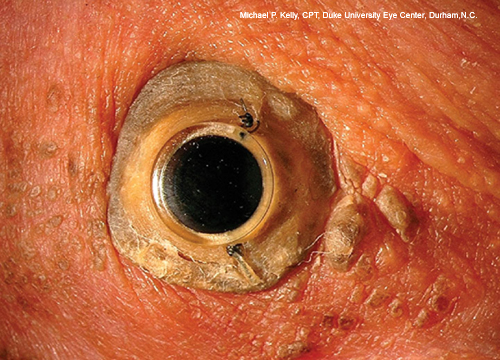
Dohlman Type II Keratoprosthesis
By Natalie A. Afshari, MD, Matthew C. Caldwell, MD, and Michael P. Kelly, CPT, Duke University Eye Center, Durham, N.C.
This article is from November/December 2008 and may contain outdated material.
A 35-year-old man with a history of Stevens-Johnson syndrome (due to a penicillin reaction at age 24) developed corneal vascularization and pannus, reducing his vision to light perception bilaterally.
Several attempts at anterior segment reconstruction and rehabilitation of his left eye resulted in short-lived improvement while the right eye progressed to total ankyloblepharon. At age 28, he underwent placement of a Dohlman type II keratoprosthesis in the right eye, combined with cataract extraction, glaucoma tube placement and blepharoplasty. Visual acuity improved to 20/40 only days after surgery but eventually required YAG laser lysis of a retroprosthesis membrane.
Currently, his visual acuity is 20/20 in the right eye and hand motion in the left. Glaucoma, a common issue in patients with keratoprostheses, is managed with a double-plated Ahmed glaucoma shunt and is monitored by observation of the optic nerve head and assessment of IOP by palpation.
| BLINK SUBMISSIONS: Send us your ophthalmic image and its explanation in 150-250 words. E-mail to eyenet@aao.org, fax to 415-561-8575, or mail to EyeNet Magazine, 655 Beach Street, San Francisco, CA 94109. Please note that EyeNet reserves the right to edit Blink submissions. |