Download PDF
Although the visual system involves about half ofthe brain’s circuits—many of which are vulnerable to head injury—vision has long been sidelined in the world of concussion diagnosis and treatment. That is beginning to change.
When Laura J. Balcer, MD, MSCE, was doing a fellowship in neuro-ophthalmology at the University of Pennsylvania in the 1990s, she and her colleagues were a bit puzzled by their patients with multiple sclerosis (MS). Many had vision-related complaints, despite seeing 20/20 on the black-and-white visual acuity chart. Later research revealed that many of these patients had deficits in contrast measures—but not in visual acuity.
“A parallel paradigm has emerged with concussion,” said Dr. Balcer, at NYU School of Medicine in New York City. “We’ve learned that vision is an important—and intricate—piece of neurological disorders. Ophthalmology plays a crucial role, not only for the sideline identification of concussion but also in concussion rehabilitation and research.”
But vision has largely been neglected as one of the key areas to assess following concussion, said Steven L. Galetta, MD, also at NYU School of Medicine. “We need ophthalmology’s involvement.”
This takes on even greater urgency, given a 60% increase in the incidence of concussion from 2007 to 2014, with the largest increases occurring among adolescents.1 The CDC estimates that 3.8 million concussions are diagnosed in ERs each year, with many more going undiagnosed.2
How Concussion Impacts Vision
A subset of mild traumatic brain injury (mTBI), concussion is a blow to the head that may induce any new neurological signs or symptoms.2
Visual skills affected. Although an mTBI rarely involves the afferent system, it can have an impact on several visual tasks in the efferent system, said neuro-ophthalmologist David Kaufman, DO, at Michigan State University in East Lansing. “This can involve convergence, accommodation, saccadic mechanisms, vestibular-ocular function, pursuit, and rarely, cranial nerves IV and VI—and very rarely, cranial nerve III.”
Common symptoms. Headache and slowed thinking are common complaints, said Dr. Kaufman. “Photophobia is often associated with headache, which is very reminiscent of migrainous symptoms.” In addition, he said, student athletes will use the word “dizzy” to describe a variety of issues, including vision problems. “When I hear this word, it’s a signal that we need to look at the ocular motor system quite carefully.”
Trouble with reading or using screens can be a sign of a convergence issue, said Dr. Balcer. The eyes are fine, she said, but they aren’t working together as a team. Even repetitive subconcussive impacts—despite a lack of symptoms—have been shown to temporarily impair ocular near point of convergence (NPC) in football players.3
Patients might also see the world jumping up and down and suffer motion sensitivity, said Dr. Galetta, which may be due to a malfunctioning vestibular system.
Timing of onset. Symptoms may arise immediately after impact or be delayed by days, said Dr. Balcer. Sometimes patients do not notice the symptoms until they try to get back to their daily routine, said neuro-ophthalmologist Heather E. Moss, MD, at the Illinois Eye and Ear Infirmary in Chicago. For example, kids going back to school in the fall may have trouble with schoolwork because they are using their visual systems more than they did during the summer.
Sideline Protocols for Athletes
For the past 5 years, Dr. Kaufman has attended practices and traveled with the Michigan State University football team as a neuro-ophthalmologist. “On the sidelines, we have limited time to make decisions about whether or not a player can continue or should get further evaluation,” he said. “More vision tests on the sidelines could potentially be useful.” This is particularly true since many aspects of vision relate to high cognitive function, which is often compromised in mTBI.4
Vision training. Because most sports medicine doctors and trainers haven’t received much training in the visual system and aren’t comfortable assessing vision, said Dr. Galetta, education needs to be part of the answer. “Instead,” he said, “they do what they know best, which is to ask questions about how the player is thinking and feeling, and to observe how the player is walking.”
SCAT 3. Released in March 2013, the Sports Concussion Assessment Tool (SCAT 3)5 is the most common tool used on the sidelines for concussions, said Dr. Kaufman. “It includes a symptom checklist and also checks memory, balance, and cognitive changes.” However, it “doesn’t use visual testing tools at all,” he said, adding that along with SCAT 3, the Michigan State players are assessed for personality changes. (Note: The SCAT 3 is for those older than age 13. Younger children should be assessed with the Child-SCAT 3.)
Neuro-ophthalmology testing. With the luxury of having a neuro-ophthalmologist on board, the Michigan State team is able to call on Dr. Kaufman to also do modified neuro-ophthalmologic testing on the sidelines. “If the student athlete passes the SCAT 3,” he said, “we have him perform a modified doll’s head maneuver in both the vertical and horizontal gaze. If it exacerbates any symptoms such as headache, dizziness, or cognitive disturbances, this may assist us in disqualifying the athlete from play.”
King-Devick test. As nonpaid consultants, Drs. Balcer and Galetta were asked 7 years ago to explore the usefulness of the King-Devick (K-D) test, which can assess saccades and vergence, said Dr. Galetta. The K-D test (which was developed by a team of optometrists who test kids for dyslexia) gauges the amount of time it takes to read numbers with variable spacing on 3 test cards.
In 2015, a meta-analysis found the K-D test to be a sensitive candidate for a sideline test, effective with athletes of all ages, said Dr. Balcer. In fact, it has been shown to capture concussions that other types of sideline tests miss, in part, because athletes tend to underreport symptoms.2 “A robust set of data indicates that it can accurately assess concussion on the sidelines, is feasibly administered by parents and coaches in about a minute, and doesn’t require any special equipment,” she said. “We think it is close to prime time use.”
What’s exciting about the K-D test, added Dr. Moss, is that it assesses a variety of integrated visual systems all at once. Requiring saccades, attention, and visual interpretation, the test can evaluate functioning of the brainstem, cerebellum, and cerebral cortex.2
“Other batteries used for sideline tests don’t capture the neurological systems as well as this test does,” she said. She added that it may be helpful both for diagnosis and for determining who should be pulled from play. This is important, as athletes are especially vulnerable to a more serious head injury if they sustain a second hit shortly after the initial concussion.2 (Technically, any athlete diagnosed with a concussion should be pulled from play, but that doesn’t always happen.)
Michigan State is carefully evaluating the K-D test but is not currently using it, said Dr. Kaufman. “I believe it’s useful,” he said, “but with so much noise and distraction, it may be challenging to use at college games in front of 75,000 people.”
Other potential tests. Drs. Balcer and Galetta are also exploring the feasibility of a picture-naming test. “Applying lessons from the MS field,” said Dr. Balcer, “we’re getting away from exams we traditionally do in the office and moving toward performance measures, which are either timed or easily scored” by clinicians. However, if an eye movement exam (K-D or picture naming) is used on the sideline, she added, it should not only include an ocular motor evaluation but also look for signs of an inaccurate saccade or choppy pursuit.
Although eye movement recordings may sound attractive, said Dr. Galetta, they aren’t practical for the sidelines, given the costs and need for equipment calibration and data interpretation. “However, eye trackers such as the EyeLink 1000 are very important for the investigation of concussion” (see “On the Horizon”).
Concussion Centers
Thanks to greater awareness of the potentially devastating sequelae of traumatic brain injury, concussion centers are springing up across the country. Although it’s difficult to track how many are now in existence, the Concussion Legacy Foundation offers a free online tool to connect patients with concussion centers and specialists.1
NYU Langone’s Concussion Center incorporates an interdisciplinary approach to treating TBI in patients of all ages and from a range of injuries, including sports, car crashes, and work accidents, said Dr. Balcer. “We’re fortunate here to have a rehabilitation physical medicine department that includes vision and vestibular rehabilitation, where therapists help patients with all kinds of neurological problems.”
The center is staffed by physical, occupational, and vestibular therapists; psychologists; and speech-language pathologists specializing in concussion treatment. The center also offers medical services from neurologists and neuro-ophthalmologists, among other physicians. Going forward, the team approach may be key, Dr. Balcer said. Among other issues, it’s critical to ensure that the head injury has not caused other eye problems such as retinal detachment or traumatic uveitis.
One potential downside of specialized concussion centers, said Dr. Moss, is that when you’re a hammer, everything is a nail. “The care team needs to ensure that symptoms such as photophobia are not caused by something other than concussion such as undiagnosed uveitis, which has directed treatments.”
___________________________
1 Concussion Clinics. www.concussionfoundation.org/learning-center/concussion-clinics. Accessed Sept. 26, 2016.
|
In the ER
A recent study found that 56% of concussions are diagnosed in the ER, with another 29% diagnosed in a physician’s office.1
Call the ophthalmologist? “Unless the patient is complaining of certain visual problems, there may not be a role for an emergent ophthalmic exam,” Dr. Moss said. However, said Dr. Kaufman, ophthalmology needs to be urgently involved if there is persistent unilateral visual loss or double vision or if there are gross monocular or binocular eye movement issues or the presence of a homonymous hemianopia or red flags such as hyphema or a subconjunctival hemorrhage.
An ophthalmologist might be brought in because an eye is down and out or a pupil is larger on one side than the other, said Dr. Balcer. “Those are signs that necessitate collaboration with a neurologist or neurosurgeon.” Other reasons to involve ophthalmology, said Dr. Galetta, might be patients complaining of blurred vision, or the need to perform tests that ER doctors may not know how to do (such as assessing convergence insufficiency).
History and exam. The history and exam are critical, said Dr. Balcer. “It’s important to remember that the injured person may or may not have told an on-call nurse about trouble with dizziness or reading, for example—but when they are asked carefully about visual systems, most patients who’ve had a concussion respond affirmatively.”
Neuroimaging. A computed tomography (CT) scan should be done immediately if the patient has any change in consciousness, said Dr. Balcer. A focal neurologic deficit or homonymous visual field deficit should also be an indication for CT, said Dr. Kaufman. “And at Michigan State, we’re extremely conservative. We will proceed with magnetic resonance imaging [MRI] if any symptoms persist.”
With concussion, neuroimaging should be normal, said Dr. Galetta. “If there is any evidence of injury on a scan, you’re beyond a concussion.”
In Your Office
Patients don’t necessarily present first to the ER, Dr. Balcer noted. Here are some issues for ophthalmologists to consider during an office-based evaluation.
Challenges evaluating concussion. After a concussion, it’s often difficult to tease out the source of the problem that’s leading to vision challenges, said Dr. Moss. “People might just say they’re having trouble reading, which could be due to a variety of things,” she said. “Maybe they can’t make out the letters, can’t move their eyes together or accurately, or have trouble with visual interpretation.”
If the symptoms are worse with motion, she said, it’s also hard to pinpoint the problem. Is it the vestibular system that’s the issue? The ocular motor system? The connection between the two?
Questions to ask. Proceed with a neuro-ophthalmological review, which is a very detailed and complete history, said Dr. Kaufman. Try to figure out the most likely location of the injury, to help guide the subsequent exam.
Ask patients how they are doing with reading and navigation, said Dr. Moss. “Have they had any difficulties getting back to their day-to-day activities? Any problems with peripheral vision, double vision, blurry vision? And then go from there.”
Exam and imaging. Dr. Moss does general ophthalmic and neurologic exams and targets the detailed examination to the problem that she suspects is causing the patient’s symptoms. She said she has a low threshold for obtaining neuro-imaging, if it has not already been performed.
She first ensures the patient doesn’t have another problem (such as severe cataract or traumatic optic neuropathy) that may be contributing to symptoms. “One of the most important things is not to miss a traumatic optic neuropathy, Horner syndrome, or cranial nerve palsy,” she said, “which suggests there may be more to this than a simple concussion. These would require a neurological evaluation and treatment and more specific ophthalmological management.”
A thorough exam, said Dr. Kaufman, would include visual acuity with refraction; color vision; pupil evaluation; complete and careful ocular motility assessment, including pursuit, saccadic movements, vestibular ocular response, and convergence and divergence; visual fields; and a dilated fundus exam, followed by a modified neurologic exam.
Insult to injury. Patients also may have prolonged symptoms such as headache, dizziness, and lowered tolerance for noise and light lasting months, said Dr. Moss. When this is the case, they are said to have postconcussive syndrome (PCS).
Some of these individuals might have previously undiagnosed problems that impede their ability to cope, said Dr. Moss. “They might have had a mild refractive error before the concussion and did fine without glasses, but now [the visual] processing challenges make this burdensome for them. In these cases, an ophthalmological exam will be particularly helpful.”
Treatment for PCS
In many cases, patients who’ve sustained a concussion will get better over time without treatment, said Dr. Moss. But for those with PCS, treatment may be necessary to ease symptoms. “If they perceive these as a visual problem, they may want an easy fix such as glasses, but often there are no easy fixes,” she said. “These are often more complex processing issues.”
Counseling. One of the most helpful strategies is to explain the root cause of the symptoms to the patient, Dr. Moss said. For example, it can be helpful to explain that light sensitivity isn’t a problem with the eyes, but with the brain. “This relieves some of the patients’ worry,” added Dr. Kaufman, “and allows them to adapt more quickly.”
In addition, he said, the patient may need to be counseled about returning to activity in a staged way. This is determined on a case-by-case basis. “There are some similarities between physical and cognitive injuries,” said Dr. Kaufman, “and to gradually progress, it helps to find that sweet spot between too much and too little activity.”
Vision rehabilitation. At NYU Langone’s Concussion Center, Margaret A. Waskiewicz, MS, OTR/L, specializes in vision rehabilitation, which links concussion treatment to functional performance such as the ability to work or go to the store, she said. Vision therapy, which is typically offered by optometrists or other specialists who have a certification in vision therapy, is more exercise based, she said.
“Although doctors may have referred patients to us for vision problems, we work on multiple things at once,” she said, “such as eye-hand coordination, eye-motor coordination, and balance.”
Convergence insufficiency. One common problem Ms. Waskiewicz sees in concussion patients is convergence insufficiency, which often causes eyestrain and headache. “We try to train the eyes to team up more efficiently so they’re able to hold close views for longer periods of time.”
She prescribes 2 exercises. In one, patients insert the tip of a golf tee into a straw; in the other, they put pegs into a pegboard. Patients are encouraged to continue the exercises at home. Ms. Waskiewicz also incorporates tasks integral to the patients’ work. For example, a carpenter might practice gently hammering a nail, or a nurse might practice giving injections to oranges.
Photophobia. “We try to give patients compensatory techniques such as wearing sunglasses or a hat,” said Ms. Waskiewicz. “We also educate them about using computer tint screens and changing contrast and brightness levels.”
It may help for patients to slowly expose themselves to light, said Dr. Moss, or to experiment with colored lenses that block out bothersome wavelengths. “We should also ensure they don’t have dry eyes, which might make them even more sensitive to light.” In addition, she said, antidepressant, antiepileptic, or migraine medications may help relieve symptoms of photophobia, even though they don’t treat the underlying problem. (For more on photophobia, see the 2-part MD Roundtable in the November and December 2015 issues of EyeNet.)
Problems with smooth pursuit. For pursuit problems, Ms. Waskiewicz works with patients on tracking moving objects. “I’ll darken the room and have patients use a laser pointer to follow a flashlight as I move it around a wall. And I try to give them things they can realistically do at home on a daily basis.”
Vestibular rehabilitation. This is an exercise-based therapy offered by occupational or physical therapists to improve balance and dizziness after a concussion. It addresses vestibular problems when the brain receives abnormal signals about the position and movement of the head in space.6
On the Horizon
In the future, vision assessment may play a more central role in the evaluation of concussion. Here’s a sample of tests and treatment that are in investigational stages.
NODe. Michigan State University is currently working with the Brien Holden Vision Institute in Australia to see if computer-generated neuro-ophthalmologic testing can be of value, said Dr. Kaufman. Potentially used as a day-after test, the Neuro-Ophthalmic Device (NODe) measures how the eye responds when a patient watches targets on a screen. “It records visual memory, several types of saccadic movement, and smooth pursuits to see if these can be correlated with diagnosis of mTBI,” said Dr. Kaufman.
3-D vision rehab. At Penn State University, Semyon M. Slobounov, PhD, is using immersion in a computer-generated 3-D world, with goggles, to stimulate the vestibular-ocular system in depth, said Dr. Kaufman. “This might identify changes that are consistent with mild concussion that would otherwise be missed, and possibly help with rehabilitation. It stresses the visual system a bit more than other tests and, therefore, might tease out even more subtle abnormalities.”
Neutral density filters. Research is also being conducted to see whether specific types of filters can be more helpful than ordinary sunglasses in relieving discomfort from photophobia following mTBI, said Dr. Kaufman.
___________________________
1 Zhang AL et al. Orthop J Sports Med. Published online Aug. 16, 2016. doi:10.1177/2325967116662458.
2 Ventura RE et al. Semin Neurol. 2015;35(5):599-606.
3 Kawata K et al. JAMA Ophthalmol. 2016;134(7):763-769.
4 Ventura RE et al. Lancet Neurol. 2014;13(1):1006-1016.
5 SCAT 3 (Sport Concussion Assessment Tool, 3rd ed) and Child-SCAT 3. http://bjsm.bmj.com. Accessed Oct. 3, 2016.
6 Vestibular Rehabilitation Therapy (VRT). www.vestibular.org/understanding-vestibular-disorder/treatment/treatment-detail-page. Accessed Sept. 26, 2016.
Meet the Experts
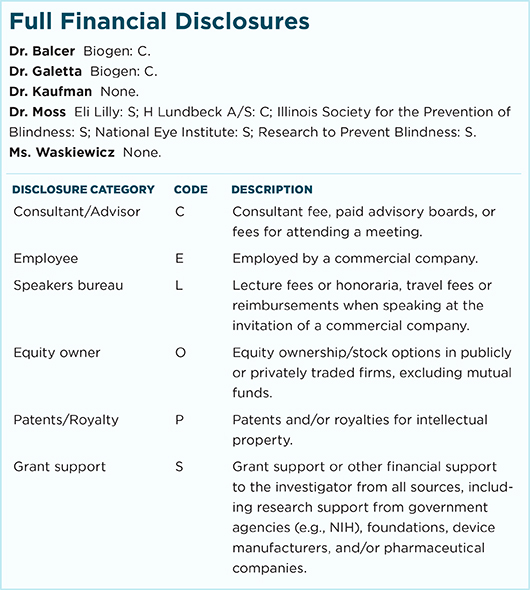
Laura J. Balcer, MD, MSCE Professor and vice chair of neurology and professor of neurology, ophthalmology, and population health at NYU School of Medicine in New York City. Relevant financial disclosures: None.
Steven L. Galetta, MD Professor and chair of neurology at NYU School of Medicine in New York City. Relevant financial disclosures: None.
David Kaufman, DO Professor and chair of neurology and ophthalmology at Michigan State University in East Lansing, Mich. Relevant financial disclosures: None.
Heather E. Moss, MD Director of the neuro-ophthalmology service and the neuro-ophthalmology fellowship program and assistant professor of ophthalmology at Illinois Eye and Ear Infirmary in Chicago. Relevant financial disclosures: None.
Margaret A. Waskiewicz, MS, OTR/L Occupational therapist at NYU Langone’s Concussion Center in New York City. Relevant financial disclosures: None.
For full disclosures and the disclosure key, see below.
|
Photo Credits
(Page numbers refer to print edition.)
Page 44. This image was originally published in the ASRS Retina Image Bank. Jason S. Calhoun. Blood in the Anterior Chamber. Retina Image Bank. 2013; Image Number 7739. © The American Society of Retina Specialists.
Page 47. This image was originally published in the ASRS Retina Image Bank. Mallika Goyal, MD. Traumatic Optic Neuropathy. Retina Image Bank. 2012; Image Number 2162. © The American Society of Retina Specialists.
|