By Annie Stuart, Contributing Writer, interviewing Elizabeth A. Bradley, MD, Michael P. Grant, MD, PhD, and Samir Mardini, MD
Download PDF
Few procedures rival the intricacies of facial transplants, which have been completed just 38 times around the world, including 13 times in the United States, according to Samir Mardini, MD, at the Mayo Clinic in Rochester, Minnesota. The first—and so far sole—facial transplant at the Mayo Clinic took place in 2016. The procedure took 55 hours and involved more than 100 people, including 9 surgeons, said Elizabeth A. Bradley, MD, also at the Mayo Clinic.
The only way to be successful with such a procedure is to have a well-trained, invested, and collaborative team that’s undergone intensive training, said Dr. Mardini. He added that having an oculoplastic surgeon as part of this team is essential for ensuring optimal results. “With a face transplant, there are many issues related to the eyes, including orbital reconstruction, eye protection, and visual acuity.”
Patient Selection Is Pivotal
Candidates for facial transplants are most often patients with severe burns, ballistic trauma, animal bites, congenital deformities, or neoplastic conditions.1 Appropriate patient selection is the No. 1 priority, said Dr. Mardini, and the selection process should include the following.
Evaluation of deformity. Facial transplant candidates have significant functional and aesthetic deficits that are beyond the scope of what other traditional methods can address, said Dr. Bradley. For example, Dr. Mardini said, these individuals often have severe facial deformities that involve facial sphincters such as eyelid or oral sphincters, which are quite challenging to reconstruct successfully with conventional methods.
Thorough screening. It is critical that patients undergo a rigorous, multidisciplinary mental and physical screening, said Dr. Bradley. “For patients, a face transplant is a long haul, and they need to have a supportive care system and understand the enormous commitment involved.” The Mayo Clinic has a transplant psychiatrist and social workers who will be integrally involved in screening these patients and guiding them through education, rehabilitation, and postsurgical care, said Dr. Mardini.
Contraindications. “If anyone on the team has a sense that the patient doesn’t fully understand the benefits, risks, and implications—including lifelong immunosuppression, major surgery, and rehabilitation—they will not be listed for a face transplant,” said Dr. Mardini. Contraindications include being medically unfit or noncompliant, he said. Relative contraindications include different forms of addiction, including smoking and alcohol abuse, which could interfere with the surgery or aftercare.
The Mayo Clinic patient “had gained much maturity and showed no signs of residual mental health issues” 10 years after he had attempted suicide with a gun, Dr. Bradley said. “For these reasons, we felt he should be considered a candidate for face transplantation.”
What about blindness? Should blind patients be eligible for face transplants? “This has been a subject of debate,” said Dr. Bradley. She explained that there have been concerns that early physical signs of rejection such as swelling and skin erythema might be missed, as well as the contention that the blind are less susceptible to others’ reactions.
“However, blind patients are perceptive and can sense people’s reactions without visual stimuli,” she said. As for signs of rejection, said Dr. Mardini, no patient will undergo the process without having a good social support network, which can help with monitoring. Moreover, blind patients may notice warmth or changes in their skin texture, Dr. Bradley added.
 |
|
POSTSURGERY. Dr. Mardini checks in with the team’s first facial transplant recipient, who has since regained his ability to smell, breathe, and eat.
|
Global Periorbital Goals
“Technically, we are able to transfer any structure, including different tissue types such as bone, muscle, and nerves,” said Dr. Mardini. But every anatomic defect is unique, so each facial transplant is individualized for the patient, he said. The periorbital aspects of the surgery are also unique depending upon what is missing or dysfunctional.
Function, protection, aesthetics. For the most part, everything in the face requires functional animation, said Dr. Mardini. For example, restoration of facial anatomy is needed for clear speech and vision, mastication of food, and air humidification.1
“With face transplants, you’re either transplanting everything or transplanting a part, but the part that is native to the patient needs to be technically well connected to the transplanted part so that it becomes functional,” he said.
Goals for periorbital area. “In broad terms, two main goals with composite tissue transplantation in the periorbital area are protecting the eyes and making the periorbital area look as normal as possible,” said Michael P. Grant, MD, PhD, at the University of Maryland School of Medicine in Baltimore. “The goal is to replace all damaged layers of tissue—including conjunctiva, skin, and levator tendons—to allow patients to open and close their eyes normally.”
Eyelid closure. A full transplant involves all the skin of the face from the forehead down to the neck, said Dr. Bradley, which means the eyelids are transplanted as well. “With full eyelid transplant, the concern is the recovery of the blink because it is so important for corneal health,” she said. “These patients may have impaired blink until reinnervation happens, which usually occurs at 6 to 8 months and earlier if the nerves are attached very close to the eyelids.”
One factor that may help with eyelid closure in volitional and reflex blink is the replacement of contracted eyelid tissue.2 The recipient nerves also need to be strong enough to innervate the transplanted eyelids and animate closure, said Dr. Mardini. In reattaching facial nerves, Dr. Grant recommends going out as far as possible on each branch to minimize the time for regeneration. “If you graft the branches as far distal as possible, that cuts your time for reinnervation. That is the single most important thing you can do to help preserve or improve blink.”
Impact on vision. Many patients who have severe facial injuries have problems with their vision, said Dr. Grant. “Some have structural problems with their eyes, often from the originalinjury, resulting in reduced vision. Others have damage to their eyelids or conjunctiva, which results in problems with the ocular surface and exposure that can also diminish vision. Restoring a normal ocular surface can potentially reverse some of these problems and maximize the patient’s visual acuity.”
Dr. Grant and his colleagues currently have a recipient listed for a face transplant who has serious bilateral scarring in the periorbital region. Multiple previous procedures were unsuccessful at completely closing both eyes, resulting in chronic dry eye and ocular surface disease. “During his facial transplant, we will remove his existing eyelids but preserve as much conjunctiva as possible. From the donor, we’ll take both upper and lower eyelids and as much conjunctiva as possible,” Dr. Grant said. “Although the patient currently has useful but reduced vision in both eyes, I believe we can significantly improve his vision by restoring the health of the ocular surface.”
Preserving sight. In the Mayo Clinic case, the patient had become blind in 1 eye due to ballistic trauma, but he had intact vision in the other eye. “Because we needed to do major orbital reconstructive surgery, my No. 1 goal was to make sure he didn’t wake up blind in the other eye,” said Dr. Bradley. “Our repair of his enophthalmos involved the insertion of custom-made implants. During the insertion process, pressure is applied to the orbital soft tissues. If too much pressure is applied, it is possible to cause a severe optic neuropathy with blindness. From a vision standpoint, that is the part of the case I was most concerned about.”
Issues With Immunosuppression
Patients who have undergone a facial transplant risk not only rejection but also significant long-term consequences, including cancer, opportunistic infections, metabolic disorders, and death. But “as immunosuppressive strategies improve, I think face transplants will become a more widely accepted solution for severe midfacial injuries involving the periorbital area,” said Dr. Grant.
Hospital-acquired infections. On average, face transplant patients undergo anywhere from 1 to 6 revisions, requiring 1- to 3-day hospitalizations, said Dr. Bradley. Patients on immunosuppressants are at greater risk of hospital-acquired infections, so the stakes are much higher, she said.
Risks of rejection. “Currently, we have to be very concerned about rejection, said Dr. Grant. “Skin is very antigenic, and almost all patients have episodes of rejection.” These episodes can produce scarring or complete death of the transplanted tissues, including eyelids, added Dr. Mardini. At Mayo Clinic, “our patient had 1 episode of acute rejection that we caught early and treated,” he said. It quickly resolved.
Catching rejection early. The Mayo Clinic team had transplanted another part of the donor tissue into the patient’s groin area, which created a sentinel flap area for routine biopsies. “From these biopsies, we had picked up that he had a mild form of rejection,” said Dr. Mardini. “We then biopsied his face, which correlated with a finding of rejection, and treated him, even though we had not picked up clinically that he had a problem with his face.”
|
Face Transplant Challenges
“What made our surgery complex was transplanting most of the bones of the face with the overlying soft tissues,” said Dr. Mardini. “We transplanted the nose and cheeks and all the muscles below the eyelids.” The partial transplant, added Dr. Bradley, involved tear drainage systems, the orbital rims, a portion of the floor of the eye socket, and soft tissue dealing with telecanthus—attachments between the eyelids and the nose.
Isolating and connecting nerves. Because the forehead and eyelid skin were preserved, it was necessary to preserve function in those parts, said Dr. Mardini. “The first thing we did was isolate all the facial nerve branches on both sides of the patient, preserving the function of forehead movement and elevation as well as upper and lower eyelid closure. We then used all the other nerve branches below that to provide nerve supply to the transplanted organ.”
Dr. Mardini added, “We connected the infraorbital nerves and inferior alveolar nerves to get supply to the cheek, upper and lower lips, and the chin as well as the teeth of the transplant. All the parts of the face that were transplanted became functional, plus the patient maintained the eye closure and forehead movement that he had before the procedure.”
Connecting other tissues. The Mayo Clinic patient had his own eyelids, lacrimal gland, and lacrimal drainage system. The tear sac was completely obstructed on one side and partially obstructed on the other. “When we transplanted parts of the nasal bone, maxillary bones, soft tissues of the cheek, chin, and upper and lower jaw, we connected eyelids and the drainage system that he had to the transplanted one,” said Dr. Mardini. “This allowed his lacrimal gland to release tears that lubricated the eyelid and moved through the canaliculi to his lacrimal sac, which was connected to the donor lacrimal sac and drained into the transplanted nose.”
Addressing unique issues. The Mayo Clinic case posed unique periorbital issues including telecanthus and lack of a nose, which meant there was nothing for the soft tissues to attach to, said Dr. Bradley.
Telecanthus. “To address this, we secured our patient’s medial canthal tendon to the donor’s robust medial canthal tendon, which was still attached to the donor’s nasal bones,” said Dr. Bradley. As a result, said Dr. Mardini, today the patient does not have such a wide distance between his medial canthal tendons.
Lacrimal system. Lack of a nose “also meant our patient didn’t have an intact lacrimal system on either side,” said Dr. Bradley. It’s important to remember that a blockage of the lacrimal sac can increase the threat of infection in an immunocompromised patient, she said. “In our case, we were putting in an alloplastic implant, and we knew an infected sac sitting right next to foreign material could pose a threat to the implant.”
Swelling. The initial surgery caused massive swelling, said Dr. Bradley, so the surgical team deferred all of the lacrimal drainage system work and the orbital surgery. “We didn’t want to add any more volume into his orbit at that point,” she said. “Because the patient was so swollen, we kept all of the patient’s and donor’s skin to close the wound.”
Secondary procedures. Dr. Mardini had previously reconstructed the orbital floors with titanium plates, screws, and mesh following the initial trauma. “We removed all the material and reconstructed the orbital floors and medial walls with a synthetic implant about 6 months after the face transplant procedure,” he said. During the secondary procedure, the surgical team also performed lacrimal drainage surgery and telecanthus and infraorbital nerve repairs and resected some excess skin, said Dr. Bradley.
One of the orbital implants elevated the patient’s eye more than anticipated, however, producing hyperglobus and hypertropia. “We did a revision—a third surgery—to allow the eye to come down,” she said. “It’s important to note that strabismus surgery may be another necessary ophthalmological aspect.”
Quality of Life
“In contrast to solid organ transplants, which are lifesaving, this is the ultimate quality-of-life surgery,” said Dr. Bradley, alluding to both the transformative and challenging circumstances surrounding any face transplant. Three weeks after the first face transplant at Mayo Clinic, surgical team members surrounded the man who had tried to kill himself. Not yet able to talk, he scribbled on a notepad, “Far exceeded my expectations.”
___________________________
For more images from the Mayo Clinic case, see www.flickr.com/photos/mayoclinic/albums/72157678243262502.
___________________________
1 Khalifian S et al. Lancet. 2014;384:2153-2163.
2 Sosin M et al. PRS Journal. 2015;135(1):167e-175e.
___________________________
Dr. Bradley is a consultant in the department of ophthalmology and oculoplastic surgeon at the Mayo Clinic and associate professor of ophthalmology at the Mayo Clinic College of Medicine and Science in Rochester, Minn. Relevant financial disclosures: None.
Dr. Grant is professor of surgery at the University of Maryland School of Medicine and oculoplastic surgeon, plastic surgeon, and chief of the division of plastic and reconstructive surgery at the R. Adams Cowley Shock Trauma Center at the University of Maryland Medical Center in Baltimore. Relevant financial disclosures: None.
Dr. Mardini is a professor of surgery at the Mayo Clinic College of Medicine and Science; consultant in the division of plastic surgery and director of the face transplant program at Mayo Clinic; and surgical director of Mayo Clinic’s Essam and Dalal Obaid Center for Reconstructive Transplant Surgery in Rochester, Minn. Relevant financial disclosures: None.
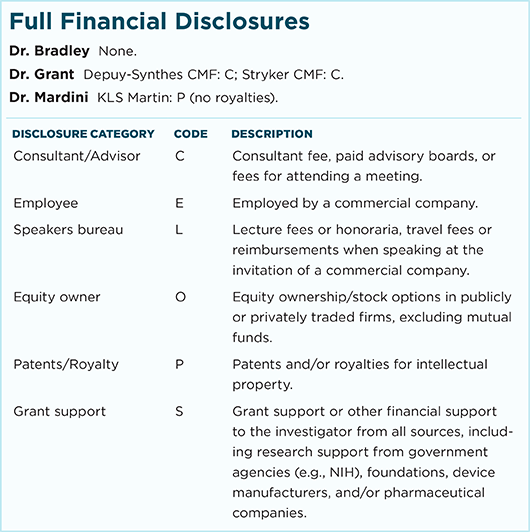
For full disclosures and the disclosure key, see below.