Download PDF
Although rare, superior ophthalmic vein thrombosis (SOVT) can lead to devastating complications if it is not detected and managed promptly and appropriately.1,2 While the exact pathogenesis of SOVT is unclear, certain factors are known to predispose individuals to this condition (which is not to be confused with superior branch retinal vein occlusion). A high level of suspicion is required to make the diagnosis.
Etiology and Risk Factors
Congestion of the superior ophthalmic vein (SOV) may occur as a result of infection, trauma, inflammation, hypercoagulable states, neoplasm, and orbital crowding.3 In patients with orbital infection, the concurrent orbital congestion can incite an inflammatory cascade that culminates in thrombophlebitis with thrombus formation; alternatively, thrombosis may be caused by direct vascular invasion by the pathogen. Offending bacteria may be aerobic or anaerobic, with Staphylococcus aureus and anaerobic streptococci being the most common causative organisms.1,4
 |
|
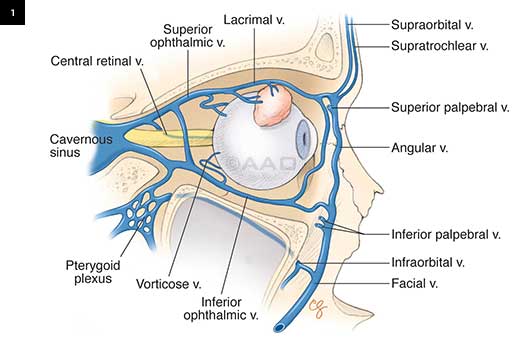
ANATOMY. The superior ophthalmic vein originates in the superomedial orbit, passes through the superior orbital fissure, and ends in the cavernous sinus.
|
Presentation
Patients with SOVT may complain of orbital or facial pain and swelling, double vision, or decreased vision. Clinical findings generally indicate an orbital process and, depending on the specific etiology, may include proptosis, chemosis, ophthalmoplegia, and ptosis. The optic nerve may be affected by compression, with clinical signs of optic neuropathy such as reduced visual acuity, abnormal color vision, and relative afferent pupillary defect.1,4,5
SOVT may progress to cavernous sinus thrombosis (CST), and the patient may have both conditions at the time of presentation.
 |
|
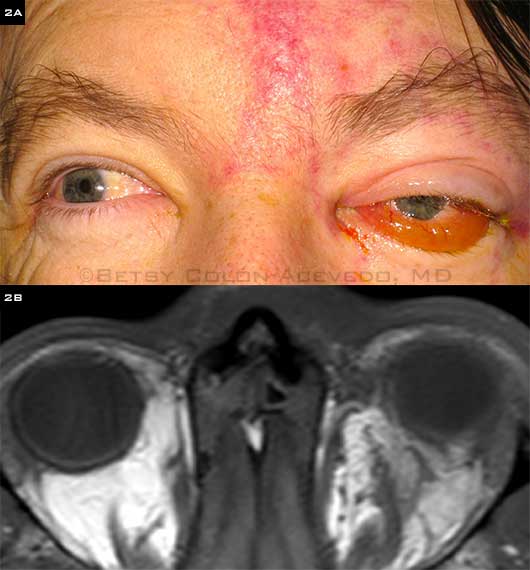
SOVT SECONDARY TO SEPSIS. (2A) A 50-year-old diabetic man was admitted with methicillin-resistant S. aureus bacteremia, endocarditis, and new-onset left scalp phlebitis with associated left eye pain. Visual acuity was 20/50 in the left eye; and ptosis, proptosis, chemosis, and incomplete ophthalmoplegia were present. (2B) MRI shows a T2 hypointense filling defect in the left superior ophthalmic vein, suggesting SOVT. Edema in the superior orbit extends into the left superior rectus muscle. After the patient was treated with IV vancomycin and IV heparin, VA improved to 20/25, and proptosis, ptosis, and ophthalmoplegia resolved fully.
|
Diagnosis and Workup
In the early stages, a mildly enlarged SOVT may be missed on CT scans, and decreased blood flow through the SOV and cavernous sinus may not be apparent. Magnetic resonance imaging (MRI) and magnetic resonance venography are more sensitive early in the disease process and are recommended if there is suspicion of SOVT or CST.1,4 MRI may demonstrate a dilated SOV and extraocular muscle enlargement. Doppler imaging with ultrasound can also be used to confirm the lack of flow in the SOV.6
Systemic associations. Patients with SOVT should be evaluated, in consultation with an internist, for underlying systemic illness. Laboratory investigation should include a complete blood count looking for leukocytosis or left shift, an increase in the ratio of immature to mature leukocytes.
Inflammatory and autoimmune workup may be indicated, including laboratory tests for serum angiotensin-converting enzyme, rheumatoid factor, antineutrophil cytoplasmic antibody, antimicrosomal antibody, and thyroid function.1,7 Chest x-ray may also be indicated to evaluate for sarcoidosis.
If there are no signs of infection or inflammation, evaluation for a hypercoagulable condition may be warranted, including factor V Leiden, prothrombin gene mutation, lupus anticoagulant, and antithrombin III.1
 |
|
SOVT IN PROTHROMBIN MUTATION. (3A, 3B) A 54-year-old woman with a history of prothrombin gene mutation presented after two days of worsening right eye pain and headache. She had visual acuity of 20/30 in both eyes, and ptosis and proptosis were apparent on her right side. (3C) Contrast-enhanced MRI shows a tubular hyperdensity in the right superior ophthalmic vein with no evidence of cavernous sinus thrombosis. She was treated with IV heparin and bridged to the oral anticoagulant rivaroxaban. She ultimately had full resolution of ptosis and proptosis.
|
Management
The appropriate management of SOVT depends on the etiology.
Antibiotics. Infection is one of the most common causes of SOVT and associated CST. For this reason, empiric treatment with broad-spectrum antibiotics is recommended while awaiting culture results. Vancomycin and ceftazidime are a typical initial regimen.8
Antibiotics should be extended for two weeks beyond clinical resolution of the infection, as pathogens may be sequestered within the thrombus.4 If there is no evidence of local infection, a remote nidus should be considered, such as bacterial endocarditis.5
Anticoagulation. The role of anticoagulation therapy in isolated SOVT is unclear. However, SOVT that is not treated with anticoagulation may progress to CST, and some evidence supports anticoagulation in the setting of CST.2 Thus, if there are no contra-indications to anticoagulation, such as risk factors for intracranial or retroperitoneal hemorrhage, then systemic anticoagulation should be initiated.4
Dose-adjusted intravenous (IV) heparin is the recommended treatment. One randomized controlled trial suggests an IV bolus injection of 3,000 IU followed by 25,000 to 65,000 IU/ day continuous IV infusion, adjusted according to prothrombin time (PTT) such that the PTT is doubled but does not exceed 120 seconds.9
Steroids. The role of corticosteroids in SOVT is, likewise, controversial.2,8 Although limiting the inflammation of thrombophlebitis within the tight confines of the orbit would be beneficial, the risk-to-benefit ratio of this intervention has not been determined.
If the etiology is infectious, steroids are typically withheld in the acute phase of the disease, and patients are managed with IV antibiotics and anticoagulation. If the etiology is noninfectious, high-dose steroids may be used in the acute phase, followed by a slow taper for several weeks.
It has been suggested that noninfectious SOVT may be a variant of idiopathic orbital inflammatory disease, which may be steroid responsive.
Surgery. Surgical intervention is indicated in the presence of an orbital abscess or sinus disease to drain the primary source of infection as soon as possible.2
If orbital crowding is causing visual loss, orbital decompression may be an option for some patients.
___________________________
1 Lim LH et al. Eye. 2014;28(3):348-351.
2 Desa V, Green R. J Oral Maxillofac Surg. 2012;70(9):2085-2091.
3 Grassi MA et al. Surv Ophthalmol. 2003;48(5):555-561.
4 Cumurcu T et al. Semin Ophthalmol. 2013;28(2):58-60.
5 Berenholz L et al. Arch Otolaryngol Head Neck Surg. 1998;124(1):95-97.
6 Flaharty PM et al. Arch Ophthalmol. 1991;109(4):582-583.
7 Park HS et al. J Craniofac Surg. 2014;25(4):e322-324.
8 Schmitt NJ et al. Ophthal Plast Reconstr Surg. 2005;21(5):387-389.
9 Einhaupl A et al. Lancet. 1991;338(8767):597-600.
___________________________
Dr. Kumar is an ophthalmology resident, Dr. Colón-Acevedo is a fellow in oculoplastic and reconstructive surgery, and Dr. Liss is an oculoplastic surgeon; all are at the Duke Eye Center in Durham, N.C. The authors report no related financial interests.