Download PDF
The patient sounded like a broken record, telling his cataract surgeon over and over again that he couldn’t read. But the surgeon was perplexed—the patient had 20/30 acuity and the retina looked fine. “Do you think your machine could help?” the surgeon asked a low vision rehabilitation colleague, who agreed to do microperimetry.
The results were stunning: The patient had a minuscule central island of vision, completely surrounded by a huge scotoma. Finally, there was an explanation for why he could identify one high-contrast letter at a time on an eye chart but had given up trying to read the morning newspaper.
This patient’s experience provided a critical insight: “What you see with the ophthalmoscope or on the OCT—or what size letters the patient reads on an eye chart—is not the whole story,” said Lylas G. Mogk, MD, medical director of the Centers for Vision Rehabilitation at the Henry Ford Health System in Grosse Pointe Park and Livonia, Mich.
Microperimetry can help the ophthalmologist solve puzzling problems presented by patients like this one, whose visual function is inconsistent with visual acuity. (For those without access to microperimetry, a more generally available alternative is a 10-2 conventional perimetry test.) Moreover, microperimetry can be used by low vision specialists to coach their patients in making the most effective use of their remaining vision. And it is beginning to find applications in broader clinical practice, as well.
What Is Microperimetry?
Microperimeters map the pattern of a patient’s retinal sensitivity onto an image of that individual’s fundus. They measure the patient’s response to light stimuli at various retinal points and superimpose that data on an image captured by scanning laser ophthalmoscopy (SLO) or fundus photography to precisely identify areas of impaired or preserved function. Current models employ eye-tracking technology to correct for eye movement, allowing accurate testing and retesting of the same retinal point, said Samuel N. Markowitz, MD, associate professor of ophthalmology and director of the Low Vision Rehabilitation Program at the University of Toronto, Ontario.
Most frequently used in patients with low vision due to retinal disease, microperimeters can reveal the correlation of residual vision and functional vision in a precise way that standard automated perimetry and optical coherence tomography (OCT) cannot, Dr. Markowitz said.
Microperimetry makes it possible for the physician to identify scotomata that would otherwise be undetectable because they do not correlate with fundus appearance, said Dr. Mogk. “It tells us which part of the macula is seeing or not seeing, or in the case of a stroke patient, for instance, which part of the macula the brain is not recording. Microperimetry helps us look at the world through the patients’ eyes, so to speak, which makes it extremely valuable for rehabilitation.”
|
Central Island
|
 |
|
Microperimetry revealed extensive areas of dense scotoma (DS) and variable scotoma (VS) surrounding fixation (red circle). The patient’s visual acuity is 20/100.
|
Microperimetry and Low Vision Rehab
No matter how poor the patient’s vision is, residual functional vision can be used more effectively through rehabilitation interventions, said Dr. Markowitz. Microperimetry has several applications that are helpful in guiding rehabilitation efforts and teaching patients to locate and maximize use of their areas of best vision.
Mapping the macula. It can be difficult for patients with central scotomata to fixate on the targets used in standard perimetry. In contrast, microperimetry allows mapping without central fixation, which makes it extremely beneficial for evaluating central vision loss, said Dr. Mogk. This can shed light on cases in which measured visual acuity is good but function is poor, or when you know the pathology but don’t fully understand how it’s affecting a person’s vision, said Dr. Mogk. If you’re using acuity as your only gauge, you might celebrate acuity of 20/40 or 20/70 in a low vision patient, she said. “But what if that patient has a big paracentral scotoma just to the right of fixation that precludes fluent reading left to right, or a ring scotoma with only a small island spared?” Microperimetry can elucidate patterns like these, she said, even if it doesn’t dramatically change the treatment of the disease.
The technique is particularly useful with kids, added Janet S. Sunness, MD, specialist in low vision, macular and retinal disease, and visual function testing, and medical director of Hoover Services at Greater Baltimore Medical Center in Baltimore, Md. “Mapping their blind spots with microperimetry is much easier for them because it’s like playing a video game.”
Picking a PRL. Patients who lose central fixation automatically pick the next-best spot, known as the preferred retinal locus (PRL). “Most patients are unaware of where that spot is,” said Dr. Mogk, “so they have to move their heads around each time until they find it. Microperimetry provides a shortcut: Once the test shows the scotoma location, size, and position relative to the PRL, the therapist coaches the patient to find the PRL quickly and use it efficiently. First, they use flashcards to demonstrate where it is and then help the patient apply it to tasks.”
Fixation stability is the ability to keep the eye fixated on the PRL. With microperimeters, the low vision practitioner can estimate fixation stability at the PRL, which allows logical planning of interventions aimed at improving functional vision, said Dr. Markowitz. Sometimes, prism glasses are used to redirect images toward the PRL. Other patients find PRL training with an occupational therapist successful and less expensive, added Dr. Mogk.
Patient education and training. The visual perimetry “map” provides a valuable patient education tool, said Dr. Sunness. “We want to see where they are fixating and the nature of the blind spots around the fixation,” she said. “Once we have that information, we know how to counsel the patient and teach scotoma awareness—where the blind spot is and how to move it out of the way more effectively.”
The strategy of rehabilitation depends in part on that relationship between the PRL and scotoma, agreed Dr. Mogk. For example, a patient with a central scotoma and PRL to the left of it might use a “ticker tape” strategy for reading: moving the print right to left, rather than moving the eyes left to right. Or, someone with a PRL superior to the scotoma might position a book straight ahead, using separate reading glasses, rather than looking down through bifocals in a standard reading position.
Microperimeter as a trainer. “Some microperimeters have a biofeedback module that trains the eye to use a better peripheral location,” said Dr. Markowitz. The program provides auditory feedback when the patient approaches the desired fixation target.
However, Dr. Mogk’s institution does not use the device in this way. First, the rehabilitation specialists there don’t attempt to change the patient’s PRL; and, second, they find that training in the use of the PRL is best done in the real world. “Our occupational therapists do PRL training in the context of actual tasks, rather than with the patient’s head fixed in a machine.” In addition, transportation back to the center to regularly use the machine could be a real issue for these low vision patients, she said.
 |
|
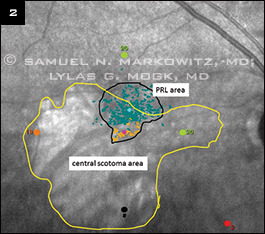
PRL MAPPING. (2) The green area in this plot from a MAIA microperimeter delineates the patient’s preferred retinal locus (PRL) and fixation stability. (3) With a preferred retinal locus superior to scotoma on the retina (inferior in patient’s field), the patient has to look above the object of interest to see it best.
|
Expanding Clinical Uses
Microperimetry also holds promise in other clinical arenas, in both practice and trials. Regardless of the application, Dr. Sunness emphasized the importance of clearly defining the information you need to obtain from microperimetry before choosing from a menu of test patterns and gating strategies. For some patients, you will simply need to find a blind spot and not need to check lots of points, she said. But for others with better vision, you will want to do more subtle testing.
After anti-VEGF injections. Dr. Sunness finds microperimetry useful in evaluating patients with wet age-related macular degeneration who are on anti-VEGF medications. “Before Lucentis, Avastin, and Eylea, patients generally ended up legally blind with a scar [in the fundus] that was very obvious,” she said. Today, vision is better preserved with these medications, but people often have blind spots in their visual fields that aren’t clinically apparent. “Microperimetry helps identify them. Then all the patients may need is a little more scotoma-awareness coaching, a stronger spectacle add, and/or a little more light, and we can often get them back to reading regular print again.”
Fixation and function. In some patients, visual function is not restored despite successful structural repair, such as reattaching a detached retina or opening a channel for aqueous flow in glaucoma, said Dr. Markowitz.
But microperimeters can help reveal the underlying reason for the persistent functional impairment, he said. After closure of a macular hole, for example, retina specialists rely on OCT to see that tissues are lined up properly. However, recent research shows that fixation stability is a more reliable predictor of visual acuity following this type of surgery.1 Likewise, visual acuity may worsen after glaucoma surgery, said Dr. Markowitz, because surgery has broken the balance between fixation stability and the PRL.
As a measure in clinical trials. Current and future clinical trials may find increasing utility for this technology, said Dr. Sunness. She gave the example of ProgStar, a study of the natural history of Stargardt disease, which was recently launched at nine centers by the Foundation Fighting Blindness. “Microperimetry will be used to track the progression of retinal function loss during the study,” she said, “because with Stargardt, it’s the only way to get this information.”
Looking ahead. Although their use is still fairly rare in mainstream ophthalmology, microperimeters may be used increasingly to evaluate visual function and to further guide interventions in a variety of conditions. The interest in this new technology is growing; for example, a special issue of the Canadian Journal of Ophthalmology dedicated entirely to microperimetry is planned for October 2013. Watch for it.
___________________________
1 Tarita-Nistor L et al. Invest Ophthalmol Vis Sci. 2009;50(1):84-89.
___________________________
Drs. Markowitz, Mogk, and Sunness report no related financial interests.
Types of Microperimeters
Priced in the range of $60,000 to $70,000, microperimeters currently on the market are similar in many regards, said Dr. Markowitz. All display PRLs, have automated tracking of the retina, and automatically calculate fixation stability. However, he advised using the same instrument consistently to follow a patient because the decibel scales are not directly comparable between devices.
Rodenstock. Dr. Mogk called the Rodenstock the Cadillac of SLOs. Although no longer in production, a number are still in use. Unlike other microperimeters, which superimpose a grid pattern of stimuli onto the retina with points showing up in certain places, the technician chooses where to put the targets on a “blank” macula.
Nidek MP-1. Introduced in 2005, the Nidek MP-1 was the first microperimeter to reach a clinical market. It also has a biofeedback module for training fixation locations, said Dr. Markowitz.
Optos OCT SLO. Currently the only device that incorporates microperimetry, SLO, and spectral domain OCT into a single instrument, the Optos OCT SLO recently received FDA approval for use as a microperimeter. “It provides a nice correlation between structure and function—where exactly the PRL is on the retina and how the retina looks on OCT at the PRL location,” said Dr. Markowitz. Other benefits are the possibility of quick hybrid perimetry and good imaging without dilation, said Dr. Sunness. A U.S. trial is currently under way to assess the precision of the device’s microperimetry function in a number of retinal disorders.
MAIA. With the widest range of sensitivity, said Dr. Markowitz, the MAIA (CenterVue), which stands for macular integrity assessment, is particularly well suited for residual fields testing in glaucoma. It also has a biofeedback module for training and unique software that makes it possible to identify normal, age-related decreases in sensitivity.
|