This article is from August 2012 and may contain outdated material.
Download PDF
When a contact lens wearer comes into your office reporting chronic red eyes and irritation, where do you begin?
The cause of the problem may not be immediately clear, said Deborah S. Jacobs, MD, medical director at Boston Foundation for Sight and assistant clinical professor of ophthalmology at Harvard Medical School. Many factors can contribute: These include lens characteristics, such as fit and materials; patient behavior, such as wearing regimen and adherence to care instructions; and ocular or systemic conditions, such as dry eye and underlying allergies. Another important consideration is the disinfection and storage solution used by the patient.
“You have to be a medical detective,” she said. “Some doctors may take an empiric approach, advising patients to discontinue all lens wear. However, spending some time sorting this out can pay big dividends for both you and your patients.”
Delayed Reactions
If patients develop eye irritation after months or more of smooth sailing, a likely culprit is the solution they use. Such delayed hypersensitivity reactions were more common with earlier cleaning and soaking solutions that contained the mercury-based preservative thimerosal, said Bruce H. Koffler, MD, of the Koffler Vision Group in Lexington, Ky.
“However, it has also been seen with solutions containing other preservatives, such as chlorhexidine and benzalkonium chloride,” he said. “Even a nonallergic person who is subjected daily to any form of chemical, solution, or eyedrop has the potential for developing a delayed hypersensitivity reaction.”
But, Dr. Jacobs added, “Patients with a history of atopy, allergy, eczema, or prior contact lens–related problems will be more easily triggered into sensitivity or an allergic reaction.”
Complex solutions. “As solutions became more complex and were designed to do a variety of things—disinfecting, conditioning, lubricating—more ingredients were added,” she said, which increased the potential for reactions. “After checking fit and regimens, the clinician would gradually conclude that maybe the solution was the ‘bad guy.’”
With the advent of multipurpose solutions (MPSs) around the year 2000, many patients made a switch to these formulations, opting for the greater convenience of a single bottle. That’s when Anne E. Fung, MD, of Pacific Eye Associates in San Francisco, started noticing a growing problem among her patients. “Some who had been wearing their contact lenses for a long time with no problem were suddenly unable to wear them,” she said.
Incompatibility. Another change that occurred in the past decade was the introduction of new silicone hydrogel materials—which offer high oxygen permeability—for soft contact lenses. This had some unanticipated consequences.1
“We just assumed they would do well,” said Dr. Koffler, “but we found that certain combinations of solutions and silicone hydrogels weren’t the most optimal mixture.” There were reports of increased staining and sterile infiltrates in the periphery, secondary to increased inflammation at the limbal juncture between the sclera and cornea, he said. “It became obvious that either the lens material or solution needed to change to enhance biocompatibility.” Today, he said, companies are doing a better job of testing solutions against a variety of silicone hydrogel contact lenses.
Evaluating Solution Sensitivity
Diagnosing hypersensitivity reactions involves a thorough history and inspection of the conjunctiva in order to recognize patterns of ocular signs and symptoms, said Dr. Fung. In addition to being red, the eyes may be constantly weepy, itchy, and irritated, making it difficult for the patient to continue with lens wear, she said. The reaction is diffuse and involves bulbar and palpebral conjunctiva (Fig. 1), with or without a follicular reaction, said Dr. Koffler.
|
What's the Cause?
|
 |
|
Generalized injection of bulbar conjunctiva and eyelid margins in a contact lens wearer.
|
Recognize the type of conjunctivitis. With allergic conjunctivitis, the conjunctiva may have a gelatinous appearance, said Dr. Fung. “Allergic conjunctivitis looks different from giant papillary conjunctivitis [GPC],” she said, “which produces 0.3- to 0.4-mm papillae on the bulbar conjunctiva and is a common, sometimes mechanical, reaction to contact lens wear.” (See Fig. 2.)
 |
|
LOOK UNDER THE LIDS. GPC may be caused by an immune response to irritants or mechanical factors.
|
Listen to the patient. Dr. Jacobs finds she learns more about the source of the problem if she first lets patients describe it in their own words. Then she follows up with questions about contact lens history, as well as wear, replacement, and solution regimens.
Physicians sometimes don’t elicit enough information, said Dr. Koffler. “Find out what contact lens material the patient is wearing and how long they’ve been wearing it,” he said. “Is it disposable, daily wear, frequent replacement daily wear, occasional extended wear, extended wear—or even overextended wear?”
Check the lens in situ. Although many ophthalmology offices delegate the initial part of the examination to technicians, Dr. Jacobs prefers to examine the patient before lens removal. “I check the fit and look for deposits and other signs,” she said, “and then I have the patient remove the lenses to examine the ocular surface, looking for dry eye and for active or prior GPC under the lids.”
Everting the upper lid and grading any GPC is an essential part of this exam, added Dr. Koffler. Ruling out fit problems, he said, involves checking for limbal injection where the conjunctiva and cornea meet. Here, too-tight lenses can have a hypoxic effect and even lead to limbal stem cell insufficiency, if allowed to progress.
Assess corneal staining. The exam may include slit-lamp observation with fluorescein dye to assess corneal staining due to cytotoxicity from solutions or other factors. To enhance the fluorescein, Dr. Koffler recommends using a Wratten #12 filter. Although some slit lamps have this type of color filter built in, clinicians with other models can obtain it through photography stores and ophthalmic instrument distributors. “This brings up staining that can be missed when looking only with the cobalt blue light,” he said.
Solving Sensitivity Problems
If the lenses fit properly, sensitivity to the lens material, solution, or deposits may be the problem, said Dr. Jacobs.
Quiet the eyes. Whatever the source of irritation, the first step is to have the patient temporarily cease contact lens wear while the physician gains control of the reaction, said Dr. Koffler. If infiltration or ulceration is apparent, topical antibiotics may be in order; he initially avoids steroids in case a bacterial or viral infection is involved.
Depending upon the seriousness of the condition, Dr. Koffler sees the patient back within one to four days. If the patient is improving, he either maintains antibiotic therapy or introduces a mild topical steroid, depending on whether the response currently appears to be more infectious or inflammatory. “Mast cell stabilizers and decongestant drops may also be useful at this time,” he said.
For patients with allergic conjunctivitis, Dr. Fung has found that temporarily discontinuing contact lens wear and detoxing the eye with preservative-free tears quickly clears up the reaction in many patients. “In a week, they feel much better.”
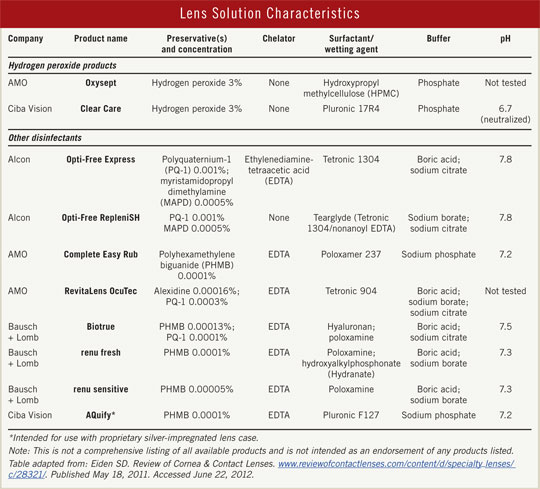
Reassess. Once the eye is quiet, what are the next steps? One option is to switch to an MPS with different ingredients or to a hydrogen peroxide– based regimen (see “Lens Solution Characteristics”). A change of contact lens material or regimen may also help. If you suspect an allergy but aren’t sure the solution is the culprit, you can suggest the patient see a dermatologist and undergo patch testing, said Dr. Koffler.
(click to expand)
Teach proper lens care. “I also use this opportunity to have the technicians teach more about contact lens care,” said Dr. Koffler. This includes rubbing, rinsing, and disposing of lenses as directed; wiping out cases with a tissue; and not topping off solutions.
Although many patients use a so-called no-rub MPS, both the FDA and the Academy—along with other eye associations—recommend the rub-and-rinse method even with these solutions. It may be helpful to direct patients to lens care information available at EyeSmart, which includes a video demonstrating proper lens cleaning and storage with MPS products.
Consider H2O2. In patients with sensitivity reactions, Dr. Fung has had excellent results by simply switching to a hydrogen peroxide–based solution. For someone prone to hypersensitivity or allergy, Dr. Jacobs recommends this option at the outset. Atopic patients are five times more contact lens intolerant, added Dr. Koffler, so they require special attention.
Because hydrogen peroxide is caustic, these overnight lens-care regimens include both cleaning and neutralizing phases. In general, one-step regimens use a platinum-impregnated disk contained in the lens case to neutralize the hydrogen peroxide, while two-step regimens require the user to add a catalase neutralizing tablet to the disinfecting solution in the lens case. In either process, the resulting chemical reaction breaks down the hydrogen peroxide into water and oxygen. “In the morning the peroxide is gone, so the patient puts only pure saline into the eye,” said Dr. Fung.
Dr. Koffler advises colleagues to alert their patients to follow the directions in the solution’s package insert precisely, particularly in regard to the neutralizing component. Otherwise, the hydrogen peroxide may not be converted, causing pain and an acute keratoconjunctivitis.
Suggest daily disposables for some problems. Another good choice for patients who are prone to allergy is use of daily disposable lenses, which come in sterile, preservative-free packs. This eliminates a host of potential problematic variables such as chemicals in the MPS, lens protein deposits, and patient noncompliance around lens and case care. Costs have come down, putting them in the range of a dollar a day, said Dr. Koffler, which makes this a financially acceptable alternative for many patients.
Partner with patients. Consider all the sources of chronic contact lens irritation, said Dr. Fung. “The contact lens solution often matters—it’s as simple as that.”
For patients struggling with reactions, it can be tempting to simply tell them to stop wearing lenses altogether, added Dr. Jacobs. But it pays to put in a little more effort. “If you take an interest in the entirety of the patient’s eye health and visual and optical needs, you can develop a lifelong relationship.”
___________________________
1 Carnt NA et al. Arch Ophthalmal. 2009;127(12):1616-1621.
___________________________
Dr. Fung is a consultant for Alcon, Genentech, Ista, Santen, Sequenom, and Thrombogenics and receives grant support and lecture honoraria from Genentech. Dr. Jacobs reports no financial interests. Dr. Koffler is on the speakers bureaus for Alcon and Bausch + Lomb.