By Peggy Denny, Contributing Writer, interviewing John J. Chen, MD, PhD, Stacy L. Pineles, MD, and Prem S. Subramanian, MD, PhD
Download PDF
Adult-onset esotropia can arise from a variety of causes, from benign to life-threatening, and it is critical for ophthalmologists to recognize key distinguishing features. One common type of esotropia that occurs in older adults has garnered particular attention in recent years, as a new understanding has emerged about its mechanism. Known by a variety of names, including divergence insufficiency, age-related distance esotropia (ARDE), and sagging eye syndrome (SES), it is characterized by diplopia only on distance viewing.1 The good news is that this condition is not associated with neurologic or systemic disorders, and it can be managed successfully.
A Puzzling Entity
With this type of strabismus, “When someone is reading or looking at their phone, they’re fine, but when they’re driving or watching a movie, they see double,” said Stacy L. Pineles, MD, at the Stein Eye Institute in Los Angeles. “It’s what we used to call divergence insufficiency, reflecting the fact that when you go from looking at near to looking far away, the eyes need to diverge.”
“The term divergence insufficiency implies a problem at the level of the brainstem, suggesting that there is decreased neural output to the extraocular muscles,” said Prem S. Subramanian, MD, PhD, at the University of Colorado in Aurora. “Because of that, we used to teach that you should be very suspicious that such a patient might have a brainstem problem and that they should be sent to a neurologist and always have neuro-imaging.”
However, noted John J. Chen, MD, PhD, at the Mayo Clinic in Rochester, Minnesota, many of these patients showed no signs of stroke, tumor, or other dangerous etiologies on examination or magnetic resonance imaging (MRI).
“We had seen a benign form of divergence insufficiency in the clinic for decades, and there was a lot of hand-waving in terms of possible causes,” said Dr. Chen. And because the condition usually occurred in patients over the age of 60, “we speculated that their divergence centers in the brainstem were just degenerating with age.”
 |
|
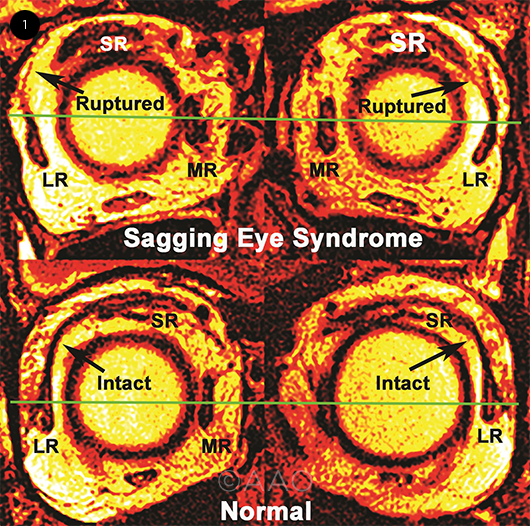
SAGGING EYE SYNDROME. The top two coronal MRI scans show inferior displacement of the lateral rectus (LR) muscle in both eyes due to rupture of the LR–superior rectus (SR) band bilaterally. The bottom row shows the normal anatomy. The horizontal line indicates the center of the medial rectus muscle.
|
Uncovering a New Mechanism
Instead of studying the brainstem for the origin of this condition, Joseph L. Demer, MD, and his colleagues looked into the orbit for clues. Using a specialized type of orbital MRI, they found characteristic changes in the position of the superior and lateral rectus muscles and the connective tissue that holds them in place.2
As Dr. Chen explained, “There’s a deterioration of a band of tissue between the superior rectus and the lateral rectus in these patients, and the lateral rectus sags down. When you’re young, that muscle is horizontal, and there’s a nice pulley system that can straighten out the eyes. But when the muscle sags, it can’t efficiently make the eyes diverge.”
Dr. Pineles added, “Just like other parts of the body, [this muscle] starts to sag. Thus, it’s a mechanical, not a neurological condition.” To describe this mechanism, Dr. Demer coined the term sagging eye syndrome. Dr. Chen said that he still generally calls the condition divergence insufficiency as an “umbrella term,” but he includes in his notes that it’s caused by SES. “I think patients like the term divergence insufficiency more than the word ‘sagging.’”
Not just horizontal strabismus. In many patients with SES, a small amount of hypotropia is present as well. “A symmetric or mildly asymmetric deficit of elevation in both eyes is part of the whole senescent process in the orbit,” said Dr. Subramanian. “It goes along with these patients often having a deep superior sulcus and even a bit of eyelid ptosis.”
Growing acceptance of the theory. When this mechanism was proposed in 2009, it was controversial. Dr. Subramanian said, “People didn’t really believe that the changes seen on MRI and even histology sections were truly responsible for eye movement abnormalities. But with further studies being published, and other researchers corroborating the findings, it has become much more accepted.” Indeed, it has been incorporated into the Academy’s Preferred Practice Pattern on adult strabismus.1
Epidemiology of SES
How common is it? Drs. Chen, Pineles, and Subramanian all reported frequently seeing SES patients in their practices. Dr. Subramanian said that he hasn’t seen an overall increase in patients with age-related distance esotropia. However, because of Dr. Demer’s work, he is approaching them differently and “sorting out more patients with the sagging eye mechanism from those with neurological conditions.”
In contrast, Dr. Pineles said that she is seeing more patients with possible SES in her practice. She attributed this to “the great evolution in cataract and refractive procedures [that] is making people expect nearly perfect vision without glasses.” She added, “It used to be that many older people would still need glasses and so would wear prisms. Now they don’t want to wear prisms and are finding their way to strabismus specialists.”
Data from a case series. A retrospective case series took a closer look at the frequency of SES. The authors studied the records of all new patients over the age of 40 who presented to the Stein Eye Institute with binocular diplopia between January 2015 and December 2018. Among the 945 patients, the leading cause of diplopia was SES, which was diagnosed in 31.4%.3
In other important findings from this study, the SES patients were older than the other diplopia patients (mean age, 71.2 years vs. 66.5, respectively), and the percentage of SES patients increased with age, from about 4.7% under the age of 50, to 60.9% over the age of 90. In addition, the SES patients were more predominantly female than the other patients (59.9% vs. 52.0%, respectively).3
Differential Diagnosis for SES
The most important part of diagnosing SES is ruling out any serious underlying conditions that may be associated with adult-onset esotropia or acquired diplopia. Drs. Chen, Pineles, and Subramanian listed the following as conditions of particular concern:
- cranial nerve palsy (third, fourth, or sixth nerves)
- thyroid eye disease
- myasthenia gravis
- any cause of increased intracranial pressure (e.g., brain tumor or pseudotumor cerebri)
In addition, adult-onset esotropia and diplopia can be caused by decompensation of a long-standing phoria, said Dr. Subramanian.
Key Points for Diagnosis
Type of diplopia. The first step, said Dr. Chen, is to make sure that the diplopia is binocular. “I’ve seen tons of patients referred to our clinic for double vision, and it’s actually monocular double vision caused by cataract or dry eye.” After that, “We do alternate cross-cover testing to look at the pattern of the double vision, and that can clue you in to other diagnoses,” such as a cranial nerve palsy.
Pattern of strabismus. Dr. Pineles said, “I look for the pattern where the esotropia is present at distance but not at near, and it’s comitant—the same in left and right gaze, and up and down. If it’s the same everywhere, then you can often make an SES diagnosis without further workup.”
Dr. Subramanian agreed, saying, “If it’s highly incomitant, I’m going to be more suspicious that it’s not ARDE or SES.” He added that a vertical component, if present, is small. “More than 4 or 5 prism diopters [PD] of vertical deviation will prompt me to think of other causes of adult-onset strabismus, such as thyroid eye disease, myasthenia gravis, or a brainstem disorder.”
Ductions. “It’s very important to check the ocular ductions to see if they are full or not. In ARDE/SES, patients should not have any significant deficit in horizontal movements, although they may have some limitation or a small symmetric deficit of elevation of both eyes,” Dr. Subramanian said.
Rate of progression. “SES is a very slow process,” said Dr. Chen. “Anything that progresses rapidly should raise suspicion of an alternative etiology.”
External clues. ARDE/SES patients “usually have normal eye position, or they may even have a mild relative enopthalmos because of atrophy of the orbital tissues,” said Dr. Subramanian. “Proptosis suggests other conditions, such as thyroid eye disease.”
Dr. Chen noted that some of the involutional changes of SES have counterparts on the face: “Patients usually have eyelid and brow ptosis and a deep superior sulcus.”
What about imaging? “I don’t routinely do orbital MRI. I will get it if I’m questioning the diagnosis, if I’m not sure,” said Dr. Subramanian. Dr. Pineles concurred, adding that in doubtful cases she obtains both orbit and brain MRI.
Management
SES can be managed with either prisms or surgery, depending on patient preference and the amount of deviation. Dr. Pineles said, “I tell patients that both are reasonable options, discuss the risks and benefits, and let them decide.”
Prisms. Dr. Subramanian said that the majority of his patients choose prism correction first. “They’re often wearing glasses anyway, so they try to see if it works.” He starts—as do Drs. Chen and Pineles—with a trial of press-on prisms before prescribing ground-in prisms.
“Because of the cost of new glasses,” Dr. Chen said, “we have them try the press-on prism for a month to make sure they like it and there’s no change in alignment. Then we usually recommend ground-in prism.”
Surgery. However, for patients with larger deviations—16 PD or more—surgery may be the better option, said Dr. Pineles. Some patients choose surgery after a trial of prism, while others prefer to go directly to surgical correction because they want to avoid wearing glasses for cosmetic or other reasons. Dr. Subramanian said, “In Colorado, where I practice, people on average remain more active, even as they get into their 60s and 70s, and they don’t want to wear glasses.”
Regarding the type of procedure, the surgeon can choose to weaken the medial rectus muscle (bilateral medial rectus recession) or strengthen the lateral rectus muscle (bilateral lateral rectus resection), Dr. Pineles said.
When It Isn’t SES: Critical Clues
Classic cases of ARDE/SES that conform to the points discussed in this article can generally be diagnosed clinically, without need for extensive workup or imaging, said Dr. Subramanian.
However, Dr. Pineles pointed out, “It’s important to be alert for signs or symptoms that are atypical for SES.”
Important red flags that require further workup and MRI include the following:
- incomitant strabismus
- limitation of ductions
- vertical strabismus greater than 4 or 5 PD
- proptosis
- rapid progression
- signs of neurologic deficits
- age younger than that typical for ARDE/SES (≥60 years of age)
|
Additional Surgical Pearls
Timing. “Don’t jump right into surgery,” said Dr. Chen. “We usually like to see some stability for about three to six months, because part of confirming the diagnosis of this type of divergence insufficiency is that it should be relatively stable over time.”
MRI can be helpful. Even if the diagnosis of SES is made clinically, MRI can be useful in surgical planning, said Dr. Subramanian. “If the MRI proves that the patient has this type of mechanical change or stretching, it can change your surgical approach.”
Adjust your surgical dose. The usual formulas of millimeters of correction per PD do not apply to SES, said Dr. Subramanian. “We’re finding that we have to do more surgery than we would expect for the measured deviation. Standard tables assume that the patient has normal lateral rectus function, but with SES, you’re not dealing with normal lateral rectus anatomy or physiology.”
Dr. Subramanian added, “We all have to make some degree of adjustment. Some surgeons say they target twice the primary deviation, while others say 1.5 times. It really is individual, and there’s a bit of a learning curve.”
Further Reading
Chaudhur Z, Demer JL. Long-term surgical outcomes in the sagging eye syndrome. Strabismus. 2018;26(1):6-10.
Kawai M et al. Characterization of the position of the extraocular muscles and orbit in acquired esotropia both at distance and near using orbital magnetic resonance imaging. PLoS One. 2021;16(3):e0248497.
Kono R et al. Magnetic resonance imaging findings of age-related distance esotropia in Japanese patients with high myopia. Graefs Arch Clin Exp Ophthalmol. 2019;237(3):657-662.
Ugradar S. et al. The adnexal phenotype of sagging eye syndrome. Ophthalmic Plast Reconstr Surg. 2020;36(5):475-477.
|
When to Refer
In most cases, patients will first see their primary ophthalmologist about new-onset double vision. Should they be referred to a neuro-ophthalmology or strabismus specialist?
“Many of these patients have already been receiving care from a comprehensive ophthalmologist for cataracts, glaucoma, or other age-related eye problems,” said Dr. Subramanian. “It makes sense to me that their regular ophthalmologist could sort out those patients who need to be referred and those who could be kept in the comprehensive practice.”
Dr. Pineles agreed, saying, “If the patient’s esotropia is small and comitant—that’s the key—and not present at near, and there are no other neurological symptoms or signs, the primary ophthalmologist can give them prisms. But if there’s anything atypical, or if they want to consider surgery, I would refer out to a specialist.”
The most important point for all ophthalmologists, said Dr. Chen, is learning to recognize the red flags to determine the next steps. And after all danger signals are ruled out, clinicians can feel comfortable knowing that the condition is benign and does not require further workup.
___________________________
1 American Academy of Ophthalmology. Adult Strabismus Preferred Practice Pattern. 2019. aao.org/preferred-practice-pattern/adult-strabismus-ppp.
2 Rutar T, Demer JL. J AAPOS. 2009;13(1):36-44.
3 Goseki T et al. Am J Ophthalmol. 2020;209:55-61.
___________________________
Dr. Chen is professor of ophthalmology and neurology at the Mayo Clinic in Rochester, Minn. Relevant financial disclosures: None.
Dr. Pineles is associate professor of ophthalmology and director of the Residency Program at the Stein Eye Institute at the University of California, Los Angeles. Relevant financial disclosures: None.
Dr. Subramanian is professor of ophthalmology, neurology, and neurosurgery, Vice Chair for Academic Affairs, and chief of neuro-ophthalmology at the University of Colorado, Anschutz Medical Campus, in Aurora. Relevant financial disclosures: None.
For full disclosures and the disclosure key, see below.
Full Financial Disclosures
Dr. Chen Roche: C; UCB: C.
Dr. Pineles None.
Dr. Subramanian GenSight Biologics: C,S; Horizon Pharmaceuticals: C,S; Invex Therapeutics: C; Santhera Pharmaceuticals: S; Viridian Therapeutics: C.
Disclosure Category
|
Code
|
Description
|
| Consultant/Advisor |
C |
Consultant fee, paid advisory boards, or fees for attending a meeting. |
| Employee |
E |
Employed by a commercial company. |
| Speakers bureau |
L |
Lecture fees or honoraria, travel fees or reimbursements when speaking at the invitation of a commercial company. |
| Equity owner |
O |
Equity ownership/stock options in publicly or privately traded firms, excluding mutual funds. |
| Patents/Royalty |
P |
Patents and/or royalties for intellectual property. |
| Grant support |
S |
Grant support or other financial support to the investigator from all sources, including research support from government agencies (e.g., NIH), foundations, device manufacturers, and/or pharmaceutical companies. |
|