Download PDF
Ta Chen Peter Chang, MD, assumed that he would never again see the 16-year-old who came to him for a second opinion. She had previously been diagnosed with juvenile open-angle glaucoma, was doing well on eyedrops, and did not need surgery. He confirmed that her pressure was controlled and that her condition should remain stable.
Flash forward to 1 year later when she returned with “incredibly high intraocular pressure [IOP]” and significant vision loss in both eyes. “Her right eye had a dense superior arcuate scotoma and a nasal step; her left had a dense inferior arcuate scotoma,” said Dr. Chang, at the Bascom Palmer Eye Institute. “I was shocked. I thought I’d dropped the ball. What had I missed?”
He’d missed the fact that the patient’s mother had always administered the drops, with 100% adherence. Then the young woman went off to college and stopped taking her meds. “That’s how she fell off the cliff,” Dr. Chang said.
Dr. Chang performed emergency surgery, and the patient no longer even needs drops, so the story ends well. Still, he frets that he had not emphasized the importance of treatment adherence. “I had not given her the tools to deal with the disease.” And he can’t stop wondering: What if? What if he’d performed surgery when he first saw her? But surgery isn’t benign, and she was doing well with drops. “When do I pull the trigger?” he said. “That’s a conundrum.”
In Search of Answers
Childhood glaucoma is full of such conundrums, and pediatric glaucoma specialists have more questions than answers. For instance, which children with risk factors will go on to develop the disease? Why do some children respond to treatment and others do not? Can you predict, based on some severity score index, which child will benefit from treatment and which one will not? If so, how should you proceed? Finally, what if you suspect that nothing will work?
In some children, a single surgery may be curative “and change the next 75 years of the child’s life,” Dr. Chang said. In others, the prognosis may be so poor that it may be best to forgo further treatment. “As ophthalmologists, we want the children to see as well as they possibly can. We also want the patient to lead as good a life as possible. Sometimes, I think those 2 [desired outcomes] may be in conflict,” he said.
In particular, he said, “Every time we do another surgery, put the child to sleep, we take away from the quality of life” for both the child and his or her parents. For instance, the multiple challenges of missing school and home life, traveling to the hospital, and preparing for and recovering from surgery means that, from the child’s perspective, “childhood halts,” he said. The child’s family is under significant strain as well. “Every examination under anesthesia is a stressful event.”
Dr. Chang is looking for a balance. “If you know further surgeries will not yield much benefit, wouldn’t it be better to help prepare the family to raise their child as a blind person, so they don’t spend their life tethered to a disease? These are the questions I struggle with at night.”
A High-Stakes Game
Ophthalmologists who treat childhood glaucoma emphasize that there is no room for error. “This is a very vulnerable population. This is not an 80-year-old whose vision is slowly going,” said Faruk H. Örge, MD, at Case Western Reserve University. “In childhood, glaucoma can be very aggressive. The patient can lose sight very quickly.”
In children, it can be “an all-or-none” situation, said Alana L. Grajewski, MD, at Bascom Palmer. But with prompt diagnosis and surgery, some children with congenital glaucoma “stand a good chance of having normal or near-normal vision the rest of their lives,” she said. “That’s why it’s important to know when to refer.”
“That’s one of the reasons some of us are attracted to this field,” said Dr. Chang. “It’s a high-stakes game. There are children who, with 1 procedure, never need another surgery and probably won’t need drops. And there are others who, even after many surgeries, have poor prognoses.”
The Impact of Puberty on IOP
When Dr. Toris ran out of rabbits in the middle of a study, she got new ones. And when the replacement rabbits yielded “all kinds of different results” from their predecessors, Dr. Toris was stumped. The replacements were the same gender, the same breed, and from the same vendor. “The only thing I could think of was age.” As it happened, the second group of rabbits was a lot younger than the first group.
Something similar happened in a separate study involving primates. The results obtained with younger monkeys were inconsistent with those of the older ones they replaced, Dr. Toris said.
Around the same time, Dr. Toris started hearing from glaucoma specialists that young patients were responding differently to medical treatment than adults. This sparked a “Eureka!” moment. Perhaps there was a link between what the doctors were saying and what she was observing in her lab’s replacement animals. “The first thing you think about is aqueous humor dynamics,” said Dr. Toris.
As a result, she began treating young rabbits with pressure-lowering drops—timolol, latanoprost, or acetazolomide. She then measured the rabbits’ IOP and aqueous humor at various time points, from when they were just weaned to when they reached sexual maturity. Her findings, which she is preparing for publication, indicate that IOP increases until puberty. At this point, it drops, and then it rises again after puberty.
None of these drugs worked in young rabbits. They only worked after sexual maturity. The question, Dr. Toris said, is: Why isn’t IOP progression linear, as it is in adults?
“Certain things that work in adults don’t work so well in children,” she said. “We know these drugs were designed and tested in adults, but children are not miniature adults. They’re quite different.”
Dr. Toris said there’s precedent for this finding in children with diabetes, whose blood sugar is well controlled before puberty, difficult to maintain during puberty, and controlled once again after puberty.1 In either scenario—glaucoma or diabetes—children experience rapid growth and development in a short time as well as hormonal changes that “throw the body for a loop.” And, as with diabetes, knowing that IOP changes are nonlinear in childhood may have clinical implications, she said.
___________________________
1 Cho YH et al. Pediatr Diabetes. 2014;15(1):18-26.
|
Not Just Small Adults
Childhood glaucoma is more than just glaucoma with a very early onset. “It’s a completely different type of glaucoma, and it is managed differently,” said Dr. Grajewski.
A panocular disorder. In adults, glaucoma is diagnosed based on the pathology of the optic nerve. But in children, glaucoma is characterized by IOP-related damage to the entire eye.
Primary congenital glaucoma, which accounts for 50% to 70% of all childhood glaucoma (and occurs in about 1:10,000 births in Western developed countries), is not an isolated disease of the optic nerve. Rather, it is a panocular disorder that is defined by structural, functional, and physiological parameters, Dr. Grajewski said. “It affects every part of the eye.”
Other types of childhood glaucoma can occur at any time. It may be acquired (e.g., as a result of trauma or uveitis); alternatively, it may be associated with either a systemic disorder, such as Sturge-Weber syndrome, or an ocular disorder, such as aniridia or Peters anomaly.
Developmental complications. Because the immature eye is elastic, elevated IOP causes structural changes. The cornea may stretch, grow, and bulge outward, leading to the descriptive name buphthalmos, or ox-eye. Globe distension also results in iris stromal hypoplasia, ectopia lentis, and Descemet breaks, which degrade optical quality. Corneal haze is another hallmark of the disease.
Moreover, a child’s eye is growing and the visual system is still immature, thus raising the risk of amblyopia, the most common cause of visual impairment in children with glaucoma.1
Diagnostic challenges. Eighty percent of cases are diagnosed during the first year of the child’s life.2 But young children can be fidgety and uncooperative, so imaging is a challenge, which complicates the diagnosis, Dr. Örge said.
Moreover, IOP readings can be difficult to obtain. For instance, if the child is crying or holding his breath, IOP tends to be artificially elevated, making it more difficult to recognize if there’s a problem. While examination under sedation or anesthesia can calm the patient, these agents can affect IOP. “Most sedation and anesthesia agents lower IOP, so if we obtain the IOP 5 minutes after [anesthesia is given], the IOP would be falsely lower than what it actually is,” Dr. Örge said. (One exception to this is ketamine, which elevates pressure, as it tightens the extraocular muscles, he noted.)
Specialty clinics have portable slit lamps and tonometers that make the job easier. It’s important to have this armamentarium at hand so that you can care for the patient, Dr. Örge said. “Our job is to make sense of what is real and not real.”
Treatment challenges. Because of the myriad potential complications in childhood glaucoma, treatment involves much more than just lowering IOP. “If you look at the outcome as being [reduction of] pressure, you can win the battle of pressure but lose the war on amblyopia,” Dr. Grajewski said.
Even if the glaucoma is controlled, the child can lose vision if the refractive error is not corrected, Dr. Örge noted. Other problems may develop, such as cataracts resulting from surgical procedures. “One disease can give birth to others,” he said.
“For anybody treating childhood glaucoma, meticulous attention to visual development and the amblyopia treatment is part of the game,” Dr. Chang said. This requires knowledge of prescribing glasses, checking vision, and patching. The stakes are highest in younger children. “You have to monitor [them] very carefully because the brain can turn the eye off very quickly when they’re young.”
Thus, as Dr. Grajewski recommended, “If you are uncomfortable treating childhood glaucoma, refer to a center that has a specialist. If you treat pediatric glaucoma yourself, involve your colleagues early to be sure you are not just treating the pressure but the final vision outcome as well.”
A note on puberty. “Most of what we know about eye physiology is from adults, and that doesn’t always transfer to children. Certain treatments that work well in adults may be unpredictable in children,” said Carol B. Toris, PhD, at Case Western Reserve University.
And that unpredictability may be exacerbated during puberty. Dr. Toris’ current research indicates that IOP progression isn’t linear in children, as it usually is in adults (see “The Impact of Puberty on IOP”). The bottom line: You might treat a patient who is in the middle of puberty differently than you would a prepubescent child or an adult, she said.
A note on surgery. In adults, the treatment paradigm generally moves from medications to laser to incisional surgery. But in children, surgery is the mainstay, with the most common surgical interventions being trabeculotomy and goniotomy.3,4 “In children, meds are more of a bridge until you do surgery,” Dr. Grajewski said.
Dr. Örge elaborated on this point: “In adults, drainage starts failing after years of working. In pediatrics [in congenital glaucoma], this mechanism is defective from the get-go,” he said. In a defective drainage system, medications are only temporary, he added.
A note on family dynamics. “When you’re sitting in the exam room and looking at an adult, it’s the adult. But with a child, everyone in the room is affected,” said Dr. Grajewski. “You’re treating the entire family, plus the glaucoma, the amblyopia, and the genetics,” she said. This means treatment is time intensive and requires the integration of services, including social services, she noted.
“The referring physician should let families know that childhood glaucoma is a very complex problem,” Dr. Örge said. “Hearing this from the referring physician makes it much easier to take in and reinforces the message that the disease can be controlled but that it needs a very high level of compliance.”
In addition, the child’s future needs to be addressed. “Most adults [diagnosed with glaucoma] have had fruitful lives, and we try to make sure they don’t lose useful vision before the end of their lives,” Dr. Chang said. “With pediatric glaucoma, the outlook can be very different. That’s actually becoming a larger part of my conversation with parents. I want them to have a broad view”—that is, to focus not only on the disease but also on the child’s quality of life.
Childhood Glaucoma Research Network Powers Up
Pediatric glaucoma specialists have a feel for what works and what doesn’t in terms of treatments, said Dr. Chang. For example, he knows that if 2 prior surgeries failed, a third probably won’t work either. “So we do have some inkling,” he said. Still, he wonders, “Is this an eye where 1 surgery is a slam dunk? Or is this child going to be blind down the road? Can we support our hunches with good evidence?”
In the past, studies have lacked the statistical power to answer such questions because of small numbers of participants. That has changed, however, with the establishment of the Childhood Glaucoma Research Network (CGRN). Thanks to the network, clinicians and scientists who specialize in childhood glaucoma now have a place to share their expertise and pool information on outcomes.
CGRN has grown from an informal discussion with a few dozen researchers at the 2012 ARVO meeting into a full-fledged organization that has more than 150 members in 31 countries, said Dr. Grajewski, who raised funding for the group, which is now located at the Samuel and Ethel Balkan International Pediatric Center at Bascom Palmer. “Anybody with an interest in caring for children should become a member,” Dr. Grajewski said. Already, CGRN has created a childhood glaucoma classification system to overcome inconsistent terminology (see “Classification of Childhood Glaucoma”). It has established registries at Wills Eye Hospital and Moorfields Eye Hospital to capture data worldwide. And it has developed a website for parents of children with glaucoma.
Other issues CGRN is addressing include the following: How does the disease start? What are the long-term outcomes? How can vision loss be prevented? “Looking at genetics is high on our list. Treatment options are, too,” Dr. Grajewski said. She reminds clinicians that not all children with pediatric glaucoma are alike. “With uveitic glaucoma and Sturge-Weber, for example, what do you do first? Second? We don’t know the best treatment pathway.”
Perhaps the collective wisdom and experience of CGRN members will generate answers. As Dr. Örge put it: “If you really want to understand whether goniotomy works better than trabeculotomy, you need lots of patients. For this reason, the network becomes an integral part of what we do.”
|
Volatile and Enduring
It’s never static. The experts also emphasized the volatile nature of pediatric glaucoma. “With childhood glaucoma, it’s always something,” Dr. Grajewski said. “That’s one of the biggest challenges we face. The condition changes as time goes on.”
“Pediatric glaucoma is much more complex than many glaucomas we take care of in adults,” Dr. Örge agreed. “What you do with a 1-month-old is very different from a 1- or 18-year-old. Being suspicious about this condition is the key.”
It’s never over. “The pathologic elevations of pressure in infancy result in considerable changes in adult eyes,” Dr. Grajewski said. It’s important to keep this in mind, she said, because when ophthalmologists first see these patients as adults, there’s a tendency to think that “they had glaucoma as kids and then it’s over. But these problems are ongoing, because they occurred at a sensitive time.”
The residual effects of increased axial length caused by early stretching may include high myopia, a thinner sclera, an enlarged cornea, and an increased risk of retinal detachment. Corneal haze or altered corneal physiology can cause glare; in addition, they may complicate cataract surgery.
These are lifelong issues. “Any surgeries on an adult eye with a history of childhood glaucoma can be magnitudes more complex,” Dr. Chang said.
On the Horizon
Dr. Örge is conducting research using ultrasound biomicroscopy to observe outflow mechanisms. It’s not a new instrument, he noted, but he’s using it in a different way to see pathology that is ordinarily obscured by a hazy cornea or a structural abnormality.
Dr. Örge is hopeful that a better understanding of outflow mechanisms will lead to better treatment decisions. In current practice, he said, “Sometimes you do 2 or 3 angle procedures in each eye before you realize that won’t work,” he said. With regard to outflow issues, he said, “If you know the trabecular meshwork is impaired but Schlemm’s canal is okay, you know that the angle procedure is going to work.” But if Schlemm’s and the collector channels are not working, a drainage device may be a better choice.
But there is reason for optimism, said Dr. Chang. The outcomes for childhood glaucoma are becoming better defined through the use of information technology, he said. In addition, a new network is helping to link doctors with others who have an interest in the field (see “Childhood Glaucoma Research Network Powers Up”).
“With timely, accurate diagnosis, expert surgery, and meticulous follow-up [to monitor] visual development, many children previously destined to be blind will now lead lives as sighted persons,” said Dr. Chang.
___________________________
1 Chang TC et al. Curr Ophthalmol Rep. 2015;3(2):85-90.
2 www.glaucomafoundation.org/childhood_glaucoma.htm.
3 Chen TC et al. Ophthalmology. 2014;121(11):2107-2115.
4 Papadopoulos M et al. Eye. 2014;28(8):931-943.
Meet the Experts
Ta Chen Peter Chang, MD Assistant professor of clinical ophthalmology and pediatrics at the Bascom Palmer Eye Institute in Miami. Relevant financial disclosures: None.
Alana L. Grajewski, MD Director of the Samuel and Ethel Balkan International Pediatric Glaucoma Center, director of pediatric glaucoma, and professor of clinical ophthalmology at the Bascom Palmer Eye Institute in Miami; founding director of the Childhood Glaucoma Research Network. Relevant financial disclosures: None.
Faruk H. Örge, MD William R. and Margaret E. Althans Chair and Professor of Pediatric Ophthalmology and director of the Center for Pediatric Ophthalmology and Adult Strabismus, University Hospitals Case Medical Center; chief of pediatric ophthalmology, Rainbow Babies and Children’s Hospital and University Hospitals Eye Institute; and assistant professor of pediatrics and associate professor of ophthalmology, Case Western Reserve University School of Medicine in Cleveland. Relevant financial disclosures: None.
Carol B. Toris, PHD Professor of ophthalmology and visual sciences at Case Western Reserve University in Cleveland. Relevant financial disclosures: None.
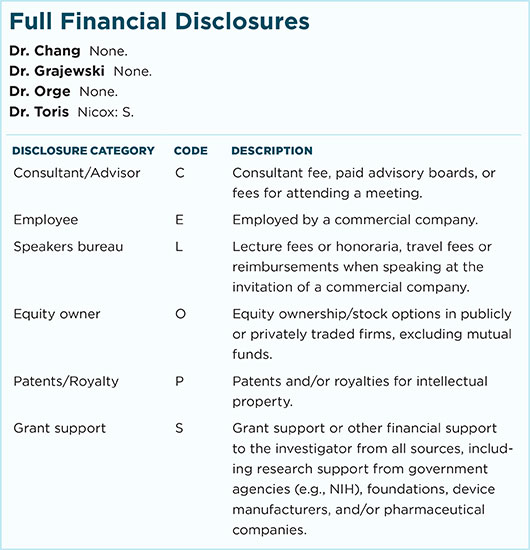
For full disclosures and the disclosure key, see below.
|