramanian A et al. Br J Ophthalmol. 2012;96(3):356-359.
___________________________
Dr. Bagheri is a vitreoretinal surgical fellow at the Bascom Palmer Eye Institute in Miami, Fla. Ms. Baid is a medical student at the University of Miami Miller School of Medicine in Miami, Fla. Dr. Gregori is chief of the Eye Care Section at the Miami Veteran Affairs Hospital as well as an associate professor of clinical ophthalmology at the Bascom Palmer Eye Institute in Miami, Fla. Relevant financial disclosures: None.