By Robert F. Melendez, MD, MBA, Mike Betzen, MBA, and Tiffany Venditti, COMT
Download PDF
In an environment of decreasing reimbursements, many practices are looking for ways to improve clinical efficiency. At our practice, we tried changing the way that technicians work with the ophthalmologists and optometrists. There were some initial challenges, but the new arrangements have boosted patient throughput.
Why We Chose a Pod System
When our practice reviewed its processes, we identified a number of problems with our traditional use of technicians, where each tech is assigned to a specific doctor. One common issue: A technician might have to wait for a patient to be ready for a workup.
Our solution was to assign techs to a group, or “pod,” of providers. And with a nod to our specialty, we refer to this internally as the “eyepod” system.
How We Got Started
Our practice is made up of 44 ophthalmologists and optometrists representing every subspecialty, and we have a wide variety of patients.
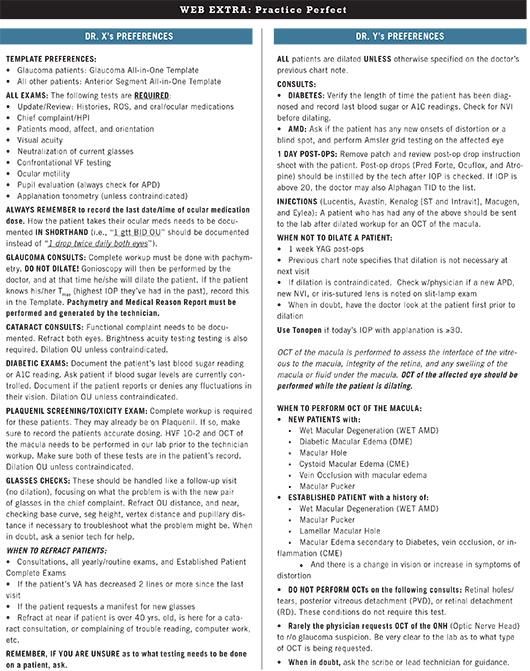
We created cheat sheets listing each provider’s preferences. All our providers were asked what tasks they wanted the technicians to perform in the initial workups for different types of patients. We used this information to create a one-page preference sheet for each provider, which technicians can use as a guide when starting the eye evaluation or workup for one of that doctor’s patients (see sample below). We found that asking providers about their preferences was a key step in gaining their buy-in for the pod system.
Physicians provide personal training to technicians in their pod. Although much can be learned from the cheat sheets and the physician feedback that takes place during the course of the regular working day, we also suggest that time be set aside for some additional training of technicians—even those who are experienced. We recommend that each physician meets with a group of technicians to discuss what steps to take with five common cases seen in the clinic. For example, when a patient presents for a cataract evaluation, there are specific tests that we want completed, such as corneal topography and a brightness acuity test. By talking technicians through these tests, a physician can help them to understand the rationale behind performing each one. As time progresses, they can meet again to discuss five additional types of case.
(click to expand)
Strengths of the Pod System
The system is fairer, and that promotes teamwork. Our new system helps to ensure that technician resources are applied equally to all providers. It also creates a level playing field for the technicians. Under the traditional model, some technicians may complain that they are working harder than everyone else, and there may be a perception that tech X does not help tech Y. In the pod environment, on the other hand, all techs must take the next available patient—they can’t say that they are waiting for “their” next patient to arrive. This creates an environment where everybody is seen to be pulling his or her own weight.
Boosts efficiency. The workup of patients proceeds in a more consistent, timely manner, which in turn helps the overall clinic run more smoothly. Patients have quicker access to the technician, which often translates into quicker access to the provider, resulting in less wait time and a shorter visit.
Improves patients’ perception of the practice. In the past, when techs were assigned to support a specific doctor, they sometimes had downtime while waiting for that doctor’s next patient. This led to some patient complaints that they had to wait while some techs appeared to be standing around. Under our new system, it’s all hands on deck, with one stack of charts and almost always a patient ready to be worked up. Patients now perceive that all the staff members are busy.
Prompts technicians to enhance their skill set. Now that technicians work for a variety of providers, they are challenged to broaden and improve their skills. In the traditional system, when a technician had shortcomings, the provider may have picked up the slack. For example, the doctor may know that her technician does not take a good IOP but otherwise does a great job. Rather than rocking the boat by telling management, the doctor may simply redo the pressure check, and the tech may not even be aware that improvement is needed. With the pod system, technicians no longer get this type of free pass; they need to work on meeting all of their job requirements. Consequently, the patient is more likely to encounter a better-trained and well-rounded technician.
Identifies technicians who are underperforming. If a tech was underperforming under the old system, he or she might have flown below the radar. The new system helps to identify these individuals so management can take appropriate action.
Makes the practice more robust. Under the new system, we have had very busy clinics operate smoothly even when down by a technician.
Three Tips for Techs
Our mantras for technicians are:
1. Always do more rather than less.
2. If you think about it, then do it. (For example, should I do a corneal topography on this patient?)
3. If you do not know how to do something, ask.
|
There May Be Some Initial Problems
Providers may be frustrated by variable skill sets of technicians. For providers, the primary drawback of the pod system is inconsistency of technical support. Some technicians have better innate abilities, some have more experience, and some strive to do more than others. In the pod system, especially in the beginning, it is likely that the provider will work with some technicians who are not familiar with the details of his or her clinic. Naturally, this can be frustrating and cause a negative perception of the pod system. Although this issue can usually be resolved through use of preference cheat sheets, it is also important for providers to have some flexibility and willingness to tolerate a degree of temporary inconsistency.
Providers may not be ready for increased patient throughput. Another drawback is that there can be a disparity between the number of patients ready to be seen and how fast the provider can see them. When we introduced the new system, it was not unusual for the patients to be worked up more efficiently than before, and some providers felt they were running behind. Providers may have to tweak their templates to address this.
Technicians may not like going beyond their comfort zone. The transition to the new system may require the technicians to learn more than they had anticipated. Ultimately, this is a good thing, but in the meantime, individual technicians can be frustrated and embarrassed if they lack the knowledge to work in the clinic of a provider who is new to them.
Technicians may stress if they’re expected to police their peers. Although the pod system is more conducive to teamwork, that doesn’t mean everybody will immediately become a team player. Those techs who are quicker to embrace the new arrangements may find it unnerving if they feel like they’re expected to “tell on” techs who don’t appear to be pulling their weight.
Patients may be frustrated by initial problems. During the transition period, patients may encounter a technician who is not yet competent in performing the tests requested by a particular provider. Thus, the patient may be subjected to retesting or a longer exam.
Newly hired techs face a steeper learning curve. Since technicians will be expected to perform a wider variety of tests and learn to work with more than one provider, new hires will need additional training, but the lead technician can help to address that.
Conclusion
Generally, we have received buy-in from technicians and providers. The techs like it because it is more of a team approach, and it distributes work more equally. And rotating the techs in different clinics keeps their skill sets sharp. The providers have noticed that there are nearly always patients ready to be seen. We also have concluded that the system works best when the types of clinics are similar.
The future of medicine is about quality, efficiency, and cost control, and we will very likely need to learn to do more with less. One way to achieve that is to use valuable technician resources more efficiently.
___________________________
The authors work at Eye Associates of New Mexico, a practice with 15 locations throughout the state.
Robert F. Melendez, MD, MBA, is a partner and specializes in cataract and refractive surgery. Financial disclosures: None.
Mike Betzen, MBA, is a regional director. Financial disclosures: None.
Tiffany Venditti, COMT, is a team leader and ophthalmic trainer. Financial disclosures: None.