By Steve L. Gerber, MD, and Cristina Lynn, OSC
Edited By: Steven J. Gedde, MD
Download PDF
Laura Mitchell,* an 11-year-old girl, had been experiencing worsening headaches over the past several weeks. Two months before coming to our office, she had seen an optometrist, who told her family that Laura’s optic nerves looked normal and referred her to a neurologist.
It took a few weeks for her to get in to see the neurologist and undergo magnetic resonance imaging (MRI). The family was told that the MRI appeared normal, and Laura was sent to us for further evaluation.
 |
|
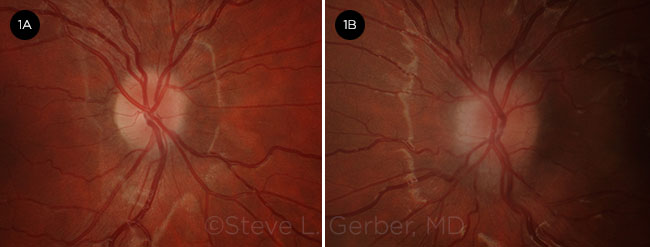
BEFORE TREATMENT. Patient’s right (1A) and left (1B) fundus. Note the optic nerve edema and indistinct margins, especially at the nasal side of the left eye.
|
We Get a Look
The patient’s story. Laura told us that the headaches were occurring more frequently. At first, they occurred only once every few days, but recently they had been striking daily and lasting for a few hours.
She described the pain as radiating from the back of her head to her right eye. The headaches were so severe that she had to lie down for relief, and they had caused her to miss a few days of school. She said that she heard a “screaming” sound in her ears several times per week, and it sometimes lasted for hours. She did not complain of blurry vision or other ocular symptoms.
She was not taking any medications and had no history of trauma. There was a family history of retinitis pigmentosa in her 2 brothers. Laura was notably overweight, and her body mass index was approximately 30, although there was no specific recent weight gain.
Exam findings. On examination, Laura’s visual acuity was 20/20 at distance and near without correction. She had normal results on color plates and stereo acuity testing, as well as on the slit-lamp exam.
However, a dilated exam showed abnormalities of both optic nerves (Fig. 1). The optic nerve borders were elevated, and no central cup was visible. The vessels, especially at the nasal border in the left eye, were obscured. The retina and vitreous exam was otherwise normal.
Visual field testing was normal in Laura’s right eye, and the left eye had a slightly enlarged blind spot.
Diagnosis
In a young patient with bilateral optic nerve edema and headache with a normal MRI, the next step would be lumbar puncture to evaluate the cerebrospinal fluid (CSF) opening pressure and content.
Based on Laura’s weight, idiopathic intracranial hypertension (IIH) was the most likely diagnosis. (This condition is also known as pseudotumor cerebri or benign intracranial hypertension.) However, IIH is a diagnosis of exclusion, and it is important to carefully evaluate the CSF to rule out other possible causes such as inflammation, infection, or tumor. For “Conditions to Consider in a Patient With Suspected IIH” see below.
The opening pressure was found to be elevated at 34 mm Hg, and the CSF was normal. Thus, we established IIH as the definitive diagnosis.
Treatment and Disease Course
The neurologist started Laura on oral acetazolamide (Diamox) at 500 mg twice daily. She did not tolerate this dosage well at first because of stomach upset. Subsequently, a lower starting dose was prescribed and was gradually increased; on this regimen, she obtained relief from her headaches and had less severe gastrointestinal upset.
It was repeatedly emphasized to her parents that weight loss would improve Laura’s condition significantly and might possibly allow her to stop taking medication. It was not until 6 months later that the family finally saw a dietitian and made a concerted effort to help her lose weight.
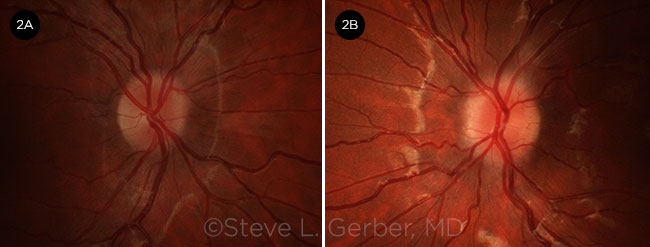
At her most recent exam, 9 months after diagnosis, Laura had lost 10 pounds. She was still taking Diamox, and her optic nerve edema had improved significantly (Fig. 2).
 |
|
AFTER TREATMENT. Patient’s right (2A) and left (2B) fundus. Nine months after diagnosis and subsequent treatment with acetazolamide and weight loss, the optic nerve edema had improved, and the margins were more distinct.
|
Discussion
Idiopathic intracranial hypertension refers to elevated intracranial pressure without an obvious cause such as tumor. The term also encompasses secondary causes such as medications (tetracycline, minocycline, lithium, vitamin A, isotretinoin, and growth hormone) and venous sinus thrombosis.
Although this disorder is sometimes called benign intracranial hypertension, we and many other authors prefer the designation idiopathic, as the disease is not benign in its effects on the patient.
Mechanisms. The mechanisms of IIH are still being explored, and multiple hypotheses have been presented. These include decreased resorption and/or excess production of CSF, elevated venous pressure, or decreased leptin levels.
The association with obesity may be due to elevated central venous pressure caused by increased intrathoracic and intra-abdominal pressure or possibly elevated estrogen production in obese patients.1
Types. Pediatric IIH occurs in 2 distinct types. In children younger than 9 years, IIH occurs equally in boys and girls and is not associated with excess weight. In contrast, in older children, there is a female preponderance and an association with excess body weight. Brara and colleagues found that childhood obesity is strongly associated with an increased risk of pediatric IIH.2
Gonadal hormones in the pubertal age group are likely to contribute to IIH. It is also suggested that increased estrogen exposure from use of oral contraceptives is correlated with IIH in females of pubertal age. The disease may also be more severe in this group compared with prepubescent girls.3
Symptoms
The most common symptom of IIH is frequent headache, reported by 90% of patients. Pulsating tinnitus occurs in 58% of patients and is often described as a “whooshing” sound. In Laura’s case, she compared it to a screaming sound. Neck pain, transient visual decrease, and diplopia are also frequently reported. Permanent visual field defects may occur as a result of optic nerve damage from papilledema.4
Treatment
Medical. First-line therapy involves weight loss and oral acetazolamide, a carbonic anhydrase inhibitor. In children, the recommended starting dose is 25 mg/kg per day, with a maximum dose of 100 mg/kg.5 Diuretics such as furosemide can be used alone or in conjunction with acetazolamide.
Topiramate, a weak carbonic anhydrase inhibitor, is sometimes used as an alternative to acetazolamide. Because its side effects include appetite suppression, it may aid in weight loss.6
Surgical. If a patient does not respond adequately to weight loss and medical therapy, surgical treatment may be considered for cases that are intractable or pose a threat to vision.
The main surgical procedures for IIH are optic nerve sheath fenestration (ONSF) and CSF shunting. ONSF is preferred for patients with visual symptoms, whereas shunting is used mainly for those with headaches.
Follow-up. All patients with IIH should have ongoing follow-up for visual field measurements and evaluation of papilledema. Length of treatment may vary according to the patient’s condition, and follow-up appointments are recommended for at least 6 months after optic nerve appearance and visual acuity stabilize.2
Take-Home Points
As the obesity epidemic spreads among children, pediatric IIH is likely to increase as well. Counseling families about the value of weight loss is vital to reducing the incidence of permanent visual loss and may also decrease long-term dependence on medications. Involving a dietitian early in the course of treatment may be helpful in achieving these goals.
___________________________
* Patient name is fictitious.
___________________________
Dr. Gerber is a practicing ophthalmologist, and Ms. Lynn is a certified ophthalmic scribe. Both are at Advanced Ophthalmology of Michiana in South Bend, Indiana. Financial disclosures: None.
___________________________
1 Goldman L, Schafer AI, eds. Goldman-Cecil Medicine, Vol. 2. 25th ed. Philadelphia: Elsevier Saunders; 2016:2362.
2 Brara SM et al. J Pediatr. 2012;161(4):602-607.
3 Sheldon CA et al. Ophthalmology. 2016;123(11):2424-2431.
4 Degnan AJ, Levy LM. AJNR Am J Neuroradiol. 2011;32(11):1986-1993.
5 Albakr A et al. Sudan J Paediat. 2016;16(2):67-76.
6 Thurtell MJ, Wall M. Curr Treat Options Neurol. 2013;15(1):1-12.
Conditions to Consider in a Patient With Suspected IIH
Conditions associated with increased intracranial pressure:
- Intracranial mass lesions (tumor, abscess)
- Increased CSF production (e.g., choroid plexus papilloma)
- Decreased CSF absorption (e.g., arachnoid granulation adhesions after bacterial or other infectious meningitis, subarachnoid hemorrhage)
- Obstructive hydrocephalus
- Obstruction of venous outflow (e.g., venous sinus thrombosis, jugular vein compression, neck surgery)
Conditions associated with optic disc edema:
- Pseudopapilledema
- Papillitis
- Hypertensive optic neuropathy
- Central retinal vein occlusion
- Ischemic optic neuropathy
- Infiltration of optic disc
- Leber hereditary optic neuropathy
- Orbital optic nerve tumors
- Diabetic papillopathy
- Thyroid-related optic neuropathy
Source: Wakil SM et al. eyewiki.aao.org/Pseudotumor_cerebri_(idiopathic_intracranial_hypertension).
|