By Lt. Sarah Wied, DO, and CMDR. Cary Harrison, MD
Edited by Thomas A. Oetting, MD
This article is from October 2011 and may contain outdated material.
John Hardie,* a 28-year-old active duty naval petty officer, visited his primary care physician complaining of irritation in his left eye that increased with eye movement. This had persisted for a day and a half, along with tearing and a foreign body sensation, also in the left eye. Mr. Hardie had just returned from hiking and camping in Shenandoah National Park and thought that a bug might have gotten in his eye.
During this initial examination, Mr. Hardie’s primary care physician found that his uncorrected visual acuity was 20/15 in the right eye and 20/40 in the left. He had a focal area of hyperemia on his left bulbar conjunctiva without purulent, watery or bloody discharge. The physician attempted to dislodge the foreign body but was unsuccessful, so he urgently referred Mr. Hardie to our ophthalmology department with what was reported to be a metallic corneal foreign body.
We Get a Look
Mr. Hardie’s ocular history was notable for childhood strabismus, which had since resolved. The rest of his medical history was unremarkable, and he was not taking any medications.
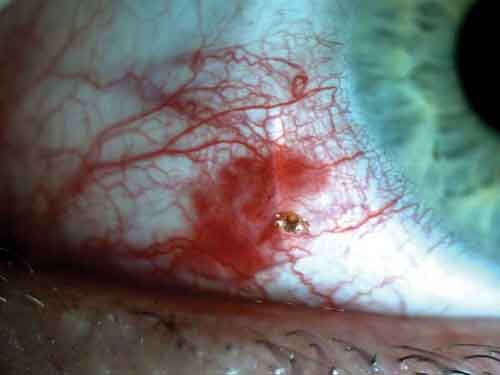
When Mr. Hardie arrived at our clinic, his VA was 20/20 in the right eye and 20/25-1 in the left, and there was no relative afferent pupillary defect. There was an injected section of bulbar conjunctiva inferonasal to the cornea, as well as a small conjunctival laceration and a subconjunctival hemorrhage surrounding a foreign body (Fig. 1). Under slit-lamp, high-power magnification, the foreign body was discovered to be a live tick with a translucent body. Its head was embedded in the conjunctiva, and motile appendages were seen in the tear film (Fig. 2).
 |
|
Foreign Body. The object was embedded in the conjunctiva (Fig. 1).
|
Treatment Strategy
We did a literature search but found no specific recommendations for how to remove ticks. In all but one of the cases, however, part of the surrounding conjunctiva was removed along with the arthropod.1–5 After extensive visual inspection, we determined that this particular tick was not deeply embedded; therefore, it would be appropriate to remove only the arthropod and thus avoid further injury and irritation to the surrounding tissues.
We began by anesthetizing the surrounding conjunctiva with 4 percent viscous lidocaine on cotton-tipped applicators. We then firmly grasped the body of the arthropod with a jeweler’s forceps and pulled straight out so that its head was in line with its body. Steady pressure was applied in a backward direction until the tick was pulled out of the conjunctiva with a little pop, like a cork coming out of a bottle. The specimen was immediately placed in formalin and sent to Naval Entomology for examination to ensure that all body, head and mouthparts were intact; for identification of the species; and for further studies to determine whether the tick carried any diseases that could be passed to humans. Mr. Hardie tolerated the procedure well.
As more than 36 hours had passed since attachment of the tick, Mr. Hardie was not immediately started on antibiotic prophylaxis for tick-borne diseases (as per the Infectious Disease Society of America guidelines6), be cause the arthropod was thought to be a larval tick. Larval ticks have a lower risk of infectious disease transmission, as young ticks often have not had a chance to feed on previous hosts and acquire pathogens. In addition, our patient was not displaying signs or symptoms of any of the infectious diseases associated with tick bites.
 |
|
Don’t Move. Motile appendages were seen in the tear film (Fig. 2).
|
Reassuring Results
The tick was found to be intact, with its head and all mouthparts attached to its body. The naval entomologists in Norfolk, Va., identified it as a hard tick in its larval stage, specifically a lone star tick (Amblyomma americanum) larva.7
The specimen was then sent to the Tick-Borne Disease Laboratory at the U.S. Army Public Health Command, where it was serologically tested by PCR and found to be negative for the following tick-borne diseases:Ehrlichia ewingii infection, human monocytic ehrlichiosis and Borrelia spp. infection (Lyme disease from B. burgdorferi and southern tick-associated rash illness8 from B. lonestari).
It was important to test for these diseases, as the tick was embedded in Mr. Hardie’s eye for more than a day and a half, which makes transmission of vector-borne diseases, if present, more likely. Moreover, researchers have found that lone star tick larvae are increasingly likely to be carriers of vector-borne diseases in the Eastern Seaboard states.9
Upon follow-up, Mr. Hardie’s conjunctival hyperemia and visual acuity had improved, and he had experienced no additional sequelae or symptoms of a systemic illness. He was released to further follow-up as needed with the ophthalmology department.
___________________________
1 Willen, C. et al. J Emerg Med 2011;40(3):e41–44.
2 Jensen, L. A. et al. J Parasitol 1982;68(4):528.
3 Meades, K. et al. Aust N Z J Ophthalmol 1991;19(4):365–366.
4 Bodé, D. et al. Ann Ophthalmol 1987;19(2):63–64.
5 Love, M. et al. Arch Ophthalmol 2001;119(12):1854–1855.
6 Go to www.idsociety.org and follow links to the Lyme Disease Final Report.
7 The Virginia Department of Health has a chart that can aid in speciation of ticks; see ;www.vdh.virginia.gov/tickbrochure.
8 www.cdc.gov/ncidod/dvbid/stari/index.htm.
9 Stromdahl, E. Y. et al. Vector-Borne Zoonotic Dis 2008;8(1):15–24.
___________________________
* Patient name is fictitious.
___________________________
Lt. Wied and Cmdr. Harrison are both U.S. Navy physicians stationed at the Naval Medical Center in Portsmouth, Va.
___________________________
NOTE: The views expressed in this article are those of the author(s) and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense or the U.S. Government.