Download PDF
Many challenges surround HSV ocular disease—from establishing the diagnosis to preventing recurrence. Three experts dispel the myths and share tips to identify, classify, and tackle the disease.
“Masquerader” is the first word that comes to mind for Sonal S. Tuli, MD, when she thinks of herpes simplex virus (HSV) ocular disease. “HSV patients are usually referred to me because their diagnosis is ‘unknown,’” said Dr. Tuli, associate professor of ophthalmology, director of the cornea and external diseases service, and residency program director at the University of Florida in Gainesville. “With the exception of HSV epithelial disease, which is an active infection that can be cultured and has a distinct appearance, there’s no definitive test for diagnosing HSV disease, and the presentation can be misleading.”
Indeed, HSV can appear similar to many other eye conditions—herpes zoster, Acanthamoeba infection, topical medication toxicity, and healing abrasions, to name just a few.1 It frequently is misdiagnosed and has earned the title of the most common cause of infectious corneal blindness in the United States.2
Profile of Ocular HSV
Epidemiology. Each year, about 50,000 new and recurring cases of ocular HSV (predominantly type 1) are diagnosed in the United States.2 HSV can cause disease in any layer of the eye, and common manifestations include blepharitis, follicular conjunctivitis, keratitis, and keratouveitis. (Posterior segment disease, such as acute retinal necrosis, can occur but is uncommon.)
The recurrence rate of HSV eye disease after an initial episode is approximately 27 percent at one year, 50 percent at five years, and 63 percent at 20 years. The risk increases with the number of recurrences.3
Primary infection. By and large, primary herpes is pediatric. It’s a mild infection that goes unrecognized in most children. Initially, the virus enters the eye and travels to the trigeminal ganglion, where it replicates and becomes latent. When it later travels back to the cornea, HSV causes episodic ocular disease, but it remains in the trigeminal ganglion for life.
Recurrent infection. “Recurrent infections are really the crux of herpetic eye disease; this is where major damage can result,” said Dr. Tuli. Proven triggers include UV light, fever, and refractive surgery, but almost every one of Dr. Tuli’s patients cites a different trigger. “One patient insists that it’s chocolate,” she said. Psychological stress, a commonly mentioned culprit, wasn’t found to be a trigger by the Herpetic Eye Disease Study (HEDS) Group, but this type of risk factor is difficult to prove, perhaps because stress is ubiquitous.4
Categorizing HSV Keratitis
“Of all the herpetic ocular diseases, keratitis is where there’s the most confusion and room for harm,” said cornea and external diseases specialist James Chodosh, MD, MPH, professor of ophthalmology at Harvard Medical School in Boston.
Broadly speaking, HSV keratitis can be divided into two types: epithelial disease, usually caused by actively replicating virus; and stromal disease, usually caused by immunologic mechanisms. Making the distinction is paramount because the treatment approaches are very different.
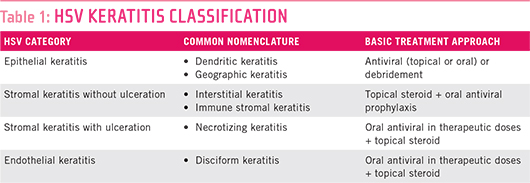
Within the epithelial and stromal groups, HSV can manifest in various ways, and a hodgepodge of terms have been used to describe each presentation. “Residents are constantly confused,” said Dr. Chodosh, who is spearheading a simplified, anatomic classification system that he hopes will get everyone speaking the same language (Table 1). “Ninety-five percent of cases will fall into one of the anatomic categories and should be discernable by any eye care provider, regardless of training level,” Dr. Chodosh said. “Once correctly classified, the treatment algorithms are fairly straightforward.”
(click to expand)
Diagnosing HSV Keratitis
Ocular HSV is often mistaken for common conjunctivitis, so it’s important to make the distinction. (See “Is It Pink Eye or Herpes Conjunctivitis?”)
Dr. Chodosh teaches his residents to make an anatomic diagnosis before doing anything else. He advises them to “identify the layer of the cornea predominantly involved; this will generate the differential diagnoses. Then you can work through those, based on the history, appearance, time course, risk factors, and associated findings.”
Presentation. In epithelial disease, the classic HSV findings are dendriform lesions (dichotomous branching with terminal bulbs). “There’s little else that looks like these tree-branching ulcers,” according to Todd P. Margolis, MD, PhD, professor of ophthalmology at University of California, San Francisco, and director of the Francis I. Proctor Foundation and the Sophie Heintz Research Laboratory at UCSF. “You just have to stain it and be mindful of the physical findings.” The center of the lesion stains with fluorescein; the borders stain with lissamine green or rose bengal.
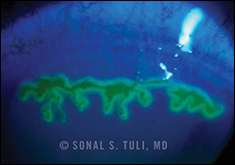 |
| Geographic ulcer in epithelial keratitis. |
“Geographic lesions [sharply demarcated corneal ulcers with scalloped margins] can sometimes be a little more difficult to tell apart from corneal abrasions and healing lines from traumatic events [trophic ulcers],” said Dr. Margolis. “But even the edges of geographic ulcers tend to have a dendriform-like pattern to them. If you stain the cornea, you shouldn’t miss this.” Neurotrophic keratitis presents with rolled-up, smooth, gray edges and only stains centrally with fluorescein, with no lissamine green staining at the edges.
Stromal disease manifests primarily as an inflammatory infiltrate with stromal edema, sometimes with vascularization and/or scarring. If there is no ulceration, stromal disease tends to run a relatively indolent course. When ulceration is present, perforation is a risk.
Reduced corneal sensation. When the presentation is not dendritic, testing for corneal sensation may help to identify HSV. Dr. Tuli said, “Every time the virus replicates in the trigeminal ganglion, it kills the cell in which it replicated. This leads to hyposensitivity.” Dr. Margolis added, “Very few conditions reduce corneal sensation, but, unfortunately, most clinicians don’t test it. If they do think to do so, it’s often only after they’ve put an anesthetic drop in the eye, at which point it’s too late.”
Clinicians often ask Dr. Margolis how to test corneal sensation if they don’t have “one of those devices.” He simply uses dental floss, dangling one tip onto the surface of the cornea to see if the patient can feel it. “It’s extremely valuable for testing corneal sensation, much better than the standard cottonwisp test because you can be very focal. We routinely test five locations: four quadrants and center. We also test sensation over the lesion itself.”
When else to suspect herpes. For stromal disease and endotheliitis, which are primarily immunologic and can’t be cultured, diagnosing HSV can be a challenge. Certain things should raise your index of suspicion. “If a patient is in far less pain than the findings would suggest, think herpes,” said Dr. Tuli. “If a patient is photophobic or has uveitis and high intraocular pressure (secondary glaucoma), think herpes. And always suspect herpes in patients with a history of herpes.”
Is It Pink Eye or Herpes Conjunctivitis?
“We typically do not recognize primary HSV infections because they are mistaken for conjunctivitis,” said Dr. Tuli. When physicians see follicular conjunctivitis, they assume it’s the garden-variety “pink eye” that children get. However, typical conjunctivitis is caused by viruses such as adenovirus, which is almost always bilateral. HSV is almost always unilateral.
Among the population with unilateral conjunctivitis, about 25 percent have herpes, according to Dr. Tuli. But most clinicians don’t think to culture the eye because they assume it’s common conjunctivitis. Because HSV is usually self-limited, few people realize that they’ve had a primary herpetic infection.
|
CLINICAL PEARL:
If a patient presents with unilateral follicular conjunctivitis, culture it because there’s a good chance it’s herpes.
—Sonal S. Tuli, MD
|
If the culture is positive for herpes, Dr. Tuli recommends treatment with oral acyclovir for two weeks. However, it’s controversial whether treating primary infections with acyclovir reduces the amount of virus replicating in the body, thereby preventing subsequent episodes. “We know that if you keep a patient on acyclovir long term, he won’t have a recurrence, yet it’s hard to justify keeping someone on a medication for the rest of his life for pink eye,” said Dr. Tuli. “However, a two-week course may prevent the child from spreading it and may lower his risk of recurrence, and it doesn’t do any harm.”
More important than yielding a treatment regimen, positive HSV cultures identify people who are at risk for recurrent disease. “If you culture it and the infectious agent is herpes, then you can tell the mom, ‘The next time your child has a pink eye, don’t just think it’s ordinary pink eye; bring him in because he could have corneal findings the next time around,’” said Dr. Tuli.
If you don’t have access to a lab that can culture herpes, Dr. Tuli suggests putting a sample on a slide, just as you would for a Pap smear, and sending it for a standard Pap test. Although the presence of multinuclear epithelial giant cells will tell you whether the eye has a virus of the herpes family, it won’t identify the specific type of herpes.
|
If the culture is positive for herpes, Dr. Tuli recommends treatment with oral acyclovir for two weeks. However, it’s controversial whether treating primary infections with acyclovir reduces the amount of virus replicating in the body, thereby preventing subsequent episodes. “We know that if you keep a patient on acyclovir long term, he won’t have a recurrence, yet it’s hard to justify keeping someone on a medication for the rest of his life for pink eye,” said Dr. Tuli. “However, a two-week course may prevent the child from spreading it and may lower his risk of recurrence, and it doesn’t do any harm.”
More important than yielding a treatment regimen, positive HSV cultures identify people who are at risk for recurrent disease. “If you culture it and the infectious agent is herpes, then you can tell the mom, ‘The next time your child has a pink eye, don’t just think it’s ordinary pink eye; bring him in because he could have corneal findings the next time around,’” said Dr. Tuli.
If you don’t have access to a lab that can culture herpes, Dr. Tuli suggests putting a sample on a slide, just as you would for a Pap smear, and sending it for a standard Pap test. Although the presence of multinuclear epithelial giant cells will tell you whether the eye has a virus of the herpes family, it won’t identify the specific type of herpes.
Treatment Basics
Fundamentals. HSV epithelial keratitis (live virus) should be treated with topical or oral antivirals but not with steroids. HSV stromal disease (little, if any, virus) requires steroids with oral (never topical) antivirals as prophylaxis.
Qualifiers. In real life, HSV keratitis is part of a spectrum, and cases don’t always fall neatly into a category. “Every keratitis has a component of both infectious disease and immunologic disease,” said Dr. Margolis. “When you’re dealing with dendrites in epithelial disease, there’s a lot of viral replication and a little bit of inflammation; when you’re dealing with stromal disease, there’s a lot of inflammation and very little viral replication.” Almost all cases require medication changes throughout the course of treatment, with frequent monitoring to maintain the balance among clearing virus, preventing reactivation, and controlling inflammation.
Surgical intervention. Surgery may be needed to correct the damage caused by HSV, but it should be performed only when the eye is quiet.
Managing Epithelial Keratitis, Stromal Disease, and Endotheliitis
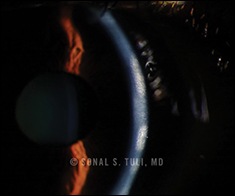
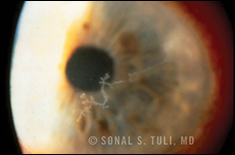 |
| Dendritic presentation of epithelial keratitis. |
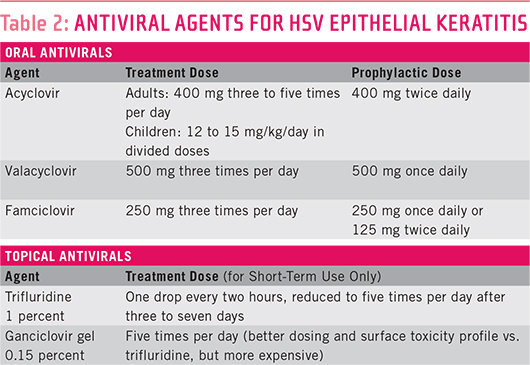
HSV epithelial keratitis. “There are a lot of ways to skin the cat when you’re dealing with epithelial disease,” said Dr. Margolis. “And they pretty much all lead to the same outcome.” You can treat with a topical antiviral such as trifluridine (Viroptic) drops or ganciclovir gel; you can treat with a systemic antiviral (acyclovir, valacyclovir, or famciclovir). Either way, it takes about seven days to heal, he said. (See Table 2.)
Drs. Margolis and Chodosh prefer oral monotherapy. “I use orals rather than topicals because of safety, efficacy, and cost,” said Dr. Margolis. “Many ophthalmologists are more comfortable using topical drugs because they’re not used to prescribing systemic agents. They question whether the systemic drug can get into the eye and do as good a job as a topical agent. But there’s no evidence that the topicals are any more effective, and orals are far safer and less expensive.”
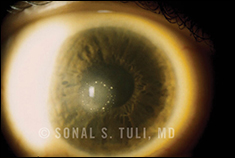
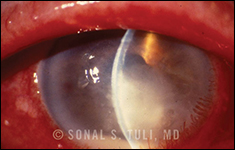 |
| Stromal keratitis with ulceration (necrotizing keratitis). |
Dr. Tuli added a cautionary note on the use of topical antivirals: “I see a number of patients who come in after months of topical antivirals for a ‘nonresponding’ keratitis. This is toxic to the eye and results in scarring. Over 95 percent of dendritic lesions are cured in under two weeks. If it’s past two weeks, either the virus is resistant or the keratitis is no longer infectious, but you’ve created a toxicity that can look very much like the herpes itself. Either way, after two weeks, stop topical antivirals!”
Another option is corneal epithelial debridement. Treatment time is about 2.5 days as opposed to seven. Some people will debride and use a topical agent; some will debride and use an oral agent.
Dr. Tuli favors debridement: “Gentle wiping removes 90 percent of the virus in the eye. Then I treat with topical antivirals—that’s my mainstay, as there is minimal resistance to topical antivirals.” (See Table 2.) If the keratitis is close to the visual axis and the patient has had more than one episode, Dr. Tuli also uses oral antivirals long term to prevent recurrence.
 |
| Stromal keratitis without ulceration (interstitial keratitis). |
Regardless of treatment strategy, epithelial disease in and of itself doesn’t cause a lot of problems, if treated properly. “It goes away, doesn’t leave a big scar, no big deal,” said Dr. Margolis. Stromal disease is where the most damage is done.
HSV stromal disease. The primary treatment for stromal disease is topical steroids in conjunction with prophylactic oral antivirals. Topical antivirals should never be used long term for prophylaxis because they can cause corneal toxicity, but orals can be used safely for substantial periods of time.
According to Dr. Tuli, what you’re trying to do with oral prophylaxis is prevent recurrence in the trigeminal ganglion because if the patient happens to shed virus while on steroids, he or she is going to get a bad infection. “Topical antivirals only treat HSV when it gets to the eye, so topicals are only for acute epithelial disease,” she said.
 |
| Endothelial keratitis (disciform keratitis). |
Although Dr. Margolis likes to start the oral antiviral a couple of days before the steroid, he has initiated them simultaneously in cases of stromal disease without ulceration. “The big problem I find practitioners have with stromal disease is that they have issues with long-term antiviral prophylaxis and the appropriate use of steroids,” said Dr. Margolis.
HSV endotheliitis. Endotheliitis is active virus in the anterior chamber of the eye. “I think of it as having more of an infectious component than typical stromal disease,” said Dr. Margolis, who treats these patients with oral antivirals because he knows these drugs will get into the anterior chamber. “I definitely start these patients on antivirals first, for a couple of days, before starting the topical steroids because I know there’s active virus in the anterior chamber,” said Dr. Margolis. “After starting the steroids, I can usually taper them faster in endotheliitis than in stromal disease with vascularization,” he added. “Endotheliitis patients can typically get off steroids.”
Using Steroids Correctly
When to use them. Steroids shouldn’t be used when there’s active viral replication on the ocular surface (as in acute epithelial keratitis). Other than that, topical corticosteroids (prednisolone acetate 1 percent or prednisolone phosphate 1 percent) are essential for treating HSV stromal keratitis. These agents control inflammation and minimize damage to the eye. You rarely need to use a topical steroid more than four times a day to get stromal disease under control, according to Dr. Margolis.
S-l-o-w-l-y taper the dose. Once inflammation is under control, the goal is to find the minimal effective dose that will keep the eye quiet. “Every time you reduce the steroid, you have to wait four to six weeks to see if the inflammation is completely under control,” cautioned Dr. Margolis. “One of the big mistakes clinicians make is that they tell their patients to use it four times a day, then twice daily, then once daily, and then come on back in to see them. Then they say, ‘Oh, you reactivated.’ But the patient didn’t reactivate; the clinician just didn’t catch the end point when tapering the steroid dose to find the minimal effective dose.” Because these patients have chronic inflammatory disease, it’s very important to bring them back each time the steroid dose is reduced to see if they’re doing well at that lower dose.
Myth: Patients have to get off steroids. Although it’s always preferable to wean patients off topical steroids, many patients, especially if they have corneal vascularization with stromal disease, never get off them, said Dr. Margolis.
Topical steroids should be maintained for as long as necessary. “Some eyes remain quiet only when topical steroids are continued at microdoses,” said Dr. Tuli. More than 50 percent of her patients remain on microdoses for life. These patients are also on chronic oral antivirals.
Using Prophylaxis Properly
After the patient completes a treatment regimen of oral or topical antivirals for seven to 10 days, oral antivirals then serve solely as prophylaxis.
Myth: Prophylaxis must be discontinued after one year. Because HEDS demonstrated the effectiveness of prophylaxis for one year,4 many believe that it cannot be used for more than a year. “It’s just not true,” said Dr. Margolis. Oral acyclovir reduces the severity of stromal disease and the frequency of recurrence for as long as it is maintained.5 “You can prophylax for as long as a patient is alive.”
Dosing. “Ideal dosing of oral antivirals for HSV ocular disease hasn’t quite been figured out, and some clinicians use too little for prophylaxis,” said Dr. Margolis. Prophylaxis requires at least 400 mg of acyclovir two or more times a day (Table 2). “Finding the lowest possible dose of oral antivirals shouldn’t be a worry,” said Dr. Chodosh. “Oral acyclovir is an exceedingly safe drug, safer than Tylenol, for example. If a patient has recurrences on acyclovir 400 mg twice daily, you can increase the dose and/or the frequency.”
When to use it. “If the keratitis is vision threatening and the patient has had more than one episode, I start oral acyclovir and keep the patient on it forever,” said Dr. Tuli. “I have hundreds of patients on chronic twice-a-day acyclovir, some for decades. Compliance is excellent because they know the consequences of going off the antiviral.”
Any patient who is undergoing eye surgery and has a history of HSV should start prophylaxis a few days before surgery and continue it at least until the inflammation has subsided, advised Dr. Chodosh. He added that any patient with a history of HSV who’s anticipating a corneal transplant, or any patient who develops HSV keratitis after a transplant, should be on oral antivirals for life.
When to Refer
“If you don’t see significant improvement within a couple of weeks with a dendrite or stromal keratitis, send the patient to a specialist,” Dr. Margolis recommends. “And if you don’t see significant improvement of endotheliitis within a matter of days, send the patient on.”
___________________________
1 http://eyewiki.aao.org/Herpes_Simplex_Virus_Keratitis.
2 www.nei.nih.gov/health/cornealdisease/#k.
3 Young RC et al. Arch Ophthalmol. 2010;128(9):1178-1183.
4 Herpetic Eye Disease Study Group. Arch Ophthalmol. 2000;118(12):1617-1625.
5 Sudesh S, Laibson PR. Curr Opin Ophthalmol. 1999;10(4):230-233.
Meet the Experts
JAMES CHODOSH, MD, MPH Professor of ophthalmology, Harvard Medical School, Boston. Financial disclosure: Is a consultant for Alcon, Allergan, and the National Eye Institute.
TODD P. MARGOLIS, MD, PHD Professor of ophthalmology, University of California, San Francisco, and director of the Francis I. Proctor Foundation and the Sophie Heintz Research Laboratory, San Francisco. Financial disclosure: None.
SONAL S. TULI, MD Associate professor of ophthalmology, director of the cornea and external diseases service, and residency program director, University of Florida, Gainesville. Financial disclosure: None.
|