By Lori Baker-Schena, MBA, EdD, Contributing Writer, interviewing Lama A. Al-Aswad, MD, MPH, Malik Y. Kahook, MD, and Michael A. Kipp, MD
Download PDF
Until recently, Michael A. Kipp, MD, rarely thought much about the need for a telemedicine program in his practice. That changed on Wednesday, March 18, when the Academy recommended that ophthalmologists cease providing any treatment other than urgent or emergent care.
Rapid Response
Dr. Kipp, a pediatric ophthalmologist, and his colleagues at the Wheaton Eye Clinic in Wheaton, Illinois, immediately started evaluating their schedules, assessing which patients needed to be seen and which could be rescheduled.
From idea to implementation. Two days after the Academy’s alert, Dr. Kipp—after reading numerous professional social media posts and emails about the potential of telemedicine—suggested that the practice implement a teleophthalmology program. Shortly thereafter, he was appointed head of the practice’s new Telemedicine Committee, which by Saturday morning had developed a game plan for approval by the board of directors. By the following Wednesday, Dr. Kipp had created comprehensive worksheets on navigating Medicare’s recent section 1135 telemedicine waiver and coding different patient scenarios. He developed new coding and billing documentation for the practice using guidelines from the Academy (see “Resources for Getting Started”) and the American Association for Pediatric Ophthalmology and Strabismus.
“None of the 32 doctors in our practice was familiar with telemedicine,” Dr. Kipp said. “We truly started from ground zero. In less than a week, with tremendous guidance from the Academy and subspecialty societies, we had created a telemedicine program.”
A variety of virtual visits. In the first week, Dr. Kipp conducted five telemedicine visits for various conditions, among them a 2-year-old who was checked for strabismus.
“The mother was worried about her child developing a lazy eye,” Dr. Kipp said. “She also is an emergency room nurse who had been exposed to patients with COVID-19, so I preferred not to bring her into the office. I was pleased that we were able to obtain a fairly compliant evaluation on the video screen and that I could determine that there was no obvious lazy eye problem. As a result, I felt that we could safely wait a month or two before having her child fully evaluated in the office.”
 |
|
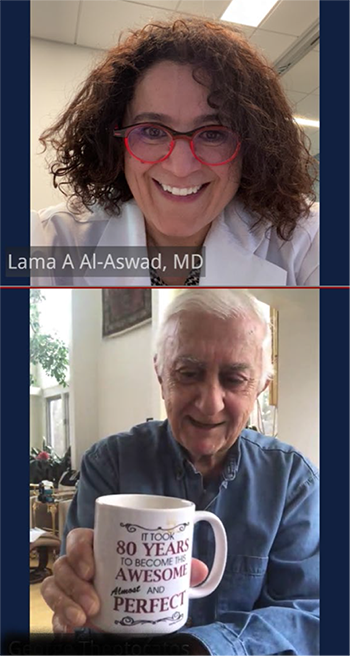
A VIRTUAL VISIT. Dr. Al-Aswad and an 82-year-old patient use the Epic Haiku mobile app that was developed collaboratively by NYU and Epic.
|
A Technology Whose Time Has Come
For glaucoma specialist Lama A. Al-Aswad, MD, MPH, at NYU Langone Health in New York City, this shift to telemedicine is welcome and long overdue. Well before the COVID-19 outbreak, Dr. Al-Aswad was running teleophthalmology projects in an effort to reach more patients who lacked direct access to ophthalmologists.
Valuable in mobile screenings. Her passion for glaucoma prevention in high-risk populations inspired a study in which 8,547 individuals were screened on the streets of New York through telemedicine techniques using mobile equipment.1 Among the screened individuals, 2,118 (25%) were deemed glaucoma suspects; and 52% of those who were followed up were confirmed to have the disease.
More recently, Dr. Al-Aswad developed a mobile screening program in New York City that offered free screenings for glaucoma, cataracts, macular degeneration, and diabetic retinopathy. The program, which used a telemedicine van and a secure data-capturing system, was able to obtain visual fields, anterior and posterior segment optical coherence tomography (OCT) images, and fundus photographs. The data were shared immediately with an offsite physician, followed by a teleconference with the patient to discuss the results and next steps. In addition, Dr. Al-Aswad piloted the first teleophthalmology kiosk in 2019 to screen for the four leading causes of blindness in New York City.
Benefits and impediments. An advocate for telemedicine, Dr. Al-Aswad observed that recent advances in technology and artificial intelligence could help address the incidence of disease underdiagnosis and the predicted shortage of physicians in the future. Both ophthalmology and health care at large could benefit from finding ways to care for patients apart from the traditional office setting.
However, the widespread adoption of telemedicine had been stymied by government regulations involving the lack of codes for telemedicine, the inability to practice telemedicine across state lines, and strict HIPAA restrictions. The arrival of COVID-19 has—at least for now—changed that.
Resources for Getting Started
The Academy’s coronavirus hub page, aao.org/coronavirus, has a link to practice management resources from the American Academy of Ophthalmic Executives, aao.org/practice-management/resources/coronavirus-resources. Here you will find links with lots of information, including the following:
Telemedicine Considerations Tip Sheet
aao.org/practice-management/article/coronavirus-telemedicine-telehealth-considerations
Includes advice on getting started, a checklist for when and how to conduct a telemedicine session, Medicare telehealth FAQs, and more.
Telehealth Resources
aao.org/practice-management/telehealth
A road map to all Academy-produced resources designed to help practices safely and smoothly transition to telehealth environments.
Coding for Phone Calls, Internet, and Telehealth Consultations
aao.org/practice-management/news-detail/coding-phone-calls-internet-telehealth-consult
Recorded overviews of telemedicine options; clinical vignettes for 99202, 99212, and 99213; checklists, at-a-glance information, and more.
Cybersecurity
aao.org/practice-management/cybersecurity
Hackers are taking advantage of the COVID-19 pandemic’s increased burden on the health care system. How to protect your practice and patients.
|
Changes in Response to COVID-19
CMS eases access. On March 6, 2020, the Centers for Medicare & Medicaid Services (CMS) broadened access to Medicare telehealth services under the section 1135 waiver authority and Coronavirus Preparedness and Response Supplemental Appropriations Act.2 Under the new policies, Medicare can pay for telehealth visits whether the patient is in a health care facility or at home when seen. If a patient has Medicare Advantage or commercial insurance, the visit may include a co-pay, co-insurance, deductible, or be considered a non-covered service. It’s important to make patients aware of this potential cost.
More e-communication platforms allowed. Dr. Kipp added that the Department of Health and Human Services has loosened its requirements regarding HIPAA-compliant platforms during the pandemic. This allows physicians to use their discretion in communicating with patients through non–public-facing platforms such as Skype, Zoom, Doxy.me, and Google Hangouts.3 Notably, the doctor may conduct video visits from his/her home.
“While these interfaces have limited capabilities—for example, you can’t do a retina exam at this time—at least in my field we can identify lazy eye, follow vision problems, track patching progress, and look at lesions on the eyelid or red eye,” Dr. Kipp said. “There are several printable eye charts that allow patients to check their visual acuity at home and apps with near-vision eye charts that patients can download. These tools can help in conducting a virtual examination by teleconference.”
Challenges for Setting Up a Telemedicine Program
“My main advice when creating a telemedicine program is to bring in every resource you can find,” Dr. Kipp said. “The Academy is an excellent source of information [see “Resources for Getting Started”]. Also, reach out to your colleagues. Without a doubt, we can learn from each other.”
In addition to Academy resources, Malik Y. Kahook, MD, at the University of Colorado School of Medicine in Aurora, sought information from health care facilities across the country that use the Epic electronic health record (EHR) system to learn how they implemented virtual health for ophthalmic care.
“While we brought together a small internal group that could gather, analyze, and disseminate this information with the rest of our department, our health care system [UC Health] was proactive in educating our attending doctors through Zoom meetings on how to start a virtual health visit and how to document and bill for each encounter,” Dr. Kahook noted.
“It took 10 days to train 1,000 surgeons to use virtual health across our system, and it took our department around the same time to get the majority of our faculty trained on the basics of shifting our practices toward virtual care when possible,” he added.
Consistent terminology. One key to communicating both within our department as well as with colleagues across the globe is knowing what each of the telemedicine terms mean, said Dr. Kahook. Specifically, while his department uses the broad term virtual health to mean any type of communication (phone, video, email, text) used in caring for a patients or answering health questions, “telemedicine” is more focused on the phone or video conferencing with a patient. “There are many other terms that we are learning as we go along,” he added.
Patient selection. A challenge with starting a telemedicine program is determining which patients and conditions are most amenable to virtual health. Dr. Kahook and his colleagues asked each of the department’s service leaders to identify patient categories that would benefit from video-based visits. For example, red eye, post-op blepharoplasty checks, conjunctivitis symptoms, and questions about medication use can easily be moved to virtual health. In contrast, glaucoma visits requiring IOP measurement and visual field testing are not as appropriate for virtual visits.
Education for rapid deployment. Another challenge has been finding resources that provide clear and concise educational information that the faculty and department can rapidly adopt and deploy in their practice. “We often have had to create our own path and are documenting each workflow and standard operating procedure so that we can share with other Epic users,” Dr. Kahook said. “My colleague Cara Capitena-Young championed much of this work, and we are open to sharing all that we are producing.”
 |
|
ONSITE VIRTUAL HEALTH. The patient (not pictured) checks in and is escorted, along with her husband, to the exam room. The tech, in a nearby room, talks with the husband, who is the family historian, by phone. The tech will enter the room to perform necessary testing with as little talking as possible.
|
Putting Telemedicine Into Practice
Early in the COVID-19 outbreak, Dr. Al-Aswad realized that telemedicine would be an optimal way to take care of many patients. “I want to applaud NYU, which had been doing virtual urgent care in its emergency department for a few years,” she said. By mid-March, NYU had rolled out telemedicine protocols to all departments. She said, “Prior to this, we had created telemedicine protocols specific for each subspecialty in the department and criteria for face-to-face visits.”
Glaucoma. “We are looking at glaucoma patients, and this is not optimal as of right now in terms of checking pressure,” she continued. “But what we can do is check on the patients, look at the front of their eyes, and check vision and Amsler grid when needed. We are currently developing an app to better evaluate our patients remotely and are sending those patients who require close monitoring an iCare tonometer to measure their pressure at home.”
Retina. Retina also has telemedicine challenges, and some retina specialists are finding creative solutions. (See Letters.)
Age is no limit. Dr. Al-Aswad dispels the perception that older patients do not have the tech skills to participate in telemedicine visits. On one recent day, she had virtual visits with an 85-year-old woman and an 82-year-old man and was amazed at how savvy they were. “We must not assume that older patients cannot handle telemedicine visits. They will surprise you.”
Be aware of the patient’s overall health. Dr. Al-Aswad added, “The most important piece of advice I can give is to approach telemedicine as a physician first, and then as an ophthalmologist —especially while we are coping with this pandemic. Taking a thorough history is of vital importance, not only for ophthalmic conditions but also to determine patients’ overall health and ascertain whether they have other conditions that may need to be addressed.”
Conducting a Video Visit
Physical Environment
- Private, quiet, professional space; no clutter.
- Ensure background noise, such as traffic, pets, and other sounds that may be heard in your environment are not audible during the visit. Close any doors and shut windows.
- Sit in front of a simple background.
Attire
- Business casual attire with solid color shirts and blouses.
- Avoid stripes, checks, and patterns as they can create visual distraction for your patients.
- Avoid sparkling jewelry, which may be reflective on camera.
Devices
- Make sure all devices have a full charge and/or are plugged in before starting the visit.
- Set up headset, if using one.
- Close out of all other programs.
Punctuality
- Aim to see patient on time and be aware of the scheduled start and end times.
|
Planning Ahead
Dr. Kahook said that he is planning how to manage the backlog of patients caused by cancellation of all nonurgent appointments.
Satellite clinics. With the hospital disrupted by COVID-19, he is considering satellite clinics. “We will schedule several patients to get IOP checks, along with visual fields and OCT if needed, with our technicians taking the lead in performing these duties.
“This will be followed by a virtual health visit with a doctor to review IOP and testing among patients who span a wide geographic area,” he said. “This will work best for patients who are very stable and were due for routine six-to 12-month visits. For all patients who require more intensive care, we will need to find times for them to come in for more traditional visits with the treating physicians.”
New procedures. Another workflow that Dr. Kahook’s department has adopted to protect technicians and physicians is called “onsite virtual health.” It can be used at any type of facility. Once the patient is checked in, the visit proceeds as follows:
- The patient is escorted to the room by a technician and the door is closed.
- The technician goes to the tech station and calls the patient’s cell phone to ask the rooming questions, note the history of the present illness, and discuss other points as appropriate.
- The technician enters the room to perform necessary testing and exits the room with as little talking as possible.
- The doctor can talk to the patient and conduct the history by phone before entering and performing the exam.
- The discharge instructions can be given over the phone as well.
“This practice workflow minimizes face-to-face time and allows for efficient documentation,” Dr. Kahook explained. “The visit is billed as usual without using telemedicine codes. We will likely continue this workflow for all patients with potential communicable diseases beyond the time of COVID-19.”
Pearls for Implementing Telemedicine
As a physician on the front lines of implementing a telemedicine program, Dr. Kahook shared his pearls as of April 1. Reflecting on the rapidly changing nature of the pandemic, Dr. Kahook said that, within two more weeks, “I promise the list will be three times as long.”
- Find resources to read and digest quickly.
- Contact others who are using the same EHR system and who adopted virtual health before you did so you can learn from their successes and mistakes.
- Start with basic phone call visits and transition into video visits while learning the processes.
- Simplify billing workflows for the physician and have billing teams to support these efforts. Doctors should not be expected to be billing experts for these complex situations.
- Identify virtual health superusers who can support the team. In Dr. Kahook’s department, the superusers group includes two or three physicians and four or five administrative/technical staff. Billing supervisors are also needed to support the entire enterprise in the early days of implementation.
- Continue to take notes and update the team weekly about new learning and any glitches in the system.
|
Future Directions
For Dr. Kahook and his department, the transition to telemedicine, while a major undertaking, has brought a high level of cooperation and camaraderie. “I have found all of my partners to be proactive, hardworking, and very helpful in this entire process,” he said. “We have had very little pushback because everybody understands that a change in practice patterns is both necessary and here to stay for the long term.” He predicted that virtual health will continue to play a major role in ophthalmology across all subspecialties and practice locations “even after COVID-19 has been vanquished.”
Dr. Al-Aswad called the adoption of telemedicine in response to the COVID-19 pandemic a “game-changer” for clinicians around the world. “More and more technology will become available to better reach patients in the comfort of their homes, and this will become a large part of how we practice medicine in the future,” she said.
Beyond that, Dr. Al-Aswad envisions a time when teleophthalmology, in combination with artificial intelligence and centralized data management, will promote maximum efficiency and effectiveness in the practice of ophthalmology.
___________________________
1 Al-Aswad LA et al. Cogent Medicine. Published August 2017. https://doi.org/10.1080/2331205X.2017.1367059.
2 www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet.
3 www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html.
___________________________
Dr. Al-Aswad is professor of ophthalmology, vice chair for innovation, and director of Teleophthalmology, Artificial Intelligence, and Innovations at NYU Langone Health in New York City. Financial disclosures: Aerie: C; Globechek: O; Topcon: L,S; Verily: C; Zeiss: S.
Dr. Kahook is professor of ophthalmology and The Slater Family Endowed Chair in Ophthalmology at the University of Colorado School of Medicine and vice chair of translational research, chief of the Glaucoma Service, and codirector of the glaucoma fellowship at the University of Colorado Sue Anschutz-Rodgers Eye Center in Aurora, Colo. Financial disclosures: Alcon: P; Aurea Medical: O,P; Equinox: O; Fluent Ophthalmics: O,P; Ivantis: O; Johnson and Johnson Vision: P; New World Medical: P; ShapeTech: O,P; SpyGlass Ophthalmics: O,P.
Dr. Kipp is a pediatric ophthalmologist practicing at the Wheaton Eye Clinic in Wheaton, Ill. Financial disclosures: Wheaton Eye Clinic: O; Dupage Eye Surgery Center: O; 2015 Realty: O; Naperville Raymond Realty: O; Northwestern Medicine at Central Dupage Hospital: C.