Download PDF
Stargardt disease is the most common juvenile macular dystrophy and a frequent heritable cause of central visual dysfunction in young patients. The prevalence of Stargardt disease is between 1:8,000 and 1:10,000.1 Stargardt disease was first described in 1909 by Karl Stargardt. Although further information has been elucidated about the genetics and pathophysiology of Stargardt disease, and improved imaging has led to advances in diagnosis since that time, there is still no effective treatment for the disease.
Pathophysiology
Stargardt disease is most commonly caused by mutations in the ABCA4 gene and is typically inherited in an autosomal recessive fashion, although some autosomal dominant pedigrees have been identified.2 The ABCA4 gene is an ATP-binding cassette transmembrane protein expressed by rod outer segments and is involved in the transport of all-trans-retinal. The mutations in ABCA4 in Stargardt disease result in the accumulation of all-transretinal in the photoreceptors as well as the retinal pigment epithelium (RPE). Subsequent conversion of all-transretinal to N-retinylidene-N-retinylethanolamine (A2E), a component of lipofuscin, eventually leads to lipofuscin accumulation, which is toxic to the RPE and photoreceptors. Of note, ABCA4 mutations are also responsible for other retinal degenerations, including some forms of cone-rod degeneration and certain types of retinitis pigmentosa; and they are linked with an increased risk of age-related macular degeneration.3
Although 95 percent of cases of Stargardt disease are caused by mutations in ABCA4, mutations in ELOVL4, BEST1, and PRPH2 genes are also implicated in its etiology.2
 |
|
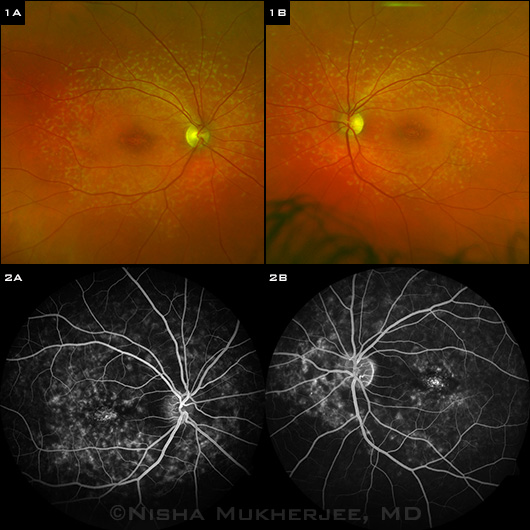
STARGARDT FINDINGS. (1A,1B) Fundus photography shows bilateral atrophic macular changes surrounded by diffuse pisciform flecks. (2A,2B) Fluorescein angiography reveals a dark choroid with hyperfluorescent pisciform flecks.
|
Clinical Presentation
Stargardt disease commonly presents in the second or third decade of life with slowly progressive bilateral visual loss, generally in the range of 20/30 to 20/200.2 The classic fundus appearance of eyes with Stargardt disease is characterized by juvenile-onset foveal atrophy, taking on a “beaten-bronze” appearance, with surrounding distinct yellow flecks that are round or pisciform at the level of the RPE (Fig. 1). These flecks have been shown to follow a pattern of radial expansion from the fovea to the peripheral fundus. The perifoveal RPE atrophy that accompanies Stargardt disease gives the macula a bull’s-eye appearance. As the disease progresses, affected patients can develop extramacular RPE atrophy as well as choriocapillaris atrophy; however, the peripapillary RPE is often spared by an unknown mechanism.2
The presentation, clinical features, and progression of Stargardt disease vary widely from patient to patient. Fundus flavimaculatus is the term for the phenotypic presentation of Stargardt disease in which flecks are widely distributed throughout the fundus. It is important to note that the progression of vision loss does not correlate with the fundus appearance.4
Fishman has described four stages of Stargardt disease based on clinical examination findings as well as ancillary testing (see table).5
 |
|
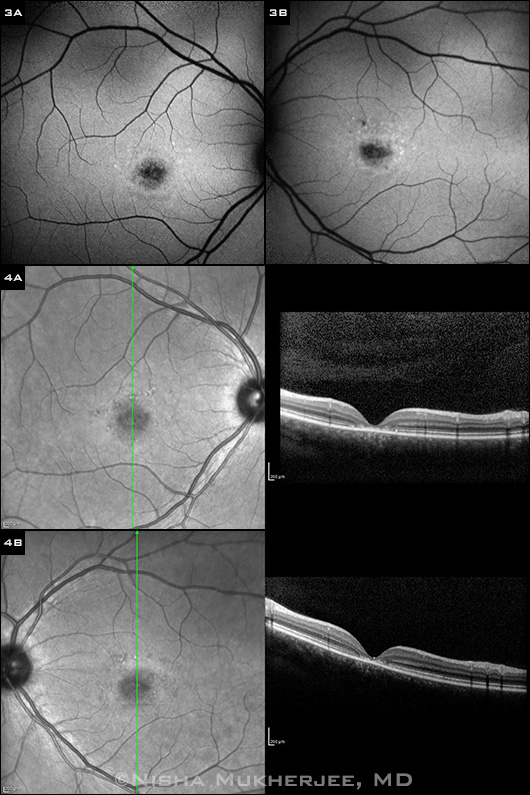
FAF AND OCT FINDINGS. (3A,3B) Fundus autofluorescence photograph shows mottled areas of hyperautofluorescence and hypoautofluorescence, corresponding to areas of lipofuscin accumulation and RPE atrophy, respectively. (4A,4B) SDOCT: Horizontal and vertical sections through the fovea reveal parafoveal disruption of outer retinal layers.
|
Imaging Characteristics
Fluorescein angiography (FA), fundus autofluorescence (FAF), and spectral-domain optical coherence tomography (SD-OCT) can help diagnose and characterize Stargardt disease.
The hallmark finding on imaging of Stargardt disease is a “dark choroid” on FA (Fig. 2). This sign, in which the retinal circulation appears to be highlighted against a hypofluorescent choroid, is present in at least 80 percent of patients with Stargardt disease. It is thought to occur as a result of blockage of background choroidal fluorescence from subretinal lipofuscin.2
FAF in early Stargardt disease reveals hyperautofluorescence in areas of lipofuscin accumulation, which is often the first detectable change on imaging,4 and hypoautofluorescence in areas of RPE atrophy (Fig. 3).
SD-OCT may show disruption or complete loss of both inner and outer photoreceptor segment layers, sometimes combined with thinning of other retinal layers (Fig. 4).
Electroretinogram (ERG) testing is not commonly performed in Stargardt patients. Standard full-field ERGs are typically normal, although both the scotopic and photopic ERG may be decreased in some patients.2 Occasionally, multifocal ERG may be performed to aid in the early diagnosis of Stargardt disease in children.
Prognosis and Management
Just as Stargardt disease presents with marked phenotypic variability, its impact on visual function is highly variable as well. It is known that visual acuity (VA) most often declines to a level of 20/200 or worse, but it usually stabilizes after reaching this nadir.1 Although some patients maintain good VA for many years, others may experience precipitous loss. One study showed that the probability of maintaining a VA of 20/40 or better in at least one eye was 52 percent by age 19, and it decreased to 32 percent by age 29 and to 22 percent by age 39.6
Currently, there is no treatment for patients with Stargardt disease, although research on disease pathophysiology and gene therapy provides hope for future treatment options. Clinical trials involving gene therapy are currently under way.7 Recently published 12-month results from one of the studies showed improvements in visual acuity and quality of life in some Stargardt’s patients.8
Patient counseling. Stargardt patients should be encouraged to maintain good sun protection, as exposure to bright light can lead to the formation of all-trans-retinal in photoreceptors and contribute to lipofuscin accumulation. Some reports have noted dimming of vision in Stargardt patients while smoking, so smoking cessation should be advised. Finally, patients should avoid high doses of vitamin A, which can lead to increased accumulation of lipofuscin and worsening of disease.
___________________________
1 Walia S, Fishman GA. Ophthalmic Genet. 2009;30(2):63-68.
2 Haji Abdollahi S, Hirose T. Semin Ophthalmol. 2013;28(5-6):372-376.
3 Koenekoop RK. Ophthalmic Genet. 2003;24(2):5-80.
4 Chen Y et al. Adv Exp Med Biol. 2010;664:333-340.
5 Fishman GA. Arch Ophthalmol. 1976;94(12):2061-2067.
6 Fishman GA et al. Ophthalmology. 1987;94(7):809-814.
7 Han Z et al. Adv Exp Med Biol. 2014;801:719-724.
8 Schwartz SD et al. Lancet. Published online Oct. 15, 2014. doi:10.1016/S0140-6736(14)61376-3.
___________________________
Dr. Mukherjee is a resident in ophthalmology, and Dr. Schuman is a retina specialist and an assistant professor of ophthalmology; both are at the Duke Eye Center in Durham, N.C. The authors report no relevant financial disclosures.