Download PDF
Armed with the latest IOLs and power formulas, cataract surgeons have largely solved the problem of minimizing postoperative spherical error, with close to 80% of patients being within 0.5 D of target.1 But what are the best ways to also manage or reduce preoperative corneal astigmatism at the same time? A comprehensive plan is essential for both your patients and your practice.
“Over the last decade, we’ve experienced an explosion of technology in terms of IOLs and femtosecond lasers that has allowed us to concentrate on astigmatism,” said Kendall E. Donaldson, MD, MS, at the Bascom Palmer Eye Institute in Plantation, Florida. “It’s an important evolution in cataract surgery. No longer are we just fixing a cataract and putting a patient in a pair of glasses.” She explained that the secondary goal in cataract surgery involves targeting and treating astigmatism, with a goal of increasing spectacle independence.
Establishing Initial Expectations
To begin with, it’s critical to manage patient expectations. In particular, the notion of astigmatism “correction” is a popular misnomer, said Kevin M. Miller, MD, at the University of California, Los Angeles. “Treating astigmatism during cataract surgery isn’t like putting a muffler on a car. It’s not going to bring the noise level down to a perfect zero—that almost never happens.” As a result, he said, he uses the term “astigmatism management” to express reality.
“I always tell my patients that our goal is not to eliminate the astigmatism but just minimize it to a point that it’s under a threshold of affecting vision significantly,” said Sumit Garg, MD, at the University of California, Irvine. You also have to discuss the inherent unpredictability when it comes to managing astigmatism, he noted. “Following surgery there’s always the small chance that the patient will need something else done, such as [surgical correction of] an IOL rotation or some kind of additional procedure to help achieve the refractive goal.”
 |
|
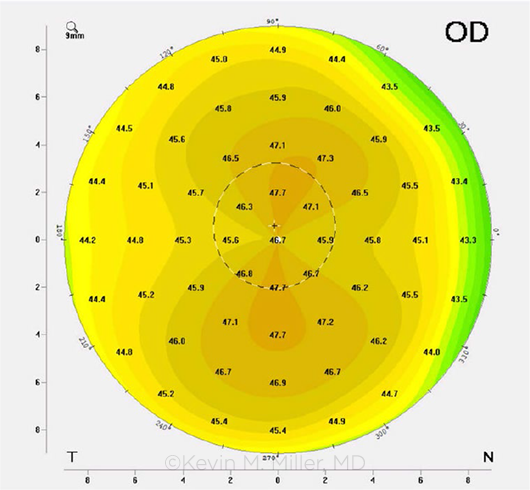
WITH-THE-RULE. An example of vertically steep corneal astigmatism.
|
The Stepladder Approach
Several options for managing astigmatism can be used alone or in combination. These include incision placement on the steep axis of the cornea, single or paired peripheral corneal-relaxing incisions (PCRIs), and implantation of toric IOLs.2 And different surgeons will opt for a particular technique given the amount and type of astigmatism as well as the patient’s age.
“There’s a lot to sort out,” said Dr. Miller. That’s why he teaches his residents a systematic stepwise approach. “It’s important to take a few steps back and look at the big picture. How can I develop a plan of attack for handling astigmatism for any patient who walks in my door?”
Categorize your patients. Dr. Miller’s approach is simple and straightforward. After measuring the magnitude of astigmatism by corneal topography, and in some instances corneal tomography, he places patients into one of four categories: astigmatism of less than 1 D, 1 D up to 1.5 D, 1.5 D up to 4 D, and more than 4 D.
“Each ‘bucket’ necessitates a certain approach or combination of approaches,” said Dr. Miller. “It’s similar to treating glaucoma. You climb the ladder as you need to.”
Measure early and often. This tier-based approach is a nice way to organize your surgical options, said Uday Devgan, MD, FACS, but it only works if the astigmatism in question is regular and symmetric. “This is an important factor,” said Dr. Devgan, in private practice in Los Angeles and Beverly Hills. “The only way we can really treat astigmatism effectively is if we have regularity. So measure, measure, measure prior to categorizing your astigmatic patients. Be diligent when you look at the ocular surface, make sure all of your measurements agree, look at your topography and tomography with an eye on symmetry and regularity. Only then can we move forward with effective treatment.”
 |
|
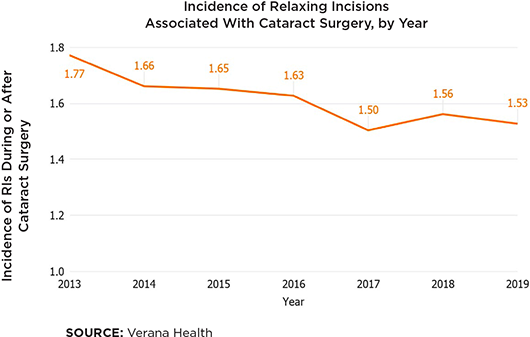
IRIS Registry Snapshot: Use of Relaxing Incisions. Verana Health analyzed data from the Academy’s IRIS Registry (Intelligent Research in Sight) to determine how the use of PCRIs—formerly known as limbal-relaxing incisions—in patients undergoing cataract surgery has changed in the last several years. Registry data from 2013 to 2019 showed that the real-world incidence of relaxing incisions has decreased since 2013, possibly due to a rise in toric IOL use. Note: The Academy has partnered with Verana Health to curate and analyze IRIS Registry data.
|
Nuances of Treatment
Surgical preference will vary from ophthalmologist to ophthalmologist. However, there is a general consensus on which techniques work well for managing different levels of astigmatism.
Treating astigmatism of <1 D. For most eyes, said Dr. Miller, placement of the phacoemulsification incision on the steep corneal axis is sufficient to manage small amounts of astigmatism, and it takes care of 80% of his patients. “If the patient is steep at axis 48, I’ll move the incision over to 48 degrees and operate there,” he said. “It’s of course important to have in mind your surgically induced astigmatism here. Personally, I use 0.4 D as my own value—but it might be 0.1 D for some surgeons or 0.7 D for others. If you move your incision on the steep axis, you’re going to knock the astigmatism in that axis down by whatever your surgically induced value is. So, if a patient starts off with, say, 0.7 D at 48 degrees, I move my incision to 48 degrees, and I’m getting, on average, 0.4 D of effect. I’ve just knocked their astigmatism down to 0.3 D.”
Treating 1 D to 1.5 D. For this range, Dr. Miller prefers PCRIs for both ease and cost. “Some surgeons might not feel comfortable performing relaxing incisions because of their unpredictability and will prefer to switch to a toric IOLs.”
But as Dr. Miller pointed out, unlike relaxing incisions, toric lenses can sometimes rotate and can add a significant out-of-pocket cost. “Relaxing incisions are therefore my go-to in this group of patients,” he said. “I’ll make the relaxing incisions on the steep axis. So if it’s at 48 degrees, I’ll make my two incisions at 48 degrees and then make the phaco incision through the most convenient relaxing incision. If we perform the cataract surgery in that fashion, I can get up to 1.5 D of astigmatism treatment very readily and with very good predictability.”
Beyond 1.5 D, Dr. Miller notes, the downsides associated with PCRIs can start to outweigh the potential benefits, particularly when toric IOLs can be used.
Treating 1.5 D to 4 D. Because of the technological advances associated with the latest generation of toric IOLs, they are the preference of many cataract surgeons when preoperative astigmatism is anywhere above 1.5 D. But many surgeons extend their use to anything above 1 D.
“For 1 D all the way up to 4 D, a toric IOL is the best choice for me,” said Dr. Devgan. “Yes, there is potential for misalignment or post-op rotation, but these IOLs are very accurate, very effective, and very predictable.”
Dr. Donaldson agreed. “There is a question of whether relaxing incisions regress over the first six months, so the toric lens is my preference for any astigmatism over 1 D—and definitely anything over 1.25 D—especially considering the level of quality, stability, and accuracy that the new generation of lenses provides.” The distinction between with-the-rule and against-the-rule astigmatism is important here as well, she added. “Because a small amount of with-the-rule astigmatism can result in better vision for some patients, I tend to be more aggressive when treating the against-the-rule variety and will start using a toric lens at a slightly lower level of astigmatism in those instances.”
And with regard to misalignment or post-op rotation experienced with these IOLs, “digital alignment improves the former, and surgical repositioning can rectify the latter,” said David F. Chang, MD, in private practice in Los Altos, California. “I’d therefore recommend a toric IOL when it is most important to have a spherical refractive outcome. This would include any patient receiving a presbyopia-correcting IOL, those who are most determined to avoid spectacles, and monofocal IOL patients with higher amounts of astigmatism.”
Treating 4 D and beyond. A combined procedure is likely necessary if your patient is in this range. But first look carefully at the topography. Does this patient have truly regular and symmetric astigmatism—or is irregularity or asymmetry present? That could be a sign of keratoconus or forme fruste keratoconus, pellucid marginal degeneration, or another condition. “Patients who have irregular corneas or keratoconus may not be suitable for toric IOLs or even incisional approaches,” said Dr. Devgan. “We may even choose to leave them with their existing astigmatism because they can be happy going back to their rigid contacts, which certainly provide excellent vision for them. These are rare instances though.”
If the patient is truly regular and symmetric, the best approach is a high-powered toric lens followed by laser refractive surgery, Dr. Devgan said. “I’ll increase the spherical IOL power to leave the patient a little myopic so that I can clean up the remaining diopters of astigmatism with an excimer laser, for example, photorefractive keratectomy or LASIK. The first shot is going to put the patient on the green, and with the second shot a few months later, we’ll sink the putt. We just can’t get a hole in one under these circumstances.”
A note on challenging eyes. “Since last fall, we’ve been using the Light Adjustable Lens (RxSight) for our most challenging astigmatism patients,” such as post-LASIK or post-RK eyes, Dr. Chang said. “With the ability to do multiple sequential light adjustments postoperatively, this technology can correct up to 4.5 D of astigmatism.”
Helping Patients Decide
In general, the treatment of preexisting astigmatism during cataract surgery is not covered by Medicare, and so any management of the condition will result in the patient paying out of pocket.
And that presents a quandary: How best to explain the benefits of astigmatism management to patients? “There is no refractive benefit to having astigmatism, so correcting it should be advantageous for any patient who doesn’t wear glasses full time,” Dr. Chang said. “Our challenge is explaining this to patients so that they can decide whether the value is worth the extra cost.”
Keep it simple. “It starts with a mindset of not leaving opportunity on the table,” said Dr. Garg. “Not just from the financial perspective of your practice, but also—and more importantly—from a patient’s perspective. You can really make a big difference in people’s lives if you’re treating even low amounts of astigmatism. So we try to put it in terms that the patient can relate to, such as, ‘Yes, the cataract surgery will be covered by insurance, but the astigmatism correction will be your responsibility, much like hearing aids, dentures, or glasses.’”
When Dr. Donaldson outlines astigmatism management to her patients, she focuses on outcomes. “There’s a tendency for ophthalmologists to present too many options to patients at once, which can make the decision-making process very complex,” she said. “So we have to do our best to simplify how we explain new things to our patients.” Thus, instead of leaning on terms such as “corneal-relaxing incisions” and “toric lens,” she focuses on what patients would like to achieve in practical terms, “because they can relate more to the ability to see distance and near more clearly.”
And Dr. Chang shows patients their color topography map and compares it to a spherical cornea map. “I then explain that whenever they are not wearing spectacles, what they are able to see naturally—for instance, at distance—will be better if we cancel out the astigmatism blur. I might also explain that the less astigmatism they have, the better nonprescription sunglasses and readers will work.”
Don’t presume. Ultimately, however, a patient may decide that he or she is comfortable forgoing any additional procedure above and beyond the removal of the cataract.
“My initial patient questionnaire is rather simple,” said Dr. Devgan. For example, he asks, “Will you be interested in correcting your vision so that you can see some ranges far or near without glasses? Or do you prefer to wear glasses full time?” The answers can be surprising, he said. “Believe it or not, quite a few of my patients don’t want me to bother with their astigmatism. They want to go back to the same glasses. That’s just how they like to be seen and how they like to see the world.”
Avoid overselling. Whatever the patient chooses, you don’t want to come off as being too pushy.
“Some patients get upset because they perceive their surgeon as more of a salesperson than a physician,” said Dr. Donaldson. “So, there’s a little finesse that goes into this process. We have to be very careful in the way we present our technology, and we have to be aware of our patients’ perception of that technology. The goal is creating understanding through a partnership with the patient, avoiding misperceptions, and establishing accurate expectations.”
|
Hitting That Sweet Spot
Another variable to consider is the post-op refractive target. Should you aim for zero astigmatism from the outset—or aim higher and let the patient drift down to zero over time?
Accounting for potential drift. “Early on in my career, my target was zero, but that’s no longer the case,” said Dr. Miller. “My sweet spot now is to leave the patient a little bit vertically steep, around 0.3 D at 90 degrees, because we know that people go from vertically steep to horizontally steep as they age. So if they end up zero dead-on postoperatively, they’re going to have great vision right away, but then years later they’re going to be back in glasses. But if we leave them a little vertically steep, they’ll eventually drift down to zero.”
Considering patient age. The post-op target also depends on the patient’s age. “Someone who is on the older side most likely won’t experience significant astigmatic shift in the next several years,” said Dr. Garg. For patients who are approaching age 70, he said, “a tiny bit of shift will occur—but if someone is younger, you could see a much more pronounced shift. It’s not always linear over time, but that’s the general principle: The older the patient is, the less the potential shift.”
Thus, Dr. Garg said, if he has a 75-year-old patient with a posterior subcapsular cataract, “my target is pretty close to zero.” In contrast, in a 55-year-old patient, “I aim for a little with-the-rule astigmatism so it can drift down with time.”
Considering patients’ preferences. Whatever approach you take to manage astigmatism, be sure to give your patient a voice in the matter, Dr. Miller said. “What kind of outcome does the patient prefer? Do they prefer to wear glasses in certain situations and environments? Are they comfortable with multiple procedures to reduce their astigmatism? You need to make them a partner in the process and tailor your treatment to their desires because, ultimately, this is an investment in the rest of the person’s life.”
___________________________
1 Koch DD et al. J Cataract Refract Surg. 2017;43(6):717-718.
2 Amesbury EC, Miller KM. Curr Opin Ophthalmol 2009;20(1):19-24.
Meet the Experts
David F. Chang, MD Clinical professor of ophthalmology at the University of California, San Francisco, and in private practice in Los Altos, Calif. Relevant financial disclosures: Carl Zeiss; C; Johnson & Johnson Vision: C; RxSight: C.
Uday Devgan, MD, FACS In private practice at Devgan Eye Surgery in Beverly Hills, Calif., chief of ophthalmology at Olive View UCLA Medical Center, and clinical professor of ophthalmology at the Stein Eye Institute at the University of California, Los Angeles. Relevant financial disclosures: CataractCoach.com: O.
Kendall E. Donaldson, MD, MS Professor of clinical ophthalmology and medical director at Bascom Palmer Eye Institute in Plantation, Fla. Relevant financial disclosures: Alcon: C,L; Bausch + Lomb: C; Carl Zeiss: C; Johnson & Johnson Vision: C.
Sumit Garg, MD Associate professor of ophthalmology and vice chair of clinical ophthalmology at the University of California, Irvine. Relevant financial disclosures: Alcon: C,L; Carl Zeiss: C; Johnson & Johnson Vision: C; Verana Health: C.
Kevin M. Miller, MD Kolokotrones Chair in Ophthalmology and chief of cataract and refractive surgery at the Stein Eye Institute at the University of California, Los Angeles. Relevant financial disclosures: Alcon: C; Johnson & Johnson Vision: C.
Full Financial Disclosures
Dr. Chang Carl Zeiss: C; Eyenovia: O; iDrops: C,O; Ivantis: C,O; Johnson & Johnson Vision: C; Mynosys: C,O; Perfect Vision: C; PowerVision: C,O; Presbyopia Therapies: O; RxSight: C; Slack: P; Surface: O; Versant Ventures: O; Viewpoint: C,O.
Dr. Devgan Advanced Euclidian Solutions: O,C; CataractCoach.com: O; IOLcalc.com: O; LensGen: O,C; Mynosys: C; Novartis/Alcon: L; specialty surgical: O.
Dr. Donaldson Alcon: C,L; Allergan: C; Carl Zeiss: C; Eyevance: C; Johnson & Johnson Vision: C; Kala: C; Omeros: C; Shire: C; Sun: C.
Dr. Garg Aerie: C; Allergan: C; Avedro: C; Carl Zeiss: C; EyePoint: C; Eyevance: C; Johnson & Johnson Vision: C; Kala: C; New World Medical: C; OcuTrx: O; Shire/Takeda: C,L; SightLife Surgical: C; Verana Health: C; Vision Care: C.
Dr. Miller Alcon: C; Bausch + Lomb: C; ianTech/Zeiss: C; Johnson & Johnson Vision: C.
Disclosure Category
|
Code
|
Description
|
| Consultant/Advisor |
C |
Consultant fee, paid advisory boards, or fees for attending a meeting. |
| Employee |
E |
Employed by a commercial company. |
| Speakers bureau |
L |
Lecture fees or honoraria, travel fees or reimbursements when speaking at the invitation of a commercial company. |
| Equity owner |
O |
Equity ownership/stock options in publicly or privately traded firms, excluding mutual funds. |
| Patents/Royalty |
P |
Patents and/or royalties for intellectual property. |
| Grant support |
S |
Grant support or other financial support to the investigator from all sources, including research support from government agencies (e.g., NIH), foundations, device manufacturers, and/or pharmaceutical companies. |
|