Download PDF
Measuring intraocular pressure (IOP) is a routine part of an adult eye exam. “You would never not measure an adult’s IOP,” said pediatric ophthalmologist Sharon F. Freedman, MD, at Duke University Medical Center. Yet when it comes to children, ophthalmologists often don’t check.
One reason is a prevailing assumption that kids don’t get glaucoma. Kids do get glaucoma. You need to know when to check their pressure.
Another reason is that measuring pressure isn’t easy. Children squirm. They balk. They cry. At best, measuring IOP becomes a game with children. At worst, it means a trip to the operating room for sedation or anesthesia.
Three experts offer insight and advice on the special challenges of measuring IOP in children.
Which Kids to Measure
All 3 of the experts say that you have to measure IOP, at least in children with risk factors—and these are different from the risk factors in adults. The stakes are higher in children, too.
“Damage can happen on a very accelerated timeline compared with adults,” said Dr. Freedman. “The eye of a very young child is susceptible to rather rapid stretching and resultant damage to multiple ocular structures under high IOP, while the adult eye suffers damage primarily to the optic nerve.”
For a number of reasons, tonometry might be your most valuable diagnostic tool in monitoring pediatric glaucoma: Children often cannot do a reliable visual field test, and optic nerve imaging with photography or OCT may be precluded by problems with cooperation, nystagmus, and corneal scarring or other media opacities. “We rely more heavily on pressure measurements in identifying and managing glaucoma in children than in adults,” Dr. Freedman said.
Checking pressure in these kids is a must. Jane C. Edmond, MD, a pediatric ophthalmologist and pediatric neuro-ophthalmologist at Texas Children’s Hospital, told a cautionary tale about a 6-year-old who was on steroid eyedrops for juvenile rheumatoid arthritis (JRA). Because of the patient’s age, the doctor didn’t consider glaucoma and didn’t check IOP. But then, at an annual dilated eye exam, the doctor saw that the child’s optic nerve was cupped. Moral of the story, said Dr. Edmond: “A patient on chronic steroid drops for iritis from JRA is at risk for glaucoma.”
JRA is just one red flag. Be sure to check IOP in the following cases, too:
- Patient on chronic steroid drops for iritis of any cause
- Family history of glaucoma with onset at young age
- Previous cataract surgery
- Port-wine stain associated with Sturge-Weber syndrome
- Eyelid plexiform neurofibroma
- Down syndrome
- Hurler syndrome
- Aniridia
- Axenfeld-Rieger syndrome
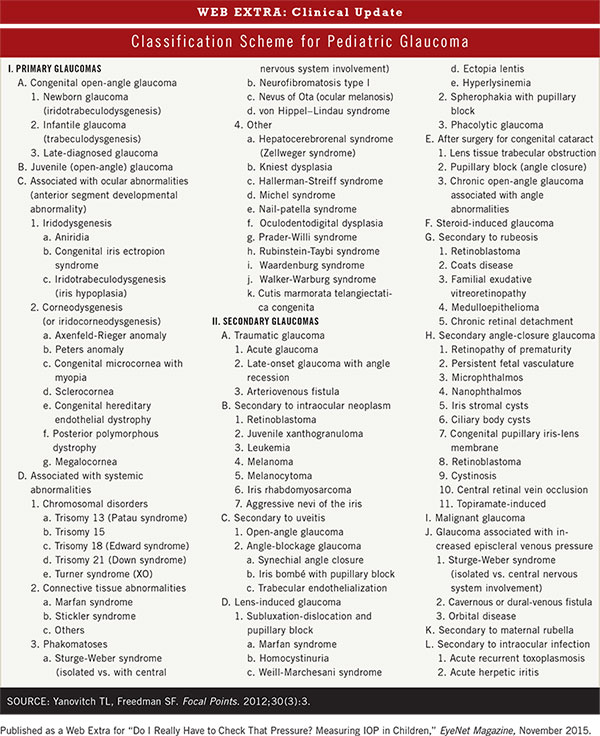
- Post-trauma (See the Web Extra below for a more comprehensive list.)
(click to expand)
Which Device to Use?
All of the measurement devices have their pros and cons.
Goldmann applanation tonometry. GAT remains the gold standard for measuring IOP. But even the most cooperative child is likely to resist the accompanying stinging fluorescein dye and numbing drops, the experts agree.
Icare (Icare Finland). Dr. Freedman favors the Icare for measuring IOP in infants and small children who cannot cooperate for GAT. The Icare, a rebound tonometer, gives a digital reading and can be used without topical anesthetic drops. Its probe tip is small enough to fit into a narrow palpebral fissure, and the probe speed is fast enough to take measurements between natural blinks of a child’s eye.
If Dr. Edmond can’t get a Goldmann applanation pressure, she’ll use the Icare. However, she will do so only if checking for a baseline pressure and if she’s not really worried about glaucoma. “I’ve been a bit disappointed with Icare,” she said. “Studies say it’s equivalent to GAT. We get high readings in my clinic.”
Pediatric ophthalmologist Allen D. Beck, MD, at Emory Eye Center, said Icare reads 2 to 3 points higher than applanation tonometry. He added that most doctors who work with children have an Icare because it “has allowed us to get pressures in children who were previously sent to anesthesia.”
Perkins (Haag-Streit). If Dr. Beck gets a high Icare reading, he may confirm with another tonometer. If the Icare reading is 21 to 22 mm Hg in a child with a healthy optic nerve, he won’t recheck pressure. But with a pressure of 22 to 30 mm Hg, he’s likely to recheck with the Perkins, a handheld applanation tonometer.
Dr. Edmond also uses the Perkins. “It still involves some level of cooperation,” she said, but it’s handheld, and it may be used when the patient is supine and in the operating room in patients under anesthesia. However, she added, not many clinics have one.
Tono-Pen (Reichert Technologies) is another handheld alternative, but like Goldmann, it requires anesthetic drops, Dr. Edmond said.
Cataract Surgery in Kids: Glaucoma Risk Rises
Children who have had surgery for congenital cataracts are at greater risk of glaucoma. “We know that,” said Dr. Beck, citing 5-year results from the Aphakia Treatment Study.1 The multicenter randomized clinical trial involved 114 infants with unilateral congenital cataract. It found a 17% risk of glaucoma by the 5-year follow-up after unilateral cataract removal at 1 to 6 months of age. The risk of glaucoma suspect status was 31%.
There are many possible explanations, Dr. Beck said. The eye may have other abnormalities apart from the cataract, or the surgery, even if done well, could increase the risk. Possibly, the effect of not having a crystalline lens might lead to long-term angle changes. Corticosteroid treatment following the cataract surgery also may play a role in the development of elevated IOP and glaucoma. (For more information, see “Aphakic and Pseudophakic Glaucoma After Congenital Cataract Surgery.”)
Dr. Edmond recalled a case of her own involving an aphakic 1-year-old with a history of congenital cataracts and unilateral episodic tearing. She ascribed the tearing to nasolacrimal duct obstruction. But when the child returned to clinic with tearing, hyperemic conjunctiva, and hazy cornea with elevated IOP, she realized the episodic tearing was due to painful, intermittent pressure spikes from glaucoma. “I had been in the mindset of nasolacrimal duct obstruction as the cause of tearing, given the child’s young age,” she said. “But if a child has had cataract surgery, think glaucoma,” she warned. “Don’t miss those at-risk kids.”
___________________________
1 Freedman SF et al. JAMA Ophthalmol. 2015;133(8):907-914.
|
Assessing Pressure Readings
With children, central corneal thickness (CCT) should be considered a little differently than it is in adults, said Dr. Freedman.
One of the surprise findings of the Ocular Hypertension Treatment Study (OHTS)—a study conducted with adult participants—was that central corneal thickness (CCT) is a powerful predictive factor for glaucoma. Thin corneas are at higher risk of developing primary open-angle glaucoma (POAG); thicker corneas predict a lower risk.
With children, Dr. Freedman said, “Under no circumstances should you adjust the recorded pressure based upon the corneal thickness.” She explained that in children, there’s a huge range of CCT, depending on the condition of the eye. In many youngsters, for example, the cornea becomes abnormal due to disease process. “In those [eyes], all bets are off in terms of knowing how CCT affects measured IOP,” she said.
“However, that said, it’s reasonable to consider whether you should change your target pressure based on your corneal assessment, especially in a glaucoma suspect with a thinner-than-normal CCT,” Dr. Freedman added. “Consider the CCT, but do not use a nomogram to change the recorded pressure.”
Tricks of the Trade
Summing up what he thinks is the most important message for ophthalmologists who are measuring pressure in children, Dr. Beck said, “Have patience.” He added, “Get the child calm by whatever means necessary. Make a little game of it, if you can. Most kids will respond to that very well.”
Dr. Edmond agreed. “We have lots of tricks.” Most are age specific.
Infants. “Babies are easy,” Dr. Edmond said. “Put in the anesthetic drop. Then give the baby a bottle. They’re zoning out. Then use the Tono-Pen.”
The terrible twos. Starting before age 2—and lasting for about 2 years—the child is savvy about the exam and resists, making it difficult to get an accurate reading. The child frequently will not cooperate with a Tono-Pen, which requires anesthetic drops and contact with the eye, Dr. Edmond said. Instead, Dr. Edmond will try Icare, while distracting the child with toys that light up and spin and make noise. If that fails, she said, you’ll need to use sedation or anesthesia to get a pressure reading.
Three years old and up. To get a child to sit at the slit lamp for applanation, Dr. Edmond says, “You’re going to ride our motorcycle. Grab the handlebars.” Then she has the child fixate on something behind her, such as a movie clip that plays on the visual acuity computer screen. She also uses distracting toys, such as a pedal-activated barking dog that has a light-up nose. After asking the child to look down, she gently opens the eyelid, keeping it propped open when the child looks straight ahead. Then she advances the applanation tip from the side and takes the pressure.
Another good trick is to use a favorite video on the parent’s smartphone, Dr. Beck said.
More at the Meeting
Dr. Freedman and Dr. Beck join senior instructor Alana L. Grajewski, MD, for Surgical Management of Pediatric Glaucoma (612). Using clinical cases and videos, this interactive instruction course will address the particulars of and provide pearls for performing surgery for childhood glaucoma. When: Tuesday, Nov. 17, 9:00-11:15 a.m. Where: Murano 3303. Access: Academy Plus course pass.
|
Off to the OR
When in-office testing is unsuccessful, pressure readings under anesthesia must be done in a hospital, with a pediatric anesthesiologist, Dr. Beck said.
Sevoflurane, the most common inhalation anesthetic, tends to cause IOP to fall. The effect is especially pronounced in children younger than age 2 but can occur in older children to a lesser degree. This can make it hard to figure out the true pressure, Dr. Beck said. He advised checking the pressure soon after the sevoflurane is administered and again later in the procedure. “Asleep, the child is cooperative, but you have to be concerned the pressure will drop off,” he said.
Ketamine, another option, doesn’t cause a drop in pressure. But it is administered by a painful intramuscular injection, and the child may wake up “out of sorts,” Dr. Beck said.
In either case, some parents don’t want their child to have anesthesia, and the jury is still out as to its possible neurotoxicity. “If parents are savvy and have been on the Internet and Facebook, they can give you pushback. They’re concerned about multiple anesthetics leading to learning disabilities,” Dr. Edmond said.
She tells parents that the literature on neurotoxicity and anesthesia in children is new and scant, and she assures them that she’ll make all efforts to limit repeated anesthetic events. Finally, she stresses her concern that an evaluation is necessary, or the child could suffer loss of vision or visual field.
Dr. Beck agreed. “We’ll take the risk of anesthesia when our suspicion for glaucoma is high and it has not been previously diagnosed, or when the glaucoma is being treated and we can’t get useful information and we’re concerned they’re getting worse.”
Bottom line. Tonometry is an important part of an exam, especially for at-risk children, Dr. Freedman said. “When a child comes into the office, if you’re not going to check the pressure, ask yourself, ‘Why do I not need to check the pressure?’ You should at least entertain the thought.”
___________________________
Dr. Beck is the William and Clara Redmond Professor of Ophthalmology, and director, section of glaucoma, at Emory Eye Center in Atlanta. Relevant financial disclosures: None. Dr. Edmond is a pediatric ophthalmologist and pediatric neuro-ophthalmologist at Texas Children’s Hospital, and associate professor of ophthalmology and pediatrics at Baylor College of Medicine in Houston. Relevant financial disclosures: None. Dr. Freedman is professor of ophthalmology and pediatrics at Duke University Medical Center, and chief of pediatric ophthalmology at Duke Eye Center in Durham, N.C. Relevant financial disclosures: None.
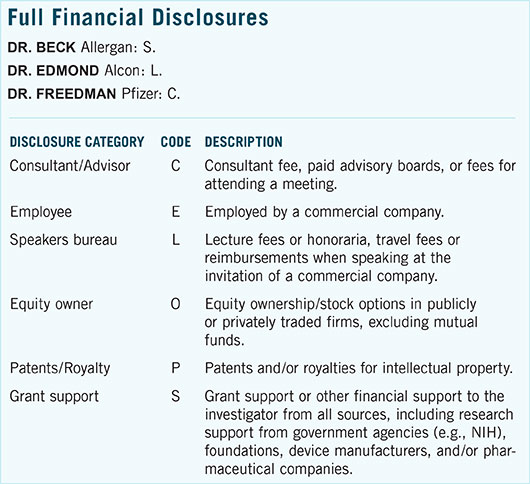
For full disclosures and the disclosure key, see below.