By Lori Baker-Schena, MBA, EdD, interviewing Marc J. Dinkin, MD, Vivek R. Patel, MD, and Prem S. Subramanian, MD, PhD
Download PDF
As the COVID-19 pandemic began, Prem S. Subramanian, MD, PhD, did not anticipate a direct connection between this novel respiratory disease and the neuro-ophthalmic conditions he treated.
“Yet as it became evident that neurological symptoms were being associated with COVID-19, we sat up and took notice,” said Dr. Subramanian, at the University of Colorado in Aurora. And in the ensuing year, neuro-ophthalmologists have identified and reported cases of optic neuritis, visual disturbance and visual loss, cranial neuropathies, and Miller Fisher syndrome in patients with COVID-19.
Dual Research Focus
Even as the science continues to evolve, neuro-ophthalmologists are beginning to see patterns and gain insights from the various case studies that have been reported.
Two current areas of focus in neuro-ophthalmology are the autoimmune cascade that appears to be triggered in the disease, and the vascular problems resulting from the hypercoagulation that seems to be induced by COVID-19, Dr. Subramanian said.
A word of caution. It’s important to not get ahead of the science, Dr. Subramanian cautioned. To date, “there is no direct cause and effect link between COVID-19 and neuro-ophthalmic findings, as COVID-19 cases are so widespread, and some of our findings can be pure coincidence. Our hope is that, as we continue to study these eye conditions, we will better understand if there is a true connection to the disease.”
 |
|
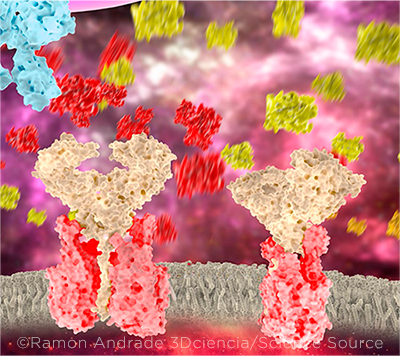
CYTOKINE STORM. Hypercoagulation may be a downstream effect of the cytokine storm that occurs following infection with SARS-CoV-2. In this illustration, the ACE2 receptors (pink and beige) are surrounded by molecules of the cytokines interleukin 1 (IL-1, yellow) and IL-2 (red). One theory holds that the inflammatory process may be driving the incidence of acute cerebrovascular disease in COVID-19 patients.
|
A Matter of Neuroinvasion?
From the beginning of the pandemic, researchers queried whether SARS-CoV-2 directly invaded the nervous system or if a secondary autoimmune process was responsible for the onset of neuro-ophthalmic disease.
There is precedent for the invasion hypothesis, said Vivek R. Patel, MD, at the University of California, Irvine. Animal data showed that both the SARS coronavirus 1 (SARS-CoV-1) and Middle East respiratory syndrome coronavirus (MERS-CoV) could directly access the central nervous system (CNS) through a transsynaptic route, traveling to the medulla and affecting respiration.
“However, with COVID-19, given the millions of cases, if there was a significant neuroinvasion, we would see evidence of this,” Dr. Patel said. “Instead, at this time, we need to look at other explanations of neuro-ophthalmic presentations, and we have two possible explanations: autoimmune dysregulation and hypercoagulation.”
Theory of Immune System Disregulation
According to Dr. Patel, it appears that SARS-CoV-2 itself is not invading the nervous system. Rather, the virus may be triggering an autoimmune cascade—which, in turn, can have a broad array of clinical manifestations depending on the target organ of the autoantibodies. This may explain why patients are presenting with neuro-ophthalmic conditions secondary to immune system dysregulation.
Myelin oligodendrocyte glycoprotein. One such condition is myelin oligodendrocyte glycoprotein (MOG) antibody demyelination, which presents as optic neuritis with severe vision loss. Some investigators have suggested that as many as 50% of cases may be linked to a viral trigger.1
Dr. Patel and his colleagues reported the case of a 27-year-old Hispanic man who presented early in the pandemic with bilateral severe optic neuritis and myelitis and tested positive for the MOG immunoglobulin G (IgG) antibody.1 The patient had reported a few days of progressive dry cough before the onset of eye pain and vision loss.
Although the cough was his only COVID-19–related symptom, it prompted Dr. Patel to order a polymerase chain reaction test for the virus, which came back positive.
However, SARS-CoV-2 was not detected in the patient’s cerebrospinal fluid, suggesting that the virus itself was not directly causing the neurological presentation.
“Interestingly, MOG antibodies can circulate freely but do not exhibit a pathologic effect unless they gain access to the CNS through disruption of the blood-brain barrier,” Dr. Patel said. “In this case, rather than COVID-19 directly invading the brain, the disease may have induced an autoimmune cascade that allowed the blood-brain barrier to be breeched, granting MOG antibodies access to the CNS.”
The patient was treated with intravenous methylprednisolone for five days, followed by an oral prednisone taper. After seven days in the hospital, his visual acuity improved to 20/50 in each eye, which further improved to 20/25 three weeks after discharge with complete resolution of disc edema and retinal findings.
“Given that we believe a viral trigger may be involved in many cases of MOG-associated antibody disease, we wondered whether SARS-CoV-2 could serve as that agent,” Dr. Patel said. “Our patient was the first case of its kind to be reported in the literature.”
Miller Fisher syndrome. Marc J. Dinkin, MD, at Weill Cornell Medical College in New York City, reported the first COVID-19–related case of Miller Fisher syndrome, a variant of Guillain-Barré syndrome, in the United States.2 (The first international case was reported by Spanish investigators.3)
A 36-year-old man presented with left ptosis, diplopia, and bilateral distal leg paresthesias along with COVID-19 symptoms, and an examination was consistent with third nerve palsy. “On day 2, the patient developed the Miller Fisher triad: ataxia, loss of deep tendon reflexes, and progressive worsening of eye movements,” Dr. Dinkin said. After treatment, which included IV immunoglobulin for the Miller Fisher symptoms, the patient was discharged three days later with partial recovery.
“Similar to Guillain-Barré syndrome, Miller Fisher syndrome is an antibody-mediated attack on certain ganglioside proteins within the nervous system, and it typically occurs after a precedent infection. In our case, and in subsequent Miller Fisher cases associated with COVID-19 in the literature, we presume that the virus provoked this immunological response,” Dr. Dinkin said.
Additional nuances. In the same report, Dr. Dinkin and his colleagues presented an additional case of a 71-year-old woman with COVID-19 who presented with painless diplopia. Her case might reflect a direct viral leptomeningeal invasion, for two reasons: The neurologic presentation occurred within two days of the respiratory symptoms, and there was optic nerve sheath enhancement of the involved eye. However, Dr. Dinkin noted, a direct infection of the nervous system was not proven.
Since then, multiple reports of oculomotor, trochlear, and abducens palsy occurring in association with COVID-19 have been reported.
Resources
Updated clinical information on COVID-19 is available from multiple medical institutions, including the Academy (aao.org/coronavirus), the NIH (www.covid19.nih.gov), and Johns Hopkins University (https://coronavirus.jhu.edu). In addition, medical publishers such as Elsevier (www.elsevier.com/clinical-solutions/coronavirus-research-hub) are compiling relevant studies for ease of access.
Here are two resources specific to neuro-ophthalmology:
Journal of Neuro-Ophthalmology COVID Compilation. Drs. Patel and Dinkin serve as associate editors for the Journal of Neuro-Ophthalmology, which maintains a compilation of articles, case reports, and studies pertaining to COVID-19 and its neuro-ophthalmic complications. See https://journals.lww.com/jneuro-ophthalmology/Pages/covid19.aspx.
The NeuroCOVID Project. In January, the National Institute of Neurological Disorders and Stroke (NINDS) launched the COVID-19 Neuro Databank-Biobank. The databank, known as the NeuroCOVID Project, is designed to be a resource of clinical information and biospecimens from patients of all ages who have experienced neurological problems associated with SARS-CoV-2 infection.
The project was created and is now maintained by NYU Langone Health in New York City. It includes information on neurological symptoms, comorbidities, disease course, complications, sequelae, and outcomes. Researchers and clinicians can request access to the database at https://med.nyu.edu/departments-institutes/population-health/divisions-sections-centers/biostatistics/research/nih-neurodatabank-neurobiobank.
|
Threat of Hypercoagulation
Researchers are tracking cases of COVID-19–associated hypercoagulation, which in turn can lead to strokes, with all of their visual manifestations, including homonymous visual field loss and higher order visual disorders.4
Acute cerebrovascular disease appears to be the most common neurologic manifestation of COVID-19, occurring in 2.8% of patients.5 While this includes mostly ischemic stroke, intracerebral hemorrhages and venous sinus thromboses also may occur.
In the New England Journal of Medicine,6 Oxley et al. reported a two-week period in which five patients younger than 50 years presented with new-onset symptoms of large-vessel ischemic stroke. In contrast, during every two-week period in the previous 12 months, the researchers’ health service treated, on average, 0.73 patients younger than age 50 for large-vessel stroke. All five patients in this report had COVID-19.
“The most common theory for this hypercoagulation is that it is the downstream result of the COVID-19 cytokine storm,” Dr. Dinkin said. “However, the binding of SARS-CoV-2 to the angiotensin-converting enzyme 2 [ACE2] receptor on endothelial cells may lead to endothelial dysfunction7 and secondary microvascular infarction.”
What to Look For
The occurrence of an otherwise unexplained cranial neuropathy should prompt consideration of SARS-CoV-2 infection even in patients with mild COVID-19 symptoms, Dr. Dinkin said.
Other signs and symptoms to watch for include the following:
Homonymous visual field loss. This could occur following ischemic stroke or hemorrhage but may also result from posterior reversible leukoencephalopathy syndrome, which has been reported in association with COVID-19.8
Myasthenia gravis. Eight patients have been described in the literature, with a parainfectious autoimmune response mechanism presumed.9
Nystagmus or saccadic intrusions. These may occur from either brainstem strokes or rhomboencephalitis. They also may be related to an autoimmune encephalitis affecting the brainstem, although this is rare.
Optic neuritis without traditional risk factors. Some cases have been associated with the MOG antibody.
Intracranial hypertension. This includes some patients with Multisystem Inflammatory Syndrome in Children (MIS-C) in which multiple organ systems and tissues can become severely inflamed following COVID-19 infection.
Dr. Dinkin treated a young teen who presented with MIS-C and developed severe headaches, papilledema, and an abducens palsy suggestive of elevated intracranial pressure. Fortunately, the syndrome resolved spontaneously.
Verkuil and colleagues reported a similar case,10 and Silva and colleagues described six patients who had COVID-19 and were found to have isolated intracranial pressure.11
Exacerbation of IIH. One of Dr. Dinkin’s patients had a three-year history of mild idiopathic intracranial hypertension (with only pulsatile tinnitus and MRI findings of elevated intracranial pressure but no papilledema). Yet within days of contracting COVID-19, the patient developed grade IV papilledema and visual field loss refractory to medical therapy. She improved with placement of a venous sinus stent.
Proposed mechanism. The underlying mechanism by which the inflammatory state associated with COVID-19 might affect cerebrospinal fluid dynamics remains unclear. One theory involves dysfunction of the spinal fluid–producing choroid plexus, based on the expression of ACE2 receptors in some of its cells.12
Emerging Associations
Dr. Subramanian noted that researchers and clinicians continue to report new neuro-ophthalmic findings related to COVID-19. One of his papers in publication presents a new constellation of conditions in a patient: severe vision loss combined with ischemia of the oculomotor system.
“We have also heard of COVID-19 patients showing up with unusual late vision loss from an optic neuropathy, as well as visual field loss, trouble reading, and so forth,” he said. “Ophthalmologists should consider an association with COVID-19 when they see these patients.”
In for the Long Haul
Dr. Subramanian also predicted that neuro-ophthalmologists will see a disproportionate number of patients with “long COVID,” who are commonly known as “long-haulers,” even as this initial phase of the pandemic subsides.
“These patients, who continue to experience symptoms months after their initial symptoms appear, will need to be seen by neuro-ophthalmologists to exclude either some visual effects or symptoms related to the optic nerve or orbital dysfunction,” Dr. Subramanian said. “It is important to keep these patients on your radar.”
__________________________
1 Zhou S. et al. J Neuro-Ophthalmol. 2020;40(3):398-402.
2 Dinken MJ et al. Neurology. 2020;95(5):221-223.
3 Gutiérrez-Ortiz et al. Neurology. 2020;95(5):e601-e605.
4 Bondira I et al. J Neuro-Ophthamol. In press.
5 Chwalisz BK, Dinkin MJ. J Neuro-Ophthalmol. 2020;40(3):283-284.
6 Oxley TJ et al. N Engl J Med. 2020;382:e60.
7 Ackermann M et al. N Engl J Med. 2020;383(2):120-128.
8 Ghosh R et al. J Neuro-Ophthalmol. 2020;40(4):523-526.
9 Restivo DA et al. Ann Intern Med. 2020;173(12):1027-1028.
10 Verkuil LD et al. Lancet. 2020;396(10250):532.
11 Silva MTT et al. Cephalalgia. 2020;40(13):1452-1458.
12 Pellegrini L. et al. Cell Stem Cell. 2020;27(6):951-961.
__________________________
Dr. Dinkin is associate professor of ophthalmology in the departments of ophthalmology and neurology, director of neuro-ophthalmology, and a Helen and Robert Appel Scholar at the Weill Cornell Medical College in New York City. Relevant financial disclosures: None.
Dr. Patel is professor of clinical ophthalmology and chief of neuro-ophthalmology services at the Gavin Herbert Eye Institute at the University of California, Irvine. Relevant financial disclosures: None.
Dr. Subramanian is professor of ophthalmology, neurology, and neurosurgery, director of neuro-ophthalmology, and vice chair for Academic Affairs at the University of Colorado School of Medicine in Aurora. Relevant financial disclosures: None.
For full disclosures and the disclosure key, see below.
Full Financial Disclosures
Dr. Dinkin None.
Dr. Patel Horizon Therapeutics: L.
Dr. Subramanian GenSight Biologics: C,S; Santhera Pharmaceuticals: S; Horizon Therapeutics: C,S; Invex Therapeutics: C.
Disclosure Category
|
Code
|
Description
|
| Consultant/Advisor |
C |
Consultant fee, paid advisory boards, or fees for attending a meeting. |
| Employee |
E |
Employed by a commercial company. |
| Speakers bureau |
L |
Lecture fees or honoraria, travel fees or reimbursements when speaking at the invitation of a commercial company. |
| Equity owner |
O |
Equity ownership/stock options in publicly or privately traded firms, excluding mutual funds. |
| Patents/Royalty |
P |
Patents and/or royalties for intellectual property. |
| Grant support |
S |
Grant support or other financial support to the investigator from all sources, including research support from government agencies (e.g., NIH), foundations, device manufacturers, and/or pharmaceutical companies. |
|