Download PDF
Many women are becoming pregnant much later in life than was once the case. And with increasing age comes greater susceptibility to health issues, including eye disease. Today, ophthalmologists are caring for a substantial number of women who have glaucoma while pregnant or breast-feeding.
“We are seeing more patients who are of childbearing potential, making treatment a sensitive issue,” said L. Jay Katz, MD, director of the glaucoma service at Wills Eye Institute. Furthermore, he said, “Many patients with congenital, pediatric, or juvenile-onset glaucoma become adults wishing to start a family.”
The challenge in treating this group is balancing the risk to the mother’s vision against the potential harm to the fetus—or to the baby, if the mother is breast-feeding. It is important for ophthalmologists to manage these risks and to understand the unique needs of these glaucoma patients.
IOP in Pregnancy
Dr. Katz noted that intraocular pressure (IOP) often decreases during pregnancy, probably due to shifts in levels of hormones, particularly estrogen. However, in some patients, IOP will increase, he said.
Bhavna P. Sheth, MD, a comprehensive ophthalmologist with a special interest in treating glaucoma during pregnancy, said that clinicians must approach treatment case by case. “It depends on the patient whether the lowering of IOP is clinically significant. If the patient’s disease is mild and early in its course, the ophthalmologist may feel more comfortable taking the patient off the medications and monitoring her intraocular pressures and visual field. But the ophthalmologist might be reluctant to stop medications in a patient with more advanced disease.” She also noted that younger patients with early glaucoma might tolerate small increases in IOP without suffering apparent adverse effects.
Weighing the Risks
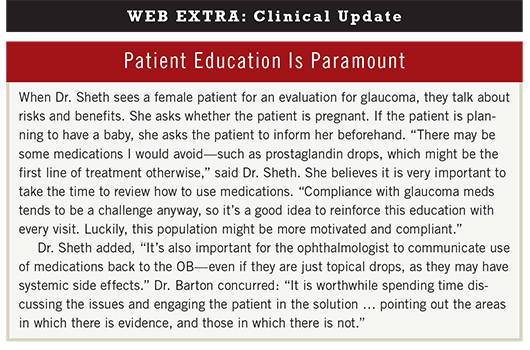
According to Dr. Sheth, weighing the risks to the mother and her child is the biggest challenge with these patients. Based on the level of disease, the ophthalmologist should identify appropriate medications and consider surgery, if needed, to minimize risk to the fetus. “The decision-making process about treatment should have participation from the patient and the obstetrician,” said Dr. Sheth. Patients must be properly educated on the benefits and risks of treatments for glaucoma. (See “Patient Education Is Paramount” below.)
Medications. Dr. Katz emphasized that “all medications for glaucoma get into the bloodstream, placenta, and fetal circulation. You always have the potential for drug exposure. Fetal circulation is very small; even a tiny amount [of a substance] is concentrated for the fetus compared with us. We still don’t know a lot—animal studies are all we have to go on.” Dr. Katz said that many ophthalmologists simply don’t think that using eyedrops is dangerous. But, he cautioned, “Anything the mom puts into her eye is shared.”
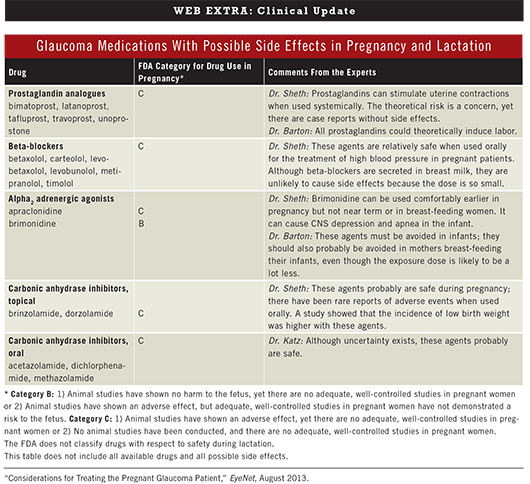
The FDA drug classification system offers guidelines gleaned from human and animal studies. Medications classified as Category B are presumed safe for use in pregnant women. Drugs in Category C may carry potential risks to the fetus, but these risks may be outweighed by potential benefits. (For glaucoma drug category information and comments from the experts, see “Glaucoma Medications With Possible Side Effects in Pregnancy and Lactation” below.)
(click to expand)
As a general rule, the lowest effective dosages of medication should be used, and systemic absorption reduced by using punctal occlusion, eyelid closure for three minutes, and blotting of excess fluid when drops are administered, said Dr. Katz.
Pregnancy. Keith Barton, MD, of Moorfields Eye Hospital in London, said that in pregnant women with glaucoma, timolol is the only drug that he currently uses; it has a long track record of safety, as it has been in use since the 1980s without scares regarding teratogenicity. As another option, he said that “evidence suggests that brimonidine is not teratogenic and therefore relatively safe in pregnancy.”
Dr. Sheth noted that brimonidine, although classified as a Category B drug, can still cause significant adverse effects in the near-term period, such as respiratory and central nervous system depression, and therefore should not be used toward the end of pregnancy. “Near term or during breast-feeding, I suggest topical beta-blockers or topical carbonic anhydrase inhibitors.” However, one study has shown greater likelihood of low birth weight when carbonic anhydrase inhibitors are used, compared with topical beta-blockers.1
Regarding prostaglandin analogues, Dr. Barton said, “There is a good reason to avoid them: They are the same class of drugs used to induce labor.”
Breast-feeding. “Truly, there is no medication for glaucoma that is 100 percent safe,” said Dr. Katz. “Beta-blockers and timolol are measurable in breast milk, and beta-blockers are a concern, as they can drop the baby’s blood pressure and pulse rate.”
Dr. Barton also advised against timolol use in breast-feeding patients, as it could theoretically slow the heart rate or cause bronchoconstriction in the infant, though he said that he is not aware of any reports of this happening. He also expressed caution with brimonidine because it “can cause apnea in the infant, and it is currently not known whether it is secreted in breast milk.”
Dr. Katz noted that prostaglandins metabolize quickly. “Latanoprost may be safest; risk to the child is probably small with breast-feeding,” he said.
Surgery. When it comes to surgery, Dr. Katz treats his patients according to their level of risk. For patients at low risk, he might opt for the watch-and-see approach. “People with elevated eye pressure are at higher risk. The worst possible scenario is a patient who is blind in one eye with glaucoma in the other, on multiple meds controlling her pressure,” he said. “But ideally, we would talk about surgery prior to getting pregnant; this is an extreme.”
Dr. Katz tries to avoid surgery during the first trimester. If IOP spirals to an unacceptably high level, which is not common in Dr. Katz’s experience, he might perform laser trabeculoplasty, or even incisional surgery, using local anesthetic only. “Laser trabeculoplasty is probably not the most effective option; more likely, a trabeculoplasty or a tube shunt will have a higher success rate.” This can be done using topical and local anesthetics, without sedation. Dr. Sheth agreed that it is wise to avoid surgery during the first trimester. “Laser surgery can be done in an office without general anesthesia, but it seems less effective in young patients.”
According to Dr. Barton, surgery only becomes a consideration in cases of severe glaucoma. “In patients with relatively healthy optic discs, a short period of IOP elevation is likely to cause very little long-term damage.”
Dr. Barton noted that surgery during pregnancy is performed with the patient under local anesthesia, and he emphasized that logistics are important. “I recently performed a Baerveldt implant in a patient in the third trimester, and the major issue was whether the patient could comfortably lie flat for the duration of the procedure. In fact, she successfully did, but this might have been a big issue.”
Cesarean Section
Whether to perform a C-section is a question that Dr. Barton has been asked by patients and obstetricians. “If the patient is tending toward a C-section, then I have no objection from the glaucoma point of view. It is more difficult if the patient asks if she should have a C-section because of her glaucoma. There is no evidence to suggest she should; however, one might expect that a lot of pushing and Valsalva-type activity might compromise an optic nerve if it is already severely damaged, in which case most patients will be concerned about the risk of visual loss and, in my experience, more likely to ask for a C-section. In reality, this has only been a serious concern in my practice in patients with severe glaucoma in one or both eyes.”
A caveat for all deliveries. A major concern for Dr. Katz is ensuring that blood pressure does not drop too low during delivery. He warned, “With blood loss, or dropping blood pressure, I would be concerned about a large drop in ocular perfusion pressure. The mom in delivery must be kept hydrated, and in rare instances, transfused.”
___________________________
1 Ho JD et al. Br J Ophthalmol. 2009;93(10):1283-1285.
___________________________
Keith Barton, MD, is a consultant ophthalmologist in the glaucoma service at Moorfields Eye Hospital in London. Financial disclosure: Is a consultant for Alcon, AqueSys, Ivantis, and Refocus; receives lecture fees from Allergan and Pfizer; serves on the advisory boards of Alcon, Alimera, Amakem, Glaukos, Kowa, Merck, and Thea; receives grant support from Alcon, Allergan, AMO, Merck, New World Medical, and Refocus; and has an equity interest in AqueSys and Ophthalmic Implants.
L. Jay Katz, MD, is director of the glaucoma service at Wills Eye Institute and professor of ophthalmology at Jefferson Medical College in Philadelphia. Financial disclosure: Is a consultant for Alcon, Allergan, Amorphex, Bausch + Lomb, Glaukos, Merck, Sensimed, and Sucampo; receives lecture fees from Alcon, Allergan, Lumenis, and Merck; receives grant support from Aerie, Alcon, Allergan, Bausch + Lomb, Glaukos, Lumenis, Merck, and Pfizer; and has an equity interest in Glaukos and Mati.
Bhavna Sheth, MD, is a comprehensive ophthalmologist and professor of ophthalmology at the Medical College of Wisconsin in Milwaukee. Financial disclosure: None.