Download PDF
It’s not surprising that the gadget-filled world of ophthalmology would be a fertile breeding ground for the creation of clinical applications, or “apps.” These ophthalmic apps are transforming smartphones into medical devices and challenging ophthalmologists not only to keep pace with their rapid development but also to differentiate the good from the questionable.
Early Adopters
“Physicians were early adopters of mobile technology,” said Iltifat Husain, MD, at the Wake Forest School of Medicine in Winston-Salem, N.C. “Remember using Epocrates and other medical references on your PDA [personal digital assistant] more than a decade ago? The introduction of the iPhone 3G, with its apps and the App Store, represented the natural extension of these capabilities.” And as it turned out, Dr. Husain said, “Some of the first medical applications involved ophthalmology—for example, apps to test visual acuity.”
Blistering Pace of Development
As of 2014, there were 182 ophthalmology-related apps available through the Apple iTunes Store.1 Functions range from simple flashcards to patient assessment tools to virtual surgery applications and imaging capabilities; practice management apps are available, too2 (see “Practice Management Apps for the Ophthalmic Office” in next month’s issue of EyeNet).
Here’s a brief sample of some current clinical apps.
- AAPOS Vision Screening, which is derived from the basic distance Vision Screening Kit created by the American Association for Pediatric Ophthalmology and Strabismus.
- Eye Handbook, which features clinical tools, physician and patient education material, forums for interaction with other physicians, and a large YouTube video library. It also hosts material from the Academy, including a direct link to EyeWiki and the Academy’s Summary Benchmarks (see “A Closer Look at Eye Handbook”).
- Eye Emergency Manual, which provides a guide to recognizing and managing common eye emergencies.
- Eye Pro, which contains such features as the Astig PLOT (to help users plot and calculate surgically induced astigmatism in a series of eyes), a cataract surgery outcomes calculator, a toric IOL calculator, and a biometry formula for post-LASIK/PRK eyes.
- SightBook, a vision assessment app that supports standardized and frequent vision testing. It is part of a system that integrates the app with an Internet-based vision care network and website.
Another angle. Imaging apps are also transforming the ophthalmology landscape. Shizuo Mukai, MD, a retina specialist at the Massachusetts Eye and Ear Infirmary, has spent the last decade searching for simple, affordable alternatives for fundus photography systems. His quest began in 2004 with off-the-shelf digital cameras and then shifted to smartphones.
“The smartphones not only had good cameras, but the light source also was right next to the lens,” said Dr. Mukai, who studied both photography and biology as an undergraduate. “David Kim, MD, my fellow at the time, stumbled upon an amazing app, the FiLMiC Pro, which allows you to control the iPhone camera like a manual camera, with full control over focus and exposure as well as the intensity of the light. This really clinched our ability to take high-quality fundus photos with a smartphone.”
Dr. Mukai and his colleagues published a report on the technique, which requires an iPhone 4 or later, the FiLMiC Pro app, and a 20-D lens.3 He noted that his residents and fellows use the app both in the emergency room and at the bedside. For example, a resident can email the fundus photograph to the fellow on call for retina, who can then confirm the diagnosis.
“This technique also has implications for developing countries,” said Dr. Mukai. “I have been in Uganda, where they may not have running water, but they do have iPhones. We taught this technique there, and now they can take fundus photographs and send them out either by the Internet or through mobile telephone networks.”
Users Beware
While apps are changing the way that physicians practice medicine, the app development field can be likened to the Wild West. For instance, in 2014, the majority of ophthalmic apps lacked community user ratings and had 3,000 or fewer downloads. In addition, only 37% had documented qualified professional involvement in their development.1
Notably, recent research has found considerable variability in the optotype accuracy of smartphone-based Snellen visual acuity charts (see “Accuracy of Snellen Apps”).
Given this, how can physicians even begin to keep tabs on and assess new apps?
Apply a filter. One source for learning more about the latest apps is www.iMedicalApps.com, which Dr. Husain founded in 2009 as a 24-year-old medical student.
At that time, he said, “No one was explaining which apps were useful and which were not, or how physicians and patients could best use the apps to advance health.” Dr. Husain launched the website to address this gap, and it features physician editors and a team of medical professionals who provide reviews, research, and commentary on mobile medical technology.
Probe further. Dr. Husain acknowledged that there is surprisingly little information for physicians on the validity and usefulness of new and existing apps. “I recommend that ophthalmologists search their journals and PubMed for any new information and seek out reviews in the App Store—the more specific, the better,” he said. “The best apps are those that are evidenced based.”
The FDA Weighs In
The fact that some mobile apps are transforming smartphones into medical devices hasn’t been lost on the FDA.
Earlier this year, the agency updated its guidelines on the topic, which focus on the small subset of mobile apps that meet the regulatory definition of “device” and are “intended to be used as an accessory to a regulated medical device” or are designed to “transform a mobile platform into a regulated medical device.”4 Mobile medical apps that undergo FDA review are assessed using the same regulatory standards and risk-based approach that the agency applies to other medical devices.
“We are focused on the functionality of the app, regardless of the mobile platform,” said Bakul Patel, MS, MBA, who is at the FDA. “Consequently, we aren’t concerned with the majority of apps, most of which are educational or informational. However, for example, if an app is designed to detect a retinal detachment, it needs to be regulated by the FDA to ensure its safety and effectiveness.”
During the past decade, the FDA has cleared more than 100 mobile medical apps. “With this clearance, we are giving physicians information so they know which devices to trust,” Mr. Patel said. “We are excited about the technology, but we need to make sure [apps] work as intended if ophthalmologists are going to rely on them to make diagnostic decisions.”5
A Closer Look at Eye Handbook
Eye Handbook made its debut in 2009, when Dr. Shah and his colleague Ken Lord, MD, began it as a small resident project at the University of Missouri in Kansas City. Since then, the free app has had more than 1 million downloads and 300,000 unique users.
Eye Handbook serves as an aggregator and brings together a variety of content, including patient education materials, instructional videos, and myriad clinical testing tools. “Using the app, our residents can check a patient’s visual acuity and color vision; they also can measure the pupil and use the flashlight to check the pupil response,” Dr. Shah said. “With the blue light from the smartphone, we can do a fluorescein test to check for corneal abrasions. Subsequently, by using the camera function, photos of the eye exam, including a laceration of the eyelid or corneal abrasion or even fundus photos, can be emailed to colleagues for a nearly instantaneous second opinion.”
For a tour through the Eye Handbook, view the Multimedia Extra below.
|
Changing the Paradigm
Dr. Husain anticipates that apps will continue to be introduced at a rapid pace. “I tell physicians that the next space for innovation is mobile technology—and instead of waiting to see how these apps develop, they must take an active role in creating them.”
Citing the evolution of electronic medical records, “which didn’t have much input from physicians,” Dr. Husain urged ophthalmologists to “take a more engaged approach to information technology in the medical workplace. It will be good not only for physicians but for patients as well.”
No going back. Vinay A. Shah, MD, at the Dean McGee Eye Institute at the University of Oklahoma, observed that younger physicians, especially those in training, are increasingly using their smartphones for both personal and professional efficiency.
Steven M. Christiansen, MD, a first-year ophthalmology resident at the University of Iowa, is a perfect example of this transition. Three years ago, Dr. Christiansen created a website (www.eyesteve.com) to keep ophthalmologists up to date on the latest ophthalmology news and encourage them to use social media. He sees a big shift in how the acquisition of information is occurring. “In prior generations, it was important to have basic science and clinical knowledge memorized, but with rapid changes in medicine, it is vital to also be able to quickly find the information rather than simply memorizing it.”
Although Dr. Christiansen acknowledged that memorization is still crucial, apps that can locate information quickly are changing the educational process, he said. “Apps are transforming the way we live our lives. When I come across an unmet need, whether personal or professional, I always ask myself, ‘Is there an app for that?’ Oftentimes there is—and if there isn’t, it is likely someone is developing it.”
___________________________
1 Cheng NM et al. Telemed J E Health. 2014;20(4):385-387.
2 Zvornicanin E et al. Acta Inform Med. 2014;22(3):206-209.
3 Haddock LJ et al. J Ophthalmol. 2013;518479.
4 Mobile Medical Applications: Guidance for Food and Drug Administration Staff. Accessed June 8, 2015.
5 The FDA’s list can be accessed at www.fda.gov/MedicalDevices/ProductsandMedicalProcedures.
___________________________
Steven M. Christiansen, MD, is an ophthalmology resident at the University of Iowa in Iowa City and founder of www.eyesteve.com. Relevant financial disclosures: None.
Iltifat Husain, MD, is assistant professor of emergency medicine and director of the Mobile App Curriculum at the Wake Forest School of Medicine in Winston-Salem, N.C. He is also the founder and editor-in-chief of www.iMedicalApps.com. Relevant financial disclosures: None.
Shizuo Mukai, MD, is associate professor of ophthalmology at Harvard Medical School and associate scientist and surgeon at Massachusetts Eye and Ear Infirmary in Boston. Relevant financial disclosures: None.
Bakul Patel, MS, MBA, is associate director for Digital Health in the FDA’s Center for Devices and Radiological Health. Relevant financial disclosures: None.
Vinay A. Shah, MD, is clinical associate professor of ophthalmology at the Dean McGee Eye Institute at the University of Oklahoma and a vitreoretinal specialist in Oklahoma City. Relevant financial disclosures: Cloud Nine Development: O.
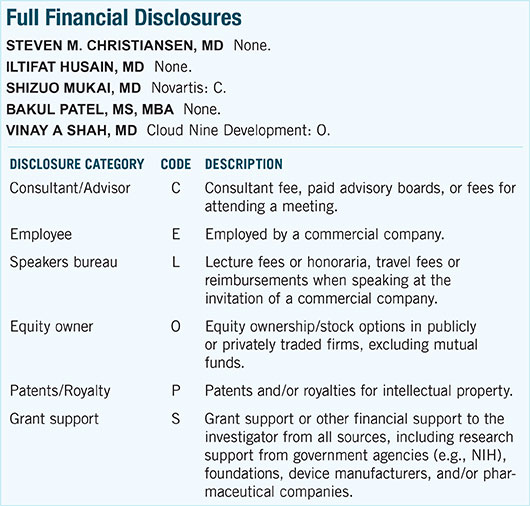
For full disclosures and the disclosure key, see below.