This article is from July 2012 and may contain outdated material.
Download PDF
A corneal ulcer is an ocular emergency that raises high-stakes questions about diagnosis and management. Four corneal experts provide a guide to diagnostic differentiators and timely treatment, focusing on the types of ulcers most likely to appear in your waiting room.
When a large corneal ulcer is staring you in the face, time is not on your side. “Despite varying etiologies and presentations, as well as dramatically different treatment approaches at times, corneal ulcers have one thing in common: the potential to cause devastating loss of vision—often rapidly,” said Sonal S. Tuli, MD, associate professor of ophthalmology, director of the cornea and external diseases service, and residency program director at the University of Florida, in Gainesville.
In the early 1990s, when broad-spectrum antibiotics became commercially available, there was a sea change in the treatment of corneal ulcers, explained Elmer Y. Tu, MD, associate professor of clinical ophthalmology and director of the cornea service at the University of Illinois at Chicago. “Before the introduction of fourth-generation fluoroquinolones, every ulcer required referral to a tertiary-care center and the compounding of special antibiotics to treat the lesion,” said Dr. Tu. “But since then, primary-care ophthalmologists can write prescriptions to cure bacterial ulcers, often eliminating the need for referral to a tertiary-care center.”
That doesn’t mean that diagnosing and treating corneal ulcers (ulcerative keratitis) is simple. According to Natalie A. Afshari, MD, associate professor of ophthalmology and director of the cornea and refractive surgery fellowship program at Duke University, maximizing the chances of complete recovery requires first pinpointing the etiology and then tailoring treatment, not just to the condition but to the individual as well.
Diagnostic Approach
Profiling the Ulcer
The number of ulcers seen in clinical practice depends largely on geography. “In the southern United States, corneal ulcers are significantly more common than in northern states because it’s warm and humid, with lots of young people swimming and sleeping in their contact lenses,” said Dr. Tuli. Estimates of annual incidence in the United States range from 30,000 to 75,000.1,2
Categories. Ulcers are primarily divided into infectious and noninfectious categories. Bacterial infections (chiefly Pseudomonas and Staphylococcus) are by far the most common, but other microbes include fungi (molds such as Fusarium and yeasts such as Candida), parasites (Acanthamoeba), and viruses (herpes simplex). Noninfectious ulcers include autoimmune, neurotrophic, toxic, and allergic keratitis, as well as chemical burns and keratitis secondary to entropion, blepharitis, and a host of other conditions.
Talk to your patients. “As clinicians, we sometimes get sucked into taking a quick look at the eye to get the diagnostic process started without really talking to the patient,” said Francis R. Mah, MD, associate professor of ophthalmology and pathology and medical director of the Charles T. Campbell Ophthalmic Microbiology Laboratory at the University of Pittsburgh. “It’s imperative to take a detailed history to help identify the ulcer’s etiology.”
Ask about pain. How does the patient describe the pain? “If a patient says it feels like he has a rock in his eye or got poked in the eye, that foreign-body sensation tells you there’s an epithelial defect, which is a symptom more typical of a bacterial ulcer,” said Dr. Tuli. “If it’s more of ‘a toothache in my eye’ or ‘when the light hits my eye, it really hurts,’ that’s more likely a nonbacterial or noninfectious keratitis.”
And how severe is the pain? If it’s Acanthamoeba keratitis, for example, patients typically complain of far more pain than the physical findings would suggest; if it’s herpetic keratitis, patients usually don’t have pain complaints, even though the appearance would suggest the presence of severe pain, said Dr. Mah.
Consider the context. The clinician should seek clues by asking the patient about environmental or social factors that could be related to the infection. For example, Were you wearing contact lenses when the problem started? Did you wear lenses while swimming or wash them in tap water? Have you been gardening, or have you encountered vegetation or dirt in another activity?
It’s also important to talk about ocular history, in particular, such risk factors as previous herpetic keratitis, ocular surgery, current or recent use of ocular medications, dry eye, or trauma. Systemic diseases, such as diabetes or rheumatoid arthritis, also predispose patients to corneal ulcers.3
“If the patient wears contact lenses, that’s obviously going to be a huge factor in swaying your diagnosis toward infectious keratitis. However, the history and physical exam could reveal a sterile contact lens–associated ulcer caused by the patient sleeping in contact lenses,” said Dr. Mah.
Examine the eye. The physical exam should include measurement of visual acuity, external examination, and slit-lamp biomicroscopy. Bacterial ulcers are typically associated with a large amount of necrotic material and an epithelial defect; other types are generally less necrotic and may have intact overlying epithelium.3
Culture the site. With the advent of fluoroquinolone antibiotics, which can treat both gram-negative and gram-positive species, many clinicians have dropped culturing as part of their diagnostic practice.4,5 Dr. Tuli said that it’s understandable if you don’t culture small peripheral ulcers. But, at the very least, you should always culture central ulcers and ulcers 2 mm or larger prior to initiating therapy. “If you don’t have access to all the culture media of a lab (blood, chocolate, and Sabouraud agar), you can still get valuable information from a Gram stain,” she said.
The site should be cultured even in patients already on antibiotics; it’s still possible to get positive results, Dr. Tuli added. “If you don’t get a positive culture, you have to start considering nonbacterial causes.”
When to Refer
Typically, when comprehensive ophthalmologists see a patient with a corneal ulcer, they reflexively start fluoroquinolones. If the ulcer doesn’t noticeably improve in a couple of days, they refer the case to a cornea specialist or an academic institution.
But there are instances that require immediate referral to a cornea specialist to make sure the patient doesn’t go downhill quickly. For example, if an ulcer is larger than 2 mm, especially if it’s located directly on the visual axis, or if there’s stromal melting, anterior chamber inflammation, or any scleral involvement at all, immediate referral is warranted, said Dr. Mah. Any suspicious or atypical presentation should also be strongly considered for referral.
Bacterial Ulcers
Sometimes the diagnosis is straightforward: A patient presents with a history of contact lens wear and severe pain that started two days ago; there is purulent discharge and anepithelial defect over a round, necrotic ulcer (Fig. 1). This type of presentation practically screams bacterial keratitis, according to Dr. Tuli.
 |
| (1) Typical bacterial (Pseudomonas) ulcer with a necrotic stroma, purulent discharge, and a hypopyon. |
Diagnostic Differentiators
The characteristic presentation of bacterial keratitis includes an acutely painful, injected eye, often accompanied by profuse tearing and discharge and decreased visual acuity. “The patient will often report feeling a large foreign body
in the eye with every blink,” said Dr. Tuli.
Stromal invasion with an overlying area of epithelial excavation is typical, and the lesion may produce mucopurulent discharge. The cornea and/or the eyelids may be swollen, and the conjunctival and episcleral vessels will be hyperemic and inflamed. In severe cases, there may be a marked anterior chamber reaction, often with pus.3
Treatment
Antibiotics: Frequent dosing required. The topical fluoroquinolones gatifloxacin and moxifloxacin are excellent empiric antibiotics. “Immediately after culturing, start putting the antibiotic drops in every 5 minutes for at least half an hour to show the patient how important it is to use the drops as often as possible,” said Dr. Mah. “By putting those drops in yourself, you will, hopefully, impress upon the patient how imperative it is to dose frequently. Compliance cannot be emphasized enough!”
If the ulcer is larger than 2 mm, adding fortified antibiotics to fluoroquinolones ensures eradication of all the gram-positive and gram-negative bacteria. Furthermore, if you have the patient on two antibiotics, you’re much less likely to miss resistant bacteria, said Dr. Tuli. “Tobramycin is a great and cheap medication, which we often use in conjunction with a fluoroquinolone or vancomycin.
“For the first 48 hours, we typically have the patient administer each antibiotic every hour, alternating the antibiotics on the half hour,” said Dr. Tuli. “After 24 hours, we’ll ease up a little at night to maybe every two hours with the two medications five minutes apart, but you have to make sure the patient understands the importance of antibiotics around the clock to prevent a worsening infection by morning.”
Noncompliance leads to failure. The most common reason for unsuccessful treatment of bacterial ulcers is noncompliance, said Dr. Mah. “If the ulcer is very serious or there was a delay in accurate diagnosis and treatment, or if a patient has no support system to help with compliance, consider admitting the patient to the hospital overnight.”
Steroids: Use with care. Although using strong antibiotics will sterilize the ulcer, it won’t control the inflammatory reaction, which can be just as damaging to the cornea as the infection itself, according to Dr. Afshari. As soon as there is evidence that the antibiotic is working (e.g., the epithelial defect is starting to close, or the culture shows sensitivity to antibiotics), using corticosteroids will inhibit the inflammatory response and reduce corneal scarring.
“Think carefully before starting the steroids because a steroid without antibiotic coverage will make the infection much worse,” said Dr. Afshari. “For steroids to be most beneficial, prescribe them while the ulcer bed is still open, usually within the first 48 hours after initiating antibiotic therapy.”
When to question the diagnosis. “Day 1, you do a culture and start a fluoroquinolone. Day 2, you expect the patient to feel at least no worse and, hopefully, a little better. Days 2, 3, and 4, the ulcer should start consolidating and the appearance of the eye should be noticeably improved,” said Dr. Mah. “I have to reassure patients that vision is the last thing to improve. But if you don’t have signs of at least some overall improvement in four to seven days, then start considering atypical causes of the keratitis. This is the time to refer the patient to a cornea specialist.”
Resistant Bacterial Ulcers
If a classic-looking bacterial ulcer isn’t responding to fluoroquinolones, when is it reasonable to suspect antibiotic resistance, in particular, methicillin-resistant Staphylococcus aureus (MRSA)?
MRSA should be considered if a patient develops infectious keratitis in a hospital or nursing home, is immunosuppressed or has previously been on antibiotics without success, or works in a health care environment. Also consider MRSA early in your differential diagnosis if the eye looks especially toxic, said Dr. Mah.
“The key thing with MRSA is that, even though you may not be able to use some of the first-line agents we use today, you may be able to use older agents that have regained some effectiveness,” said Dr. Mah. “You have to culture the infection and look at sensitivities to various antibiotics.”
Bacitracin ointment and drops, sulfacetamide (Bleph-10) in patients who aren’t allergic to sulfa drugs, gentamicin, and even cefazolin are effective.
If older agents don’t work, the medication to turn to is topical fortified vancomycin, said Dr. Tu, which is the last-resort drug reserved for MRSA or any gram-positive resistant bacteria.
|
Fungal Infections
 |
| (2) Fungal ulcer with feathery borders. |
Diagnostic Differentiators
Fungal keratitis is notoriously difficult to diagnose and, according to Dr. Tu, needs to be cultured on special media. With molds, the ulcer has a dull gray infiltrate, and satellite lesions are often present. Initially, molds produce lesions with characteristic feathery, branching borders in the cornea (Fig. 2). However, advanced fungal infection may resemble advanced bacterial keratitis, which can lead to misdiagnosis, said Dr. Tuli.
Ulcers caused by yeast have better defined borders and may look similar to bacterial infections. Yeast infections remain localized, causing a relatively small epithelial ulceration.6 “You can have both foreign-body sensation and light sensitivity, but the eye won’t produce a lot of discharge because the tissue isn’t being damaged,” said Dr. Tuli.
Red flags. A major red flag for fungal infection is agricultural trauma with vegetable matter, according to Dr. Mah. In addition, he suggested that clinicians maintain a high index of suspicion in the setting of contact lens wear and in humid weather conditions.
Treatment
Only one medication is commercially available for fungal keratitis: natamycin, which is usually applied hourly during the day. “Natamycin’s best activity is against Fusarium mold. It has less efficacy against Candida yeast, which we treat with a compounded medication that’s either amphotericin or voriconazole,” said Dr. Tu.
Dosing regimen. Fungal keratitis requires medication for six weeks on average. The dosing schedule doesn’t have to be as aggressive as for bacterial ulcers because fungi don’t replicate as fast as bacteria. “Patients will need to be on medication for so long that you don’t want to exhaust them early on with an intensive schedule, raising the risk of noncompliance,” said Dr. Tuli.
Management of complicated cases. A particularly worrisome risk in infection with fungi, particularly molds, is deep penetration, not only into the cornea but also into the eye itself. If the infection doesn’t resolve, medical options are limited. Because the topical medications do not penetrate deeply, Dr. Tu said that “trying different delivery methods, like injecting the antifungal directly into the stroma to achieve higher concentrations, is one well-documented option.” Corneal transplantation should be considered urgently if there is risk of the infection moving into the eye or adjacent sclera.
Acanthamoeba Keratitis
 |
| (3) Acanthamoeba keratitis showing typical perineuritis. |
Diagnostic Differentiators
“If a patient’s history includes contact lens wear and/or a recent trauma, especially agricultural trauma, I would suspect Acanthamoeba, which is on the rise,” said Dr. Mah.The ulcer appears very similar to herpes simplex keratitis, with epithelial irregularity as well as ring-shaped and perineural infiltrates (Fig. 3). But, in contrast to herpes simplex, the pain level is out of proportion to the physical exam findings.7
Patients with a parasite such as Acanthamoeba are exquisitely light sensitive. “I call it the ‘jacket-over-the-head sign’—they come in wearing two pairs of sunglasses with a jacket over their head because they can’t tolerate any light,” said Dr. Tuli. “This overwhelms any foreign-body sensation they may have in the eye.”
Among patients with Acanthamoeba keratitis, studies show that only about 33 to 45 percent of cultured cases have a positive culture, said Dr. Tu. Alternative methods for diagnosis include confocal microscopy, direct smears, and polymerase chain reaction.
Treatment
There are no FDA-approved medications for treating amoebic infections. “We rely on compounded antiseptics, most often biguanides, specifically topical chlorhexidine and polyhexamethylene biguanide (PHMB),” said Dr. Tu. Although good evidence supports the use of these agents for Acanthamoeba, the organisms are difficult to eradicate, requiring medication anywhere from three months to a year. “Even after treatment, many patients go on to need a corneal transplant,” said Dr. Tu, “either to control the infection or for visual recovery.”
Herpes Simplex Virus Keratitis
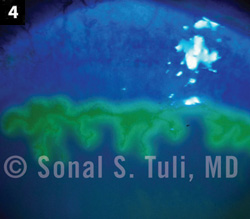 |
| (4) Herpes simplex virus keratitis. |
Diagnostic Differentiators
The characteristic slit-lamp finding in HSV keratitis is a dendritic corneal ulcer (Fig. 4). Loss of corneal sensation is also an important sign, so the clinician should perform a cotton-wisp test. Although patients don’t report a foreign-body sensation or much pain, they are usually photophobic. “You turn the light off, and the patient feels much more comfortable; you put topical anesthetic in the eye, and the patient doesn’t feel a difference,” said Dr. Tuli.
Dr. Mah added that when there is far less discomfort than the physical findings would indicate, you should suspect HSV, especially if the patient has a history of similar episodes.
Types of HSV keratitis. Primary HSV infection typically occurs in children, but the virus persists in the body for a lifetime by becoming latent and hiding from the immune system in neurons. Reactivation is sometimes triggered by fever, exposure to ultraviolet light, trauma, stress, or immunosuppressive agents. In such a recurrence, the virus invades and replicates in the corneal epithelium, causing epithelial keratitis.
HSV can also result in stromal keratitis, which isnot an infection but rather an inflammation causedby the immune response to dead viral particles.
A third type of keratitis associated with HSV is what Dr. Tuli likes to call “a diabetic foot in the eye.” Each time the virus replicates, it bursts out and kills off more nerves that supply the eye, reducing sensation. The resultant hyposensitivity can lead to unrecognized trauma, predisposing patients to neurotrophic keratitis (discussed below).
Treatment
Antivirals. For epithelial ulcers, the mainstay of treatment has been topical antivirals, specifically trifluridine drops (nine times a day) or ganciclovir gel (five times a day). Topical antivirals shouldn’t be used for longer than 10 to 14 days because they kill both normal and infected cells, leading to corneal toxicity.8
Gentle-wiping debridement with a cotton-tipped applicator may benefit epithelial ulcers, as the infected cells come off easily, according to Dr. Tuli. In addition, oral antivirals like acyclovir, valacyclovir, and famciclovir may shorten the course of the keratitis, said Dr. Tu.
Steroids: for stromal keratitis only. The treatment for stromal keratitis is topical steroids. In addition, patients are usually given oral antivirals as prophylaxis to prevent spontaneous recurrence of epithelial disease while the patient is on steroids. However, steroids are contraindicated in epithelial keratitis because they would help the virus to replicate. Conversely, the topical antivirals prescribed for epithelial ulcers are contraindicated in stromal keratitis because they are ineffective (there is no live virus) and may cause toxicity.
Treatment is more complex in patients with herpetic necrotizing keratitis, in which both live virus and an immune response are present. “You have to walk a tightrope trying to figure out which medication to increase and which to decrease,” said Dr. Tuli. Many of these patients end up with long-term problems, including glaucoma and corneal scarring.
Other measures. Because eyes with viral keratitis are prone to superinfections, Dr. Tuli suggested using a daily drop of antibiotic to protect against bacterial infection. In addition, for patients who are immunocompromised or have recurrent or vision-threatening disease, chronic low-dose oral acyclovir or valacyclovir significantly reduces the risk of recurrence.
Noninfectious Ulcers
The appearance of noninfectious ulcers is often quite different from infectious lesions. “Most notably, the underlying cornea is relatively clear, and you don’t see a lot of haze or white blood cells entering the area,” said Dr. Tu.
Sterile infiltrates are typically smaller than 1 mm, gray-white circumlimbal lesions separated from the limbus by about 1 mm of clear space, Dr. Mah said. Some patients are asymptomatic, while others present with mild symptoms of conjunctival swelling, hyperemia, and ocular irritation.
Sterile infiltrates are usually self-limiting and, left untreated, resolve within a week or two. If an ulcer does develop but is less than 2 mm, fairly round, and peripheral, without much stromal involvement or inflammation, it is most likely a sterile ulcer. “These are very responsive to steroids,” said Dr. Mah. “If you’re concerned about a secondary bacterial infection, I recommend giving a day’s worth of antibiotics before starting the steroids.”
Comprehensive ophthalmologists should feel comfortable treating sterile ulcers related to entropion, blepharitis, rosacea, incomplete lid closure, dry eye, and other problems that damage the surface of the cornea as a result of constant friction or drying out. “Fix the underlying problem, and then all you have to do is manage the ulcer supportively with some antibiotics and lubricating ointment,” said Dr. Tuli.
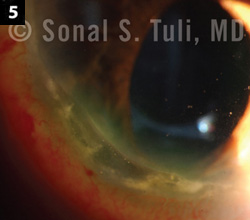 |
| (5) Autoimmune peripheral ulcerative keratitis. |
Autoimmune-related keratitis (Fig. 5) is typically associated with an underlying autoimmune disease such as rheumatoid arthritis or Sjögren syndrome. It’s essential totag-team with the treating rheumatologist to manage the condition, according to Dr. Tu. Moderate to severe ulcers can progress rapidly to melting and perforation. “If a patient has not yet received an underlying diagnosis, the biggest hurdle initially is communicating to the rheumatologist just how serious the ocular condition is and getting him or her on board to treat the patient systemically with potentially life-threatening medications.”
Although systemic immunomodulation is required, some topical measures, such as lubricating the surface, may be helpful, said Dr. Tu. The clinician may also consider using topical cyclosporine to help heal the eye and immunosuppressant drops such as ascorbate to reduce the risk of stromal melting.
Neurotrophic ulcers are associated with many underlying conditions, including diabetes, HSV infection, chemical burns, and overuse of topical anesthetics. The common finding is a decrease in corneal sensation.
A neurotrophic ulcer generally has smooth, thick, gray edges, with minimal inflammation; and hypopyon may be present. Along with poor corneal sensation, there is a decrease in the tearing that is needed to protect the ocular surface; moreover, the damaged corneal nerves endings can’t produce necessary growth factors to help heal the eye. Thus, patients with neurotrophic ulcers have two problems, said Dr. Tuli: repeated minor traumas they can’t feel and impaired healing ability.
Minor neurotrophic ulcers can be managed supportively with preservative-free artificial tears and ointments. Prophylactic antibiotic drops are generally added to the artificial tears. Adjunctive medical and surgical approaches for more serious ulcers are discussed below.
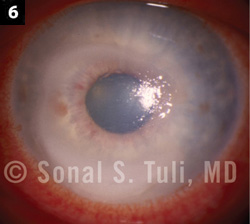 |
| (6) Anesthetic abuse ulcer. |
Topical anesthetic abuse (Fig. 6) is part of the differential diagnosis when the ulcer appears as a disciform, nonhealing epithelial defect. “It shoots up the list if the patient isa health care worker or has been treated for everything but is still not improving,” said Dr. Mah. “It’s a diagnosis of exclusion.” The first step is to eliminate the anesthetics. Dr. Tuli also recommends providing surface support with lubrication, collagenase inhibitors, and bandage contact lenses, as well as treating the inflammation with topical steroids cautiously. However, some patients will go to great lengths to continue using topical anesthetics despite the damage. Psychotherapy may be indicated.
Allergic keratoconjunctivitis comes in two types: vernal (seen primarily in younger males, typically when the weather is hot) and atopic (more typically seen in older women). These can lead to ulcers with significant vascularization and scarring.
“If the ulcer is recognized early, before there’s significant corneal involvement, a comprehensive ophthalmologist can treat it,” said Dr. Mah. Medical management typically includes antihistamines, steroids, and bandage contact lenses. Some reports say topical cyclosporine is helpful, added Dr. Mah, who sometimes uses tacrolimus ointment (Protopic) applied to the lids in especially resistant cases. “Carefully monitor Protopic use because the ointment can lead to some necrosis and skin color changes,” he cautioned.
A patient with significant allergic keratoconjunctivitis usually has other allergic manifestations (such as allergic rhinitis or contact dermatitis) and may already be under the care of an allergist/immunologist. It’s important to work in tandem. To fully treat such a patient, immunotherapy may be necessary; and an allergist/immunologist is far more experienced in administering immunotherapy shots than most ophthalmologists, said Dr. Mah.
More at the Meeting
Don’t miss the symposium on Non-bacterial Infectious Keratitis, a combined meeting with the Cornea Society. It includes eight sessions covering many of the topics in this feature, as well as the 2012 Castroviejo Lecture. (Monday, Nov. 12, 2 to 4 p.m.)
Several relevant instruction courses are also scheduled throughout the Joint Meeting, including:
- Herpes Simplex Keratitis: When Herpes Isn’t a Dendrite, and Vice Versa (Sunday, Nov. 11, 10:15 a.m. to 12:15 p.m.)
- Diagnosis and Treatment Modalities in Cases of Moderate and Recalcitrant Fungal Keratitis (Sunday, Nov. 11, 2 to 3 p.m.)
- Atypical Keratitis (Monday, Nov. 12, 10:15 a.m. to 12:15 p.m.)
- Help! A Corneal Ulcer Just Walked In! What Do I Do Next? (Tuesday, Nov. 13, 2 to 3 p.m.)
|
Adjunctive Approaches
Supporting the surface. Most adjunctive medical and surgical interventions for corneal ulcers focus on providing surface support—with lubrication, collagenase inhibitors, and growth factors—and shielding the cornea. Approaches include bandage contact lenses, punctal occlusion, autologous serum eyedrops, amniotic membrane, and tarsorrhaphy, among others.
In cases of stromal melting, topical collagenase inhibitors such as N-acetylcysteine, doxycycline, or medroxyprogesterone as well as oral vitamin C 1,000 mg per day may be prescribed. Cyanoacrylate glue, a Gunderson (conjunctival) flap, or penetrating keratoplasty may be indicated.
Ultimately, the treatment approach has to be individualized to each condition. Take bandage contact lenses, for example. With an active infection, they’re contraindicated. “You don’t want to hide dirt under the rug, so to speak” said Dr. Afshari. “But, in contrast, we do use bandage contact lenses for neurotrophic ulcers, because those we want to cover to promote healing.”
Managing perforation. When an ulcer perforates the cornea, tissue glue is applied if the defect is less than 2 mm. Otherwise, a partial or penetrating keratoplasty is needed. That said, corneal transplants are not the best option for neurotrophic ulcers. “If the patient can’t heal her own cornea, she’ll have the same problem with a transplanted cornea,” said Dr. Tuli.
Corneal scars can wait. For repairing the scarring caused by a bacterial infection that has resolved, “Time is on our side, unlike during the diagnostic phase,” said Dr. Afshari. “After the infection has resolved and the ulcer has scarred over, we wait to see if the scarring will improve over time. Then we try to improve vision without surgery, with either rigid gas-permeable or scleral contact lenses that encompass the scar and give a new curvature. In selected cases, we do phototherapeutic keratectomy to erase some of the superficial scar, smoothing out the surface.” If these don’t work, lamellar or penetrating keratoplasty is the final step.
___________________________
1 Pepose JS, Wilhelmus KR. Am J Ophthalmol. 1992;114(5):630-632.
2 Jeng BH et al. Arch Ophthalmol. 2010;128(8):1022-1028.
3 American Academy of Ophthalmology. Preferred Practice Pattern Guidelines: Bacterial Keratitis – Limited Revision; 2011.
4 McDonnel PJ et al. Am J Ophthalmol. 1992;114(5):531-538.
5 Rodman RC et al. Ophthalmology. 1997;104(11):1897-1901.
6 http://eyewiki.aao.org/Fungal_Keratitis.
7 Dart JKG et al. Am J Ophthalmol. 2009;148(4):487-499.
8 http://eyewiki.aao.org/Herpes_Simplex_Virus_Keratitis.
Meet the Experts
NATALIE A. AFSHARI, MD Associate professor of ophthalmology and director of the cornea and refractive surgery fellowship program, Duke University. Financial disclosure: Is a consultant for Bausch + Lomb.
FRANCIS R. MAH, MD Associate professor of ophthalmology and pathology and medical director of the Charles T. Campbell Ophthalmic Microbiology Laboratory, University of Pittsburgh. Financial disclosure: Is a consultant for Alcon and Allergan.
ELMER Y. TU, MD Associate professor of clinical ophthalmology and director of the cornea service, University of Illinois at Chicago. Financial disclosure: None.
SONAL S. TULI, MD Associate professor of ophthalmology, director of the cornea and external diseases service, and residency program director, University of Florida, Gainesville. Financial disclosure: None.
|