By Ruth D. Williams, MD, With Anne L. Coleman, MD, PhD, and Dale K. Heuer, MD
Download PDF
With the advent of minimally invasive glaucoma surgery (MIGS), glaucoma treatment paradigms are changing. However, the traditional surgical procedures—trabeculectomies and tube shunts—still have an important place in glaucoma management. In this two-part article, Ruth D. Williams, MD, of the Wheaton Eye Clinic, hosts a discussion with Anne L. Coleman, MD, PhD, of University of California, Los Angeles (UCLA), and Dale K. Heuer, MD, past president of the American Glaucoma Society. This month, they share their perspectives on the current status of trabeculectomy surgery, when to opt for it, how to talk with patients about risk, and the importance of postoperative management. Part 2 will appear in the next issue.
Decreasing Number of Trabeculectomies
Dr. Williams: The Medicare database shows that the number of trabeculectomies being performed in the United States is declining. Does that reflect your clinical experience?
Dr. Heuer: Yes. I have had numerous patients over the last five to seven years in whom I historically would have done a trabeculectomy that I would now instead refer to one of my colleagues for a less invasive procedure. So, in my practice (from which I should note that I recently retired), I did see a trend toward fewer trabeculectomies, at least in patients with mild to moderate glaucoma.
Dr. Coleman: We’ve seen that at UCLA, too. I think that there is a role for MIGS in individuals who have earlier-stage glaucoma. In the past, we might have done a trabeculectomy in some of these patients, but now we’re doing a different procedure.
 |
|
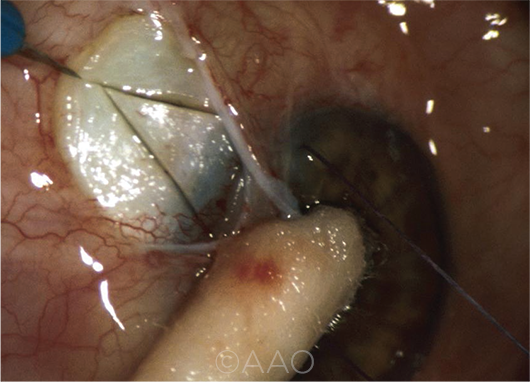
TRABECULECTOMY. The number of trabeculectomies performed each year is on the decline, but it’s still important to learn this technique and keep skills sharp.
|
When to Choose Trabs
Dr. Williams: What are some clinical situations in which you think a trabeculectomy is still the best procedure?
Dr. Coleman: I am still doing trabeculectomies in patients with very advanced glaucoma because I want a very low intraocular pressure. In my hands, I still get a lower eye pressure by performing a trabeculectomy with mitomycin C than with any other procedure.
Dr. Williams: I agree, the best way to get a very low pressure is with trabeculectomy, and with our trend of setting lower target pressures, its role becomes more precise.
Dr. Heuer: I concur, and I think that what we lack is a randomized study comparing trabeculectomy with MIGS procedures. In the absence of that, the best data we have come from a study by Schlenker and coworkers published a few years ago.1 They found that white patients, those with poorer preoperative vision, and those with more advanced glaucoma had better outcomes with trabeculectomy than with the gel stent. Actually, that last factor was only of borderline significance, so we may want to consider the gel stent in our patients with better vision, even those with more advanced glaucoma.
Talking to Patients About the Risks
Dr. Williams: We know that our patients read about the glaucoma treatment options on the internet. In fact, patients sometimes come in telling us which MIGS procedure they want. They are also reading that MIGS procedures have a lower complication rate than trabeculectomy. How does this affect your conversation with the patient regarding the risks of traditional surgery?
Dr. Heuer: I think that the conversation about possible complications with any glaucoma procedure is always a little more protracted than, for example, with cataract surgery, where we have a more predictable outcome. We always have to put the risks and benefits in the context of what the alternative is, and if the alternative is going blind—albeit more gradually from their glaucoma—it makes the decision a little easier. I do think that by preparing patients for the worst, lowering their expectations, we often have a smoother outcome postoperatively—most of the patients end up thinking, “Well, that wasn’t nearly as bad as the doctor said it would be.”
Even with patients for whom we think that trabeculectomy is a better option than the less invasive approaches, it’s still always about risk and benefit. But if the patient feels strongly otherwise or is very risk averse, I may say that, as long as we’re not going to burn any bridges, we can try something else—and do a trabeculectomy later, if needed.
Moreover, another issue is that many of the MIGS approaches are indicated only in combination with cataract surgery, and many of our patients are already pseudophakic or may not even have a cataract.
Dr. Coleman: Another big issue is that with trabeculectomies, it’s important to make sure that the patient understands the long-term risk of endophthalmitis. I think that doesn’t always show up in randomized controlled clinical trials because of the short follow-up. The studies are not usually designed to be long enough to see cases of endophthalmitis that may develop in a patient 10 or more years post-op. One thing I do is make sure that patients who undergo trabeculectomy understand the lifelong need for good hygiene.
Trabs: The Importance of Post-op Management
Dr. Williams: One of the most important skills for successful trabeculectomy outcomes is postoperative management, unlike MIGS, where in most cases, you don’t have a lot to manage afterward. The three of us have done so many trabeculectomies that we’re probably not rattled when we have a shallow chamber or a bleb leak; we have the experience to know how to manage it.
Both of you have been training residents and fellows for a long time. Do you think our glaucoma fellows and residents have seen enough post-op management of trabeculectomies to be comfortable with the procedure going forward?
Dr. Coleman: That probably depends on the training program. At UCLA, our residents still do trabeculectomies. The fellows at UCLA also do a lot of trabeculectomies because our glaucoma faculty still do mainly trabeculectomies and shunts, although fewer than in the past because of the increase in MIGS cases. I think that one of the reasons why individuals choose to do a glaucoma fellowship at UCLA is that they’re aware that we still do a lot of trabeculectomies and shunts.
Dr. Heuer: I think the experience is quite variable. It’s important for anyone going into a comprehensive ophthalmology practice—particularly if they’re not located in a major urban area—to develop a level of comfort with trabeculectomy to be able to manage the complications. Even if a comprehensive ophthalmologist sends her patients some distance to a specialist for the procedure, she might need to be involved in some of the postoperative care and will probably be responsible for the long-term follow-up.
I’d like to think that our training programs are adequately preparing all residents and fellows, but those who are not connected with a county hospital or busy VA hospital may not be getting enough exposure to trabeculectomy.2
Ironically, I think that the fellows, who are training with some of our higher-profile colleagues who do a lot of the less invasive approaches, may be in a kind of a bubble, in which they’re not being exposed to as many trabeculectomies or shunts. This is a loss because they will probably need these skills in two or three years, when some of the patients who underwent MIGS procedures will need to undergo traditional filtering surgery.
Dr. Williams: This is my advice to people in training who have the opportunity to learn trabeculectomy: During this time of excitement about learning the latest MIGS procedure, be just as excited about learning how to do a good trabeculectomy. I think that all three of us would agree that filters are here to stay.
Dr. Coleman: I agree. And I think it’s important to be prepared for the most complicated patients when you’re a glaucoma specialist. Even though trabeculectomy may not be as popular 10 years from now, it might still be the only thing we have for some cases.
___________________________
1 Schlenker MB et al. Ophthalmology. 2017;124(11):1579-1588.
2 AUPO Fellowship Compliance Committee. Exit Survey Reports: Glaucoma 2014-2019. https://aupofcc.org/fellowship-programs-residentssubspecialties/glaucoma; click “Fellow Surgical Volume Report,” then “Procedures reported by Glaucoma Fellows in Exit Surveys 2014-2019.”
___________________________
Dr. Coleman is president of the American Academy of Ophthalmology and a glaucoma specialist at UCLA, Stein Eye Institute. Financial disclosures: None.
Dr. Heuer is past president of the American Glaucoma Society. Financial disclosures: National Eye Institute: S; Santen: S.
Dr. Williams is a glaucoma specialist at Wheaton Eye Clinic, Wheaton, Ill., and the Chief Medical Editor of EyeNet Magazine. Financial disclosures: None.
See the disclosure key at www.aao.org/eyenet/disclosures.
___________________________
NEXT MONTH. In EyeNet’s July issue, the experts continue the conversation, discussing long-term complications, tubes, the importance of individual technique, and the future of filtering surgeries.
___________________________
SUBSPECIALTY DAY. Don’t miss all things glaucoma at Subspecialty Day at Sands Expo/Venetian in Las Vegas, Friday, Nov. 13.