Download PDF
Involutional entropion is a troublesome eyelid malposition commonly encountered in elderly patients, with a prevalence reported as high as 2.1% in those aged 60 years and older.1 The condition is characterized by progressive inward rotation of the lower eyelid margin, causing progressive irritation of the ocular surface. Although conservative treatment with ocular lubricants, taping, or botulinum toxin injections can produce temporary relief, surgical intervention is required to definitively restore anatomic positioning.
Etiology
The pathogenesis of involutional entropion is multifactorial. Contributing factors include progressive horizontal laxity of the tarsus and canthal tendons, disinsertion of the lower eyelid retractors, and an overriding preseptal orbicularis. General fat atrophy with enophthalmos and increased appositional pressures during forced lid closure likely also play a role; however, comparison with age-matched controls by means of Hertel exophthalmometry measurements yielded no statistically significant difference.2
Development of involutional entropion is generally attributed to age-related decreases in collagen tensile strength, although there are reports of iatrogenic disinsertion of capsulopalpebral fascia during routine cataract surgery.3 Thus, a thorough history with details of recent mechanical manipulation of the eyelids with lid specula should be part of the routine entropion workup.
Interestingly, involutional entropion and ectropion share clinically and histologically defining features, including retractor disinsertion, horizontal lid laxity, and migration of the orbicularis. In comparison, entropic lower eyelids were found to have more significant capsulopalpebral fascia disinsertion than their ectropic counterparts, while ectropic lids had more pronounced horizontal lid laxity.
Other types of entropion. Other types of entropion have different etiologies; they are classified as cicatricial, congenital, or spastic. Cicatricial entropion is caused by scarring of the conjunctiva and relative shortening of the posterior lamella. This is the result of chronic autoimmune, infectious, inflammatory, thermal, or traumatic insult.
Congenital entropion is a rare condition characterized by shortened posterior lamella, capsulopalpebral fascia dysgenesis, and structural weakness of the tarsal fascia. An unusual form of congenital entropion includes a tarsal kink, in which the upper tarsus is bent, causing the cilia and the eyelid margin to come in direct contact with the globe.4
Spastic entropion develops in response to acute ocular irritation or inflammation. It often occurs in patients with underlying involutional eyelid changes and is further exacerbated by the corneal irritation caused by the entropion.5
 |
|
INVOLUTIONAL ENTROPION. (1A) Ocular irritation is apparent in affected left eye. (1B) Improvement after surgical repair with lateral tarsal strip and lower lid reinsertion.
|
Signs and Symptoms
Symptoms—such as blurry vision, severe discomfort, foreign body sensation, redness, itching, burning, excessive tearing, and discharge—are caused by cilia and keratin rubbing against an unprotected globe. This may result in a persistent epithelial defect, corneal ulceration, and in the worst cases, globe perforation.
Diagnosis
Differential diagnosis. Entropion should be differentiated from epiblepharon (overriding pretarsal muscle), trichiasis (misdirection of eyelashes without entropion), and distichiasis (anomalous growth of eyelashes).
Characteristics of involutional entropion. Diagnosis can be made by identification of involution of the eyelid and lash margin on slit-lamp examination. Diminished tarsal integrity can be detected by the lid snapback test or the lid distraction test.
Inferior capsulopalpebral fascia weakness, a defining anatomical defect in involutional entropion, can be demonstrated by reverse ptosis of the lower eyelid, deep inferior fornix, or diminished lower eyelid excursion on far downgaze. With lower lid excursion, the presence of a visible white line in the inferior cul-de-sac represents a complete retractor disinsertion.
Conservative Management
Artificial tears, lubricant eye ointment, and contact lenses can be used to protect the ocular surface from the mechanical trauma caused by rotated cilia. Lubrication will decrease a secondary spastic component of the entropion.
Tape can be placed parallel to the lower eyelid margin with horizontal tension to decrease horizontal tarsal laxity and allow for eversion of the lid margin. Care must be taken to avoid excessive lid eversion, lagophthalmos, or exposure keratopathy. In addition to cosmetic concerns, excessive taping can cause severe skin irritation.
Although thermal cautery has been used to induce shortening of inferior lid retractors and orbicularis, it is rarely a successful permanent solution.
Botulinum toxin injections have been shown to be a safe and effective temporizing mechanism for patients with an overriding preseptal orbicularis. However, the condition recurs within 8 to 26 weeks, and repeated injections are needed to maintain the therapeutic effect.6
Surgical Treatment
Everting sutures. The Quickert procedure involves everting sutures and is a fast, minimally invasive, low-cost technique to temporarily reinsert lower lid retractors.
In this procedure, a double-armed absorbable suture is inserted into the conjunctival fornix below the lower border of the tarsus to recruit the lower retractors. The suture is directed below the tarsal plate, and then upward to emerge inferior to the lash line to achieve lid eversion.
The use of Quickert sutures as a primary procedure for entropion is controversial, however, because of high recurrence rates. Male sex, severe lower eyelid laxity, and Asian race are risk factors for failure of the repair with Quickert sutures.7 In addition to recurrence, other complications can include bruising, granuloma, and trichiasis.
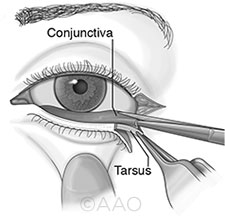
Reinsertion of lower lid retractors. Exploration and reinsertion of the lower lid retractor can be performed through a direct external incision or an internal transconjunctival approach.
In external repair, a subciliary cutaneous incision is made. After the orbital septum is bluntly dissected, the lower eyelid retractors are identified and reattached to the anterior inferior tarsal edge with interrupted absorbable sutures. The skin is then closed over the repair. Reported complications include mild eyelid retraction and pyogenic granuloma.
The internal approach involves a transconjunctival incision below the inferior tarsal border. A conjunctival flap is elevated until the lower eyelid retractors are identified. The retractors are reattached to the anterior inferior border of the tarsus, and the conjunctiva is approximated over the repair. Complications of internal repair include overcorrection with ectropion, in addition to the mild retraction and granulomas that are also reported from repair with the external approach.
Recurrence is slightly more frequent with the internal transconjunctival approach, although the difference is not statistically significant.8 Conservative retractor reinsertion without correction of horizontal laxity can have recurrence rates as high as 17%; however, concurrent horizontal canthal shortening can greatly reduce recurrence rates.9
Lateral canthal tightening. Surgical procedures for tightening lower eyelid laxity include full-thickness partial lower eyelid resection and lateral tarsal strip procedure. Full-thickness lower eyelid resections require a wedge resection and tarsal repair.
In the lateral tarsal strip procedure, after the surgeon performs a lateral canthotomy and inferior cantholysis, the tarsus is isolated from the anterior and posterior lamella to create a de-epithelialized strip of tarsus. The tarsus is shortened and then reattached to the periosteum of the lateral orbital rim.
The lateral tarsal strip procedure restores physiologic lower eyelid tension without causing eyelid margin notching or weakness, which can occur after a full-thickness lower eyelid resection. In addition to recurrence, rare complications of the lateral tarsal strip procedure include chemosis, self-limiting granuloma, and persistent trichiasis without entropion.
Combined everting sutures and lateral canthal tightening. Combined Quickert and lateral canthal tightening procedures have been gaining popularity because of their decreased recurrence rates and low risk of complication.
A small amount of preseptal orbicularis can be removed in patients who have significant override that exacerbates the entropion. Reinserting the capsulopalpebral fascia, tightening the tarsus, and trimming the orbicularis addresses all 3 etiologic factors for involutional entropion. Despite significant improvements, recurrence rates in literature range from 0% (mean follow-up, 18 months) to 9.4% (mean follow-up, 24 months).10 Varying degrees of residual horizontal lid laxity may contribute to differences in recurrence rates.
More Surgical Details
 For more detailed coverage of the entropion repair procedures discussed in this article, consult the Academy’s Basic Techniques of Ophthalmic Surgery, 2nd ed., published in 2015. Available in print and eBook formats, it presents step-by-step instruction and informative illustrations for 81 surgical procedures—and gives you access to 175 video vignettes on key points. Visit www.aao.org/store for further information. For more detailed coverage of the entropion repair procedures discussed in this article, consult the Academy’s Basic Techniques of Ophthalmic Surgery, 2nd ed., published in 2015. Available in print and eBook formats, it presents step-by-step instruction and informative illustrations for 81 surgical procedures—and gives you access to 175 video vignettes on key points. Visit www.aao.org/store for further information.
|
Conclusions
Understanding the anatomy, pathophysiology, and etiologic factors is crucial in diagnosis and management of involutional entropion. Patient age, general health, and preferences must be considered in deciding between more and less invasive management modalities. Many surgical procedures have been described in the literature, with varying recurrence rates. Everting sutures and lateral tarsal strip combined with preseptal orbicularis modification restore lower eyelid anatomy with good surgical result.
___________________________
1 Damasceno RW et al. Ophthal Plast Reconstr Surg. 2011;27(5):317-320.
2 Kersten RC et al. Ophthal Plast Reconstr Surg. 1997;13(3):195-198.
3 Hurwitz JJ et al. Ophthal Plast Reconstr Surg. 1990;6(1):25-27.
4 Dailey RA et al. Ophthal Plast Reconstr Surg. 1999;15(5):360-362.
5 Wies FA. Trans Am Acad Ophthalmol Otolaryngol. 1955;59(4):503-506.
6 Deka A, Saikia SP. Orbit. 2011;30(1):40-42.
7 Jang SY et al. J Craniomaxillofac Surg. 2014;42(8):1629-1631.
8 Ben Simon GJ et al. Am J Ophthalmol. 2005;139(3):482-487.
9 Boboridis K et al. Ophthalmology. 2000;107(5):959-961.
10 Scheepers MA et al. Ophthalmology. 2010;117(2):352-355.
___________________________
Dr. Lo is an ophthalmology resident, and Dr. Glavas is a clinical assistant professor of ophthalmology; both are at NYU School of Medicine Department of Ophthalmology in New York, N.Y. Relevant financial disclosures: None.