By Julia Sein, BS, Alexandra Stefanovic, MD, and Carol L. Karp, MD
Edited by Ingrid U. Scott, MD, MPH, and Sharon Fekrat, MD
This article is from September 2012 and may contain outdated material.
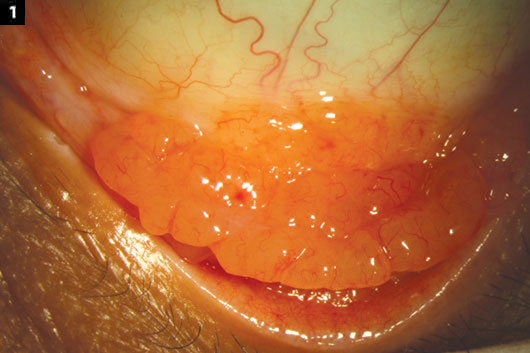
Conjunctival lymphoma is an ocular surface tumor that usually appears as a painless, salmon-pink, “fleshy” patch. Although it generally has a smooth surface, it can also appear as a multinodular lesion or as follicular conjunctivitis (Fig. 1).
 |
|
POTENTIAL PRESENTATION. The follicular form of conjunctival lymphoma. Patients often have minimal symptoms, leading to a delay in diagnosis.
|
Ocular adnexal lymphomas account for 2 percent of all non-Hodgkin lymphomas, and the conjunctiva is the primary area of involvement in 30 to 40 percent of cases. Conjunctival lymphoma constitutes about 1.5 percent of conjunctival tumors and is reportedly the most common acquired subepithelial lesion.1
These lesions are usually primary extranodal B-cell neoplasms, although 10 to 30 percent are secondary tumors in patients with disseminated lymphoma. Extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue (MALT-type lymphoma) is the most prevalent subtype, followed by follicular and diffuse large B-cell lymphoma.
The incidence of MALT ocular lymphomas is on the rise, with an annual increase of 6 percent. The masses are bilateral in about 20 to 38 percent of patients. Conjunctival lymphomas typically have an indolent course, and isolated involvement of the conjunctiva portends a better prognosis. However, 20 percent of patients with an initially localized conjunctival lymphoma will eventually develop disseminated disease. Systemic involvement is more common in bilateral (47 percent) than in unilateral lymphoid infiltrates (17 percent).2
Etiologic Factors
Infectious. One hypothesis postulates that MALT lymphoma arises from somatic mutations during the lymphocytic response to chronic antigenic stimulation from an infectious or inflammatory process, with subsequent genetic mutations, autonomic proliferation, and eventual monoclonal transformation to lymphoma. Microbial and viral agents such as Chlamydophila psittaci, Helicobacter pylori, Borrelia burgdorferi, and the hepatitis C virus have been linked to MALT lymphoma with predilection for different organs and tissues.3
A potential role of C. psittaci (Cp) in the pathogenesis of ocular adnexal MALT lymphoma has been suggested in various studies from different countries, but this association remains controversial due to differences in detection methodologies and apparent variability across different geographic regions worldwide.4
Autoimmune. Chronic inflammatory conditions associated with orbital lymphoma include thyroid orbitopathy, Hashimoto thyroiditis, Sjögren syndrome, and celiac disease.5
Clinical Presentation
Conjunctival lymphoma shows a female predominance and occurs most frequently in the fifth to seventh decade of life as a salmon-pink nodular patch in the bulbar conjunctiva. Patients often have minimal symptoms, leading to an average delay of eight months between clinical onset and diagnosis. Various clinical complaints include conjunctival redness, irritation, and excessive tear production. Patients may also present with a palpable mass, ptosis, or diplopia.
Diagnosis
Differential diagnosis. The following conditions must be ruled out: benign reactive lymphoid hyperplasia, benign ocular surface tumors (squamous papilloma, pyogenic granuloma, and lymphangiectasis), malignant tumors (squamous cell carcinoma and amelanotic melanoma), scleritis, episcleritis, ectopic lacrimal gland, presence of a foreign body, amyloid deposition, and chronic follicular conjunctivitis.
Biopsy. Whenever a diagnosis of lymphoma is suspected, it is imperative to send fresh tissue for flow cytometry and gene rearrangement studies in addition to formalin-fixed tissue analysis. Both eyes should be biopsied. In the clinically uninvolved eye, an inferior forniceal biopsy is performed. Clinical differentiation between benign lymphoid hyperplasia and malignant lymphoid lesions is impossible; therefore, histopathologic evaluation and immunohistochemical studies are necessary to establish the diagnosis.
Staging. Although conjunctival lymphoma typically presents with a localized lesion, a minority of patients have disseminated disease at presentation. Proper staging evaluation includes a complete history and physical examination, complete blood count, metabolic panel, serum lactate dehydrogenase levels, serum protein electrophoresis and beta2-microglobulin levels, computed tomography (of the neck, chest, abdomen, and pelvis), magnetic resonance imaging (of the orbit and brain), and bone marrow biopsy.
Treatment
Individual treatment is determined by whether the tumor is localized to the conjunctiva or disseminated to other parts of the body.
Localized disease. The mainstay of treatment for localized disease is external-beam radiotherapy (EBRT) with 30 to 36 gray (Gy), usually given in 20 daily fractions of 1.8 Gy. The complete remission rate is in excess of 90 percent for MALT lymphoma, with excellent long-term local control in the majority of patients. Potential complications of EBRT include xerophthalmia, keratitis, cataract formation, and retinopathy.6
Interferon alfa-2b is a glycoprotein produced by leukocytes and has both antiviral and antitumor activity. Several cases of complete remission in patients after eight weeks of intralesional injections of interferon alfa-2b have been described in localized conjunctival lymphoma.7 The drug’s role is limited to low-grade lymphomas. Side effects comprise flu-like symptoms during the first week after injection.
Intralesional injections of the CD20 antibody rituximab, combined with autologous serum, have led to complete remission in several cases of MALT lymphoma and follicular lymphoma.8 Longer follow-up is necessary to determine the role of this agent in disease regression.
If the conjunctival lesion is relatively small and circumscribed, an excisional biopsy and careful observation might suffice. However, this approach is associated with a high risk of recurrence due to subclinical invasion of tumor into surrounding tissues without adjuvant treatment.6
Systemic disease. There is no universally accepted gold standard of treatment for disseminated disease. A number of single agents (including chemotherapy and immunotherapy) as well as combination chemotherapy regimens are commonly used.
Rituximab has shown efficacy in the treatment of conjunctival MALT lymphoma, with response rates between 50 to 87 percent. However, median time to recurrence was less than one year.9
Doxycycline is considered of uncertain benefit in the treatment of patients with conjunctival MALT lymphoma. One prospective phase 2 trial observed partial or complete regression of conjunctival MALT lymphoma with doxycycline administration in seven out of 11 patients who were Cp-positive and in six of 16 who were Cp-negative.10 However, a more recent study reported no detection of bacterial DNA (from Cp, H. pylori, Escherichia coli, Staphylococcus aureus, or Yersinia pestis) in ocular adnexal MALT lymphomas, suggesting that the previously reported effect of antibiotic treatment could be due to geographic variations as well as differences in detection methodologies.11
A recent phase 2 trial using targeted radioimmunotherapy with Zevalin (yittrium-90 ibritumomab tiuxetan) presents a promising first-line therapy for patients with early stage extranodal B-cell lymphoma of the ocular adnexa. The complete remission rate was 83 percent for stage IE disease, with no significant side effects or high-grade cytopenias.12 No cases of distal (extraorbital) relapse were observed during a median follow-up time of 20 months.
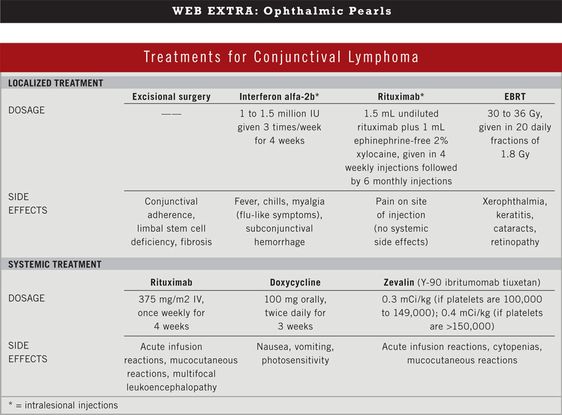
(click to expand)
Follow-up
Due to its indolent nature, the prognosis of primary localized conjunctival MALT lymphoma is generally favorable, with a reported five-year survival of 93 percent. Because nearly 20 percent of patients with ocular adnexal lymphoma eventually progress to disseminated disease, follow-up is essential and should be continued indefinitely. Follow-up is recommended every three months for the first year and every six months afterward.
Case Report
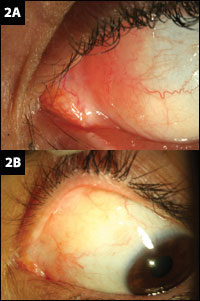 |
| BEFORE AND AFTER. (2A) Conjunctival lymphoma on presentation. (2B) One month after 30 Gy of EBRT. |
A 43-year-old woman with a three-week history of a painless pink growth on her left eye was referred to the Bascom Palmer Eye Institute for evaluation. Her UCVA was 20/20 in each eye. The slit-lamp examination of the left eye revealed a salmon-pink gelatinous lesion in the inferior fornix, the nasal bulbar conjunctiva (Fig. 2A), and the superior nasal aspect of the bulbar conjunctiva. Inferior forniceal follicles were evident in the right eye. The remainder of the examination was normal. There were no palpable preauricular, submandibular, or cervical lymph nodes.
Conjunctival biopsies were performed in both eyes. Histologic sections of both specimens showed a monotonous population of predominantly small, round lymphocytes with a small population of cytologically atypical lymphocytes. Kappa light chain restriction was found, pointing to a monoclonal B-cell population with CD20 positivity. The CD5, CD10, and CD23 markers were negative. These findings were confirmed with gene rearrangement analysis, which showed rearrangement of the immunoglobulin gene. The results were interpreted as extranodal marginal zone lymphoma (MALT lymphoma) in both eyes.
Our patient was referred to an oncologist for an extensive workup; the oncologist detected no other organ involvement or lymphadenopathy. She received external beam radiation therapy of 30 Gy to both orbits over four weeks; this was well tolerated with mild edema to the eyelids and no complaints of dryness.
One month later, the tumor had shrunken considerably (Fig. 2B), and there were no changes in vision. Six months later, there was no evidence of the tumor in either eye, and the conjunctival tissue architecture was normal. She has remained disease free for two years.
|
Summary
Conjunctival lymphoma is the second most common ocular adnexal tumor and generally manifests as a salmon-pink patch on the fornix of the eye. Marginal zone B-cell lymphoma (MALT-type lymphoma) is the most frequent subtype identified on biopsy and immunohistochemical studies. It is postulated that MALT lymphomas might be linked to chronic inflammatory or autoimmune disorders.
Although EBRT is the mainstay of treatment for localized lesions, other treatment modalities have shown efficacy in various case reports and series. Systemic treatment with chemotherapeutic agents is reserved for patients with disseminated or recurrent disease.
___________________________
Ms. Sein is a medical student, Dr. Stefanovic is assistant professor of clinical medicine, and Dr. Karp is professor of ophthalmology; all are at the University of Miami. The authors report no related financial interests.
___________________________
1 Bardenstein DS. Ophthalmol Clin North Am. 2005;18(1):187-197.
2 Shields CL et al. Ophthalmology. 2001;108(5):979-984.
3 Stefanovic A, Lossos IS. Blood. 2009;114(3):501-510.
4 Husain A et al. Cancer. 2007;110(4):809-815.
5 Nutting CM et al. Eye. 2006;20(6):645-648.
6 Tsai PS, Colby KA. Semin Ophthalmol. 2005;20(4):239-246.
7 Lachapelle KR et al. Arch Ophthalmol. 2000;118(2):284-285.
8 Ferreri AJ et al. Ophthalmology. 2011;118(1):24-28.
9 Coupland SE et al. Surv Ophthalmol. 2002;47(5):470-490.
10 Ferreri AJ et al. J Natl Cancer Inst. 2006;98(19):1375-1382.
11 Matthews JM et al. Br J Haematol. 2008;142(2):246-249.
12 Esmaeli B et al. Ann Oncol. 2009;20(4):709-714.