By Annie Stuart, Contributing Writer, interviewing Zélia Maria Corrêa, MD, PhD, J. William Harbour, MD, and Prithvi Mruthyunjaya, MD, MHS
Download PDF
Because of the COVID-19 pandemic, the Academy now recommends that ophthalmologists provide only urgent or emergent care. In this environment, ocular oncologists face unique challenges. “Some of the tumors we treat are potentially fatal,” said Zélia Maria Corrêa, MD, PhD, at Johns Hopkins University in Baltimore. “But many of our patients are also immunocompromised from cancer treatment, which increases their risk of contracting COVID-19.”
Triage. “How long can we delay evaluation and treatment, especially when we don’t know how the crisis will pan out? And what about the ‘invisible casualties’ that might result from denying or delaying care if we fail to prioritize correctly?” she asked.
To provide a snapshot of the approaches in the field, J. William Harbour, MD, at the Bascom Palmer Eye Institute in Miami, surveyed 25 members of the Collaborative Ocular Oncology Group (COOG).1 “We hope the survey provides insights about real-world practice patterns at a time when evidence is limited,” said Dr. Harbour, “to help build consensus for a subspecialty that’s small in numbers but is treating complex, rare conditions.” This EyeNet article reflects the practices of the majority in the COOG survey and adds commentary from three of the group’s members.
 |
|
RETINOBLASTOMA. Telemedicine can be challenging in ocular oncology, especially for intraocular tumors that cannot be easily photographed remotely with a smartphone. For example, it was clear from this external photo that there was an abnormal pupillary reflex (left), but it was not possible without EUA with indirect ophthalmoscopy to confirm that this abnormality was caused by a retinoblastoma (right).
|
Practice During Pandemic: Evolving and Variable
“We’re all trying to do what’s best for our patients, but every hospital or university system is addressing these challenges in different ways,” said Prithvi Mruthyunjaya, MD, MHS, at Stanford University Medical Center in Palo Alto, California. The challenges are evolving and differ from one region to another, he said. “Clinic capacity, staffing, and imaging expertise may all be moving targets affecting when patients can be seen,” he said. “We are all getting used to ‘pre-rounding’ to assess urgency and disease severity for our established patients and learning as much as possible about our new patients so we can postpone as many visits as possible.”
Decisions will be based, in part, on the extent and acuity of disease, as well as the availability of personal protective equipment (PPE), supplies, and staff, said Dr. Harbour. “With limited resources,” added Dr. Mruthyunjaya, “we don’t want to tax the system if other patients have higher priority.”
However, it’s important to ensure that urgent patients aren’t unnecessarily delayed due to fear of infection, he said. Rather than faxing or mailing in referral requests as is typically done, it’s advisable for ophthalmologists seeing new patients with a suspected ocular tumor to contact an ocular oncologist and properly “hand off” coordination of care. This may also provide an opportunity to initiate additional testing locally, said Dr. Mruthyunjaya.
Contingency plans. There’s also the ever-present elephant in the room: If the ocular oncologist gets sick, what to do? “We may be able to offer telemedicine if we aren’t hospitalized,” said Dr. Corrêa. “But it’s a good time to think about a contingency plan. When dealing with ocular tumors, you need a backup or two in case patients need to be seen and you’re not able to do it.”
Candidates for Telemedicine
Because rules about the use of telemedicine have been relaxed for COVID-19, ocular oncologists are seeing patients remotely. “Although I may not be able to see the fundus during a telemedicine visit, by carefully taking a history and going over the symptoms, I feel I can gauge a lot of what is going on with the patient,” said Dr. Corrêa. Dr. Mruthyunjaya noted, “Documenting phone calls and telemedicine encounters in the medical record is essential.”
Ocular surface tumors. Because they are on the external surface of the eye and do not progress rapidly, ocular surface tumors such as conjunctival melanoma, conjunctival squamous cell carcinoma, and conjunctival lymphoma are great candidates for telemedicine—whether through an official telemedicine encounter or the patient emailing you photos, said Dr. Harbour.
Other types of tumors. Telemedicine can also be helpful when assessing symptoms in patients with intraocular tumors, said Dr. Harbour. “You may be able to defer the initial in-person exam if patients don’t have visual loss or other symptoms.”
Get patients on video and ask how their vision is doing, advised Dr. Corrêa. “Ask them to write down the smallest letter they can see and show it to you on video. This gives a rough idea of who needs to be coming in within the next month or so, and it can be reassuring to the patient.”
To avoid unnecessary visits, you may be able to screen most benign tumors before the patient comes into the clinic, said Dr. Mruthyunjaya. “Let’s be clear, families coming into health care facilities increase the risk of exposure, and we don’t know the full extent of how children respond to this virus. Minimizing exposure for both families and clinic staff can help keep everyone safe.”
Fore more about how to get started with telemedicine, see “COVID-19 Moves Telemedicine to the Forefront,” and aao.org/practice-management/telehealth.
|
Patients With COVID-19
How would you deal with a patient who has tested posted for COVID-19? “Except for the very young kids, I would usually prioritize systemic treatment and wait to treat the ocular tumor later,” said Dr. Corrêa.
Dr. Mruthyunjaya has one COVID-19-positive patient who needs an enucleation. “Even though I have full assurances that I can perform the surgery any time I want, I’m looking across the entire system,” he said. “I don’t want to tax the use of PPE or unnecessarily expose hospital staff. Ophthalmologists, scrub nurses, anesthesiologists, PACU nurses—everyone is a vital link in the chain. If any link needs to get pulled due to exposure, the whole chain gets weakened.” After a long discussion with the medical oncologist and others in ophthalmology, anesthesia, and surgery, Dr. Mruthyunjaya is delaying the patient’s surgery by a few weeks while carefully watching his status. “It’s a great example of multidisciplinary decision-making that went to the highest levels for just one patient—and it’s appropriate at this time.”
|
Pediatric Patients
One of the biggest challenges during the pandemic is that children must come in with their parents, said Dr. Mruthyunjaya. “If the child’s mother is under isolation or is COVID-19–positive, your institution may set rules to protect the OR team and other staff. That may impact when children are seen, and care may be delayed beyond what is ideal.”
“And, if a child is sick or has a fever,” said Dr. Harbour, “many institutions may now require testing for COVID-19 before admission to the hospital, even for cases considered urgent.” For example, Johns Hopkins currently has a strict policy of only one family member accompanying a minor, said Dr. Corrêa, and this family member is also screened and tested for COVID-19 before walking into the OR pre-op area.
“All my recommendations are based on the assumption of healthy, nonexposed children,” said Dr. Mruthyunjaya. “But there will be scenarios where children need to be treated, even though they are at higher risk. That’s where conversations with the entire OR team—and maybe even an ethics consult—may be needed.”
Retinoblastoma. Retinoblastoma cases are the most challenging for ocular oncologists right now, said Dr. Harbour. “Most other ocular tumors will not threaten the survival of the patient if there is a delay in care of a month or two, but with retinoblastoma, such a delay could be life-threatening.” These cases also require exams under anesthesia (EUA), which necessitates intubation, a procedure that increases risk of spreading COVID-19 to health care workers, he said.
Children with suspicion for retinoblastoma. “I still see any child with a suspicion of retinoblastoma as quickly as possible, regardless of age,” said Dr. Corrêa. “I also obtain an MRI of the brain and orbits within a week or so to look for optic nerve invasion, orbital extension, and intracranial involvement.”
New patients and active disease. Nearly 100% of COOG survey respondents would manage new patients and patients with active disease within the last three months as per their normal protocols. “If the child’s eye has any other abnormalities such as proptosis or pain, then it is more of an emergency,” said Dr. Corrêa.
Follow-up visits. Dr. Mruthyunjaya is prioritizing—often in concert with systemic treatment—cases that have had intervention in the past three months. “I’m trying to keep them under the same follow-up plan as previously, which is typically every three- to four-week EUAs and any necessary treatment.”
Of survey respondents, 60% would delay EUAs or office visits for a few weeks in patients who have previously stable disease (e.g., no prior treatments or changes for more than three months). Factors such as age or laterality would not change their management decisions, according to the survey. “Regardless, we are all keeping close track of these patients,” said Dr. Mruthyunjaya. “We don’t want to ‘forget’ any of these kids or lose them to scheduling neglect.”
A change in treatment protocol? “Normally, we can save most eyes with unilateral retinoblastoma using intra-arterial or intravenous chemotherapy,” said Dr. Corrêa. “During the pandemic, however, I would tend to promptly enucleate if I think the child has very limited visual potential. We don’t know how long this crisis will last or how reliably the child would be able to return for frequent follow-up exams and treatment. I would rather keep the child healthy and lose the eye.”
Dr. Mruthyunjaya agrees that difficult decisions may be required. “But they are rarely made in isolation and should include a multidisciplinary discussion with the pediatric oncologist or a virtual tumor board, when available,” he said.
Benign tumors. Benign ocular tumors can include hemangiomas, osteomas, and hamartomas, some of which may occur in the setting of systemic syndromes such as Sturge-Weber, neurofibromatosis types 1 and 2, and other conditions.
Remote assessment. “Many of these patients are good candidates for telemedicine in the short term,” said Dr. Harbour. “Usually these tumors are not life threatening, and only rarely is prompt intervention required.” (See “Candidates for Telemedicine.”)
“It is even more important to get as much information as you can by talking to the referring physician, reading all prior clinic notes, and looking at any old imaging studies like photos or OCT,” said Dr. Mruthyunjaya. “Reviewing this information with the family via phone or video visit may allow you to offer your opinion and expected treatment course. More importantly, you can reassure them that you will still care for their child, but the safest thing might be to cautiously delay their evaluation for the time being.”
New patients and follow-up. “With suspected benign tumors that you have not previously evaluated yourself, the concern is always whether or not the referring doctor got the right diagnosis,” said Dr. Harbour. Still, most ocular oncologists would delay the initial evaluation by one to four weeks and follow-up visits by more than four weeks. However, if visual symptoms are present, most would see the patient sooner.
Where a definitive diagnosis is not yet established, Dr. Mruthyunjaya would consider an office visit. “It could be something malignant if you haven’t checked.” If no images are available that are clearly consistent with a benign condition like a retinal astrocytic hamartoma, Dr. Corrêa would still consider bringing the patient in promptly to rule out a retinoblastoma.
 |
|
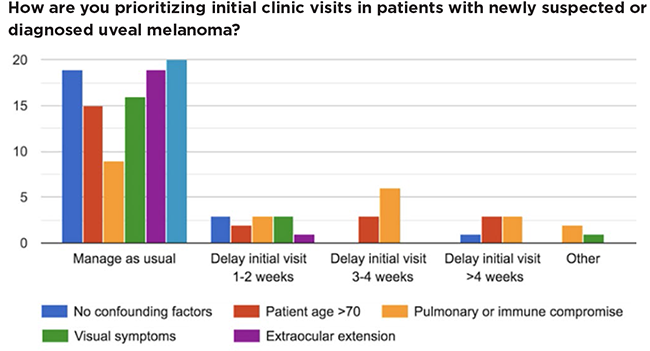
UVEAL MELANOMA. The COOG survey found that most respondents would manage most new uveal melanoma patients according to normal protocols.
|
Adult Patients
In the case of adult ocular tumors, said Dr. Harbour, most ocular oncologists fortunately have a colleague such as a retina specialist who can provide backup to manage patients, at least temporarily.
Uveal melanoma. Uveal melanoma occurs mainly in patients over age 60, said Dr. Harbour. Ocular treatment usually involves plaque brachytherapy or enucleation. “There’s no evidence that delaying treatment for a month or two alters survival, he said, “but you don’t want to wait six months.”
New patients. “For new patients, these are anxious times, and they want to be seen,” said Dr. Mruthyunjaya. “But telemedicine may be an excellent first step. Prior to scheduling an office visit, try to look at photographs, clinical notes, imaging, or other available information. This may allow you to determine that the case does not require immediate treatment.” If a delay is reasonable, outline your rationale to the referring physician and patient, he said, and ask the patient to report any changes in symptoms.
“I do my best to see patients expeditiously—within one to two weeks—if they have extraocular extension or neovascularization with pain, or neovascular glaucoma,” said Dr. Corrêa.
Follow-up visits. It’s important to customize follow-up for each patient, said Dr. Mruthyunjaya. One issue is patients undergoing regular intravitreal injections of anti-VEGF medications for radiation complications. “At least for now, many of us are continuing to do these injections, but they can most likely be safely delayed by four to eight weeks since this is a chronic process,” said Dr. Harbour. If the patient has immune or pulmonary compromise, most survey respondents recommended delaying injections for four weeks or more. “This is something doctors need to evaluate on a case-by-case basis,” added Dr. Corrêa.
High-risk choroidal nevus. “We see a lot of these patients with suspicious choroidal nevi who have borderline clinical features between a benign nevus and a small malignant melanoma,” said Dr. Harbour. “In recent years, there has been an increased tendency to treat these patients more promptly, hoping to reduce their risk of metastasis,” he said, “but this an unproven theoretical assumption.”
There’s no evidence that waiting for three months to recheck them for tumor growth increases the risk of metastasis, he said. “As a result, I am currently managing most of these patients more conservatively for now, having them come back in two to three months unless growth has already been documented.”
Intraocular metastasis to the eye. Most survey respondents would promptly see new patients with suspected intraocular metastasis from a systemic cancer. However, there are other considerations in this decision process.
“Patients who have metastasis to the eye may have been on systemic chemotherapy, immunotherapy, or targeted molecular therapy,” said Dr. Harbour, and may be immunocompromised from their treatment. “We should use the greatest of care with these patients,” said Dr. Mruthyunjaya.
“Although we occasionally use external beam radiation, laser, or other types of treatment,” said Dr. Harbour, “most of these patients won’t require ongoing regular eye treatment. We often wait a few months to see if the eye tumors respond to systemic therapy before considering ocular treatment.”
Vitreoretinal lymphoma. Frequently involving both the brain and eyes, this highly lethal type of lymphoma may be first diagnosed by ophthalmologists, said Dr. Harbour. Most of these patients are over the age of 65, and they usually receive systemic chemotherapy.
New patients. Most COOG survey respondents would see new patients promptly for initial evaluation of suspected vitreoretinal lymphoma—especially patients with blurred vision or floaters. One challenge of this type of lymphoma is that it may share visual symptoms and clinical features with benign conditions, said Dr. Mruthyunjaya. Although a diagnostic vitrectomy is often required for diagnosis, these patients could first get nonsurgical evaluations including blood tests to rule out simulating conditions, MRI, or lumbar puncture, he said. “These tests may take a few weeks to coordinate, which is still appropriate for the patient.”
Follow-up visits. Most patients typically receive external beam radiation or intravitreal chemotherapy injections to treat the eyes, said Dr. Harbour. “At this point, I am more likely to convert patients receiving intravitreal injections to external beam radiation therapy,” said Dr. Corrêa. “Bringing them into the office every four weeks for injections, especially if they’re immunocompromised, is not worth the risk.” If an institution has challenges getting patients in promptly for radiotherapy, she would advise continuing injections until the patient can be treated by radiation oncology.
___________________________
1 https://castlebiosciences.com/wp-content/uploads/2020/03/COOG-Consensus-COVID19_Results_2020-03-26.pdf.
___________________________
Dr. Corrêa is director of ocular oncology and echography services at the Wilmer Eye Institute and professor of oncology and ophthalmology at Johns Hopkins University in Baltimore. Relevant financial disclosures: None.
Dr. Harbour is director of ocular oncology and vice chairman of translational research at Bascom Palmer Eye Institute, and associate director of basic science at Sylvester Comprehensive Center in Miami. Relevant financial disclosures: None.
Dr. Mruthyunjaya is director of ocular oncology and vitreoretinal surgery fellowship at the Byers Eye Institute and associate professor of ophthalmology at Stanford University Medical Center in Palo Alto, Calif. Relevant financial disclosures: None.
For full disclosures and the disclosure key, see below.
Full Financial Disclosures
Dr. Corrêa Castle Biosciences: C; Immunocore: C.
Dr. Harbour Aura: C; Castle Bisociences: C,P; Immunocore: C.
Dr. Mruthyunjaya Aura: C; Castle Biosciences: C; Optos: C; Santen: C; Spark: C.
Disclosure Category
|
Code
|
Description
|
| Consultant/Advisor |
C |
Consultant fee, paid advisory boards, or fees for attending a meeting. |
| Employee |
E |
Employed by a commercial company. |
| Speakers bureau |
L |
Lecture fees or honoraria, travel fees or reimbursements when speaking at the invitation of a commercial company. |
| Equity owner |
O |
Equity ownership/stock options in publicly or privately traded firms, excluding mutual funds. |
| Patents/Royalty |
P |
Patents and/or royalties for intellectual property. |
| Grant support |
S |
Grant support or other financial support to the investigator from all sources, including research support from government agencies (e.g., NIH), foundations, device manufacturers, and/or pharmaceutical companies. |
|