Download PDF
The myopia epidemic has become virtually impossible to ignore. In 2010, 28% of the world’s population was affected. By 2050, that number could reach 50%.1 The burden has been felt most strongly in East Asia, where rates can be as high as 90%, said Michael X. Repka, MD, at Johns Hopkins University in Baltimore. “In the United States, we’re nowhere near that level, but rates are higher than they were two generations ago.”
In the past, ophthalmologists have devoted more attention to other areas of their practice than to myopia prevention and progression, said Dr. Repka. “However, public awareness is growing, and we’re seeing much more interest in North America than we saw [even] five to six years ago.”
As evidence of this, Dr. Repka said, “clinical trials on myopia progression are now underway in the United States, Europe, and elsewhere.” And advocacy and education efforts are underway as well. “Given the magnitude of the condition and its impact on clinical care, education, research, advocacy, and the economy,” the Academy has identified myopia as a top strategic initiative, said Sarwat Salim, MD, at Tufts University in Boston (see “Joining Forces”).
Lifelong Impact
Despite this increase in awareness, some ophthalmologists may still be unaware of myopia’s full potential impact on patients’ lives, largely because the ramifications are not visible to them in the 10 to 20 years following diagnosis, said Aaron M. Miller, MD, with Houston Eye Associates.
“Up to 15% of myopic patients will become highly myopic and be at risk for disorders such as glaucoma, retinal detachment, and cataract,” said Nathan G. Congdon, MD, MPH, at Queen’s University Belfast in Northern Ireland.
A comprehensive strategy. Given this threat to eye health, researchers are now taking a broad approach. “First, we want to prevent the onset of myopia. Then, when a child becomes myopic, we want to prevent high myopia. And when a child becomes highly myopic, we want to prevent pathological myopia and all of its complications,” said Jason C.S. Yam, FCOphHK, FRCS, at the Chinese University of Hong Kong.
As for treatment, “Eye care providers need to know that there is now good evidence that we can ease myopia progression using more than one option,” said Donald Tan, MD, FRCS, FRCOphth, at the Singapore National Eye Centre. However, as Dr. Repka acknowledged, “To maximize results, we will almost certainly use those options in combination, but we don’t yet know if their effects will be additive.”
Behavioral Tx: Preventing Onset
In Hong Kong, children are at very high risk of myopia onset. By age 9, up to 44% have myopia—and up to 80% of adults eventually develop it, said said Prof. Yam. “This is why we really need to do something about myopia prevention, not just myopia control.”
Still an enigma. A mismatch between eyeball length and its optical power, myopia still remains a bit of an enigma. “We’re not much closer to understanding how the eye grows and the signals that prompt its growth,” said Dr. Tan, “but some of the risk factors for myopia onset are probably related to lack of time spent outdoors.”
Solution No. 1: Get outside. Although outdoor activities are protective against the onset of myopia, there are no studies to show they are protective against myopia progression, said Dr. Tan. It’s also not fully understood why time outdoors only prevents myopia onset and doesn’t retard its pace, Dr. Congdon said.
Trials in Taiwan and China have found that 40 to 80 minutes of extra outdoor time during the day reduced myopia incidence in schoolchildren by up to 50%. “A trial in China is now comparing one versus two hours, but there’s growing agreement that two hours each day is probably preferable,” said Dr. Congdon. In any event, “getting kids outdoors at a time when we have a global epidemic of obesity, diabetes, and diabetic retinopathy—and myopia—is a no-brainer. The potential to tackle these epidemics with the same intervention is especially powerful and appealing.”
Why does outdoor time help? Although it is likely related to scleral remodeling, the precise reason why outdoor time is effective in preventing myopia onset remains unproven, said Dr. Congdon.
Two potential explanations have gained prominence. One involves light, as recent studies suggest that differences in light intensity are a significant factor. Dr. Congdon was coauthor on one such study. “We were able to show that being outdoors at noon, when light is brighter, was more effective.” This provided another piece of evidence in favor of the light hypothesis, in addition to observed seasonal variation in myopia progression, he said.
The other hypothesis involves minimizing near focus, Dr. Congdon said. “When kids get outdoors, they have more opportunity to see the horizon and distance, not [just] accommodative targets.”
Solution No. 2: Bring light indoors. Dr. Congdon also coauthored a paper about a glass classroom, a Chinese pilot project that tested the acceptability of delivering high levels of light indoors, using glass that could filter out infrared light and prevent too much warmth. “The classroom design was preferred by teachers, students, and parents, so if China moves forward in building more of these classrooms, they will ‘push against an open door,’” he said.
Dr. Congdon added that there may be a variety of ways to add light to the classroom, such as skylights, proximity to windows, and the light boxes that are used to treat seasonal affective disorder.
Solution No. 3: Curtail near work. Excessive near work may increase axial length through biomechanical factors involved in downward gaze, such as ciliary muscle contraction.1 Although the influence of near work remains an unsettled question, Dr. Miller still encourages his patients to take breaks when they read or play computer games, for instance. He promotes the Academy’s 20-20-20 tip: That is, take a 20-second break to look 20 feet away for every 20 minutes of near work.
At this time, myopia experts feel that out-door activity is protective and may be more important than curtailing near work, said Dr. Tan. But there may simply be an interplay between near activity and lack of time outdoors. “That’s because children who are spending a lot of time doing near work and playing computer games are not outdoors.”
 |
|
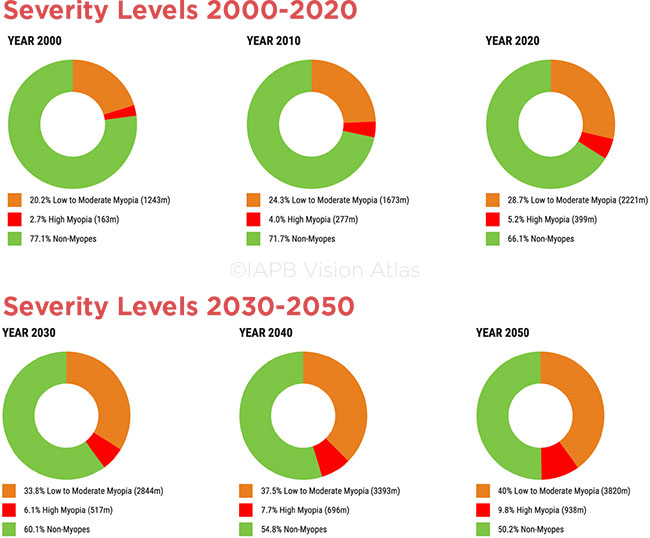
GROWING PANDEMIC. Statistics from the International Agency for the Prevention of Blindness outline the worldwide increase in myopia. (Red = high myopia.)
|
Drug Tx: Low-Dose Atropine
“Although several modalities are now available for slowing the progression of myopia, very good reviews and meta-analyses point toward atropine as having the strongest benefits,” said Dr. Tan.
Does it work? In 2017, the authors of an Academy Ophthalmic Technology Assessment (OTA) reviewed the published literature on the efficacy of topical atropine2 and concluded that Level I evidence supports its use for the prevention of myopic progression in children, said Dr. Salim. Now there’s further evidence that low-dose atropine is effective, at least in East Asian populations, said Dr. Repka. “Building on the ATOM study, coauthored by Dr. Tan, the LAMP study, coauthored by Prof. Yam, shows the ability to slow progression.” (See “Landmark Atropine Studies in East Asia.”)
Is it safe? Overall, the safety of low-dose atropine has been extremely good, said Dr. Tan, and the side effects are reversible. “Although the pupil may be slightly dilated and accommodation slightly reduced, these changes return to normal after cessation of atropine,” he said. “We’ve treated thousands of children for as long as five years with no cataract formation or retina changes during active trials, and there’s no evidence to suggest that there are long-term side effects.”
When providing parents with informed consent about atropine’s off-label use for myopia, Dr. Miller emphasizes that the concentration he uses in children with amblyopia is 30 to 100 times stronger than for myopia. “That’s why I feel more comfortable using low-concentration atropine,” he said.
Best protocol still unknown. We don’t yet have answers about the ideal candidates, concentrations, or formulations for atropine, said Dr. Repka. The optimal time to start and stop treatment to manage progression while minimizing side effects also remains unclear.
Evolving approach. Dr. Miller noted that his approach has changed over the years. “In the past, I’d want to see more than 1.5 D of myopia progression from one year to the next before starting treatment. As my comfort level with low-dose atropine has increased due to observing minimal side effects, my threshold has changed. Now I ask the parents about their final refraction. If both parents have moderate to high myopia, I might offer atropine to a child with .75 D progression in one year.”
Individualized dosing. Which concentration is best? Prof. Yam noted that his LAMP study identified 0.05% as most effective. “But we may titrate up or down, depending upon response,” he said. “We might choose a lower concentration for kids who are very responsive with no progression, and we might consider a higher dosage for nonresponders, such as the 15% of children who progress more than a diopter a year on 0.05% atropine.”
U.S. studies. Until recently, most atropine studies had been conducted in Asian countries where myopia prevalence is highest, said Prof. Yam, so it was important to replicate studies in other populations. Atropine trials in the prevention of myopia are now ongoing in children of European descent not only in the United States but also in Ireland, the United Kingdom, and Australia. “We may find factors related to ethnicity such as iris color and fundus pigmentation that impact its effectiveness,” said Dr. Miller. He added that he’s observed a little greater effect on near focus in some of his fair-complected patients.
Dr. Repka is a cochair of the Low-Dose Atropine for Treatment of Myopia (MTS1) Study,3 which is recruiting subjects between the ages of 5 and 13 to compare the efficacy of 0.01% atropine with placebo. It is one of a few atropine studies currently recruiting or underway in the United States. Published results likely won’t be available until the end of 2022, he said.
In the meantime, some U.S. ophthalmologists remain skeptical about the size of atropine’s effect, Dr. Repka said. “And lack of insurance [coverage] is a barrier. The cost here has tripled, largely due to greater compliance standards required at compounding pharmacies.” If it is approved by the FDA, Eyenovia’s microdosed atropine formulation (MicroPine), delivered using its patented piezo-print delivery technology, might solve the compounding conundrum, presuming that it is available at a reasonable price. Last June, the company launched a phase 3 study in the United States; the researchers will explore MicroPine’s safety and efficacy in more than 400 children between the ages of 3 and 12.4
More room to improve. Atropine’s cumulative public health benefit is very real, said Dr. Repka, and the effect on individuals is statistically significant. But there is still room for improvement. “With treatment, a child may be a –2 myope instead of a –3 myope, but he will still be wearing glasses all the time.”
Even though atropine is most effective at this point, other pathways also need exploring, said Dr. Tan. “We are at the cusp of having more pharmacological options. In initial studies, other antimuscarinic analogs may end up being even more effective than atropine. Early experiments also show that dopamine, which inhibits axial elongation in animal models and is released by light, might be a good candidate as well.”
 |
|
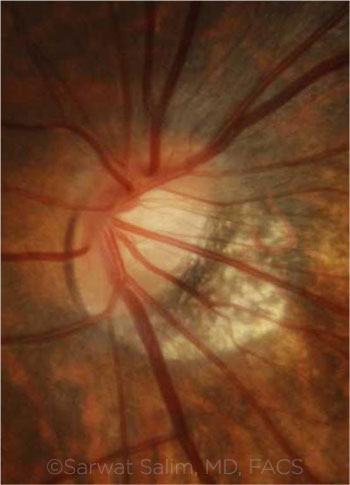
MYOPIC OPTIC NERVE. A tilted myopic disc with temporal rim thinning and large peripapillary atrophy. Several population-based studies have reported a 2- to 4-fold increased prevalence of glaucoma among patients with myopia, particularly those with moderate to high myopia.
|
Optical Tx: Ortho-K
Orthokeratology (Ortho-K) involves wearing gas-permeable contact lenses at night to reshape the cornea, causing central corneal flattening by compressing the corneal epithelium. In 2019, an Academy OTA assessed the role of Ortho-K to reduce myopic progression in children and adolescents compared with the use of spectacles or daytime contact lenses for standard refractive correction.5
The review concluded that Ortho-K may be effective in slowing myopic progression, especially when initiated between the ages of 6 and 8, said Dr. Salim. “However, several concerns have been raised with this intervention,” she said. These include the risk of corneal infection and cost, as well as insufficient data about the ideal duration of treatment and efficacy in non-Asians.
In addition, there is a lack of data about Ortho-K’s impact on refraction and its rebound effect, said Dr. Tan. “The rebound phenomenon has been observed in some Ortho-K studies.”
Does it work? Ortho-K is second to atropine in terms of efficacy, Dr. Tan said. Although it was approved by the FDA for the daily management of myopia, it has never been approved for slowing the rate of myopia progression. Some studies evaluating its impact on progression are being completed; others are underway, Dr. Repka noted.
Is it safe? “The elephant in the room will always be the potential for sight-threatening complications,” said Dr. Tan, such as microbial keratitis and corneal scarring. “Proponents of Ortho-K will say the risk of infection in children is about the same as it is for adults wearing conventional soft contact lenses overnight. But we don’t recommend overnight wear in adults because of the risk of infection. We shouldn’t ignore the risk in children.”
These risks lead many ophthalmologists to be negative about Ortho-K, said Dr. Miller. “But we could be a little biased. As ophthalmologists, we always see the disasters and may not see the hundreds of other kids that do well with Ortho-K.”
Patient selection is key. Clinicians who choose Ortho-K must identify the right patients, said Dr. Miller. Ortho-K “takes a lot of work and is not easily sustainable.” Dr. Tan agreed. “In general, older children may have better contact lens habits—cleaning lenses and hands, avoiding overwear, and changing lens cases regularly. These all help decrease the risk of infection.”
With regard to infection risk, Prof. Yam noted that he always advises parents, “If your child has any discomfort, redness, or pain, stop and see the eye doctor without delay.”
What about other optical approaches? In addition to orthokeratology, executive bifocal spectacles and peripheral plus contact lenses appear to be most helpful in reducing the rate of myopia progression.1 Optical approaches may work in a variety of ways, such as by reducing accommodative lag or through myopic defocus.1
Novel designs of soft contact daily wear lenses are based on an optical defocus principle, said Dr. Tan. Trials are in progress—and, in November, the FDA approved the MiSight contact lens (Cooper-Vision) for children who are 8 to 12 years old. Prof. Yam is most excited about defocus spectacles, partly because they are less invasive than their contact lens counterparts. “However, we need more data to support their efficacy, whether used alone or in combination with atropine,” he said.
“My main concern is what to do in low-resource areas,” said Dr. Congdon. “If these spectacles and contact lenses come down in price, they could be of great interest.”
 |
|
RETINAL DETACHMENT. RD in a 27-year-old woman with myopia. Note demarcation line and subretinal gliosis in superotemporal quadrant—and spontaneous reattachment in inferotemporal quadrant. This image was originally published in the ASRS Retina Image Bank. Kamal Kishore, MD, MBBS, and Stephanie Shaver. Chronic Retinal Detachment in a Young Myopic Patient. Retina Image Bank. 2019; Image Number 40413. © The American Society of Retina Specialists.
|
Joining Forces
Although interest in myopia progression is picking up, additional research is needed. To make this happen, Dr. Tan said, greater action by professional societies, the ophthalmic community, and governments is needed.
Efforts underway include the following:
Academy task force. In 2019, Dr. Salim joined a group of international experts to convene a Myopia Task Force, spearheaded by the Academy under the leadership of Richard L. Abbott, MD, who is at the University of California, San Francisco, and Dr. Tan. Its main purpose is to develop an evidence-based white paper to provide a rationale for prevention and early intervention, review available approaches to control myopia progression, and outline next steps to ameliorate this public health challenge.
Government initiatives. In 2010, Taiwan launched a national myopia prevention program, called Daily 120, to promote at least two hours of outdoor activity each day.6 “That program is beginning to publish data showing that it has been very effective in reducing myopia rates,” said Dr. Congdon.
In August of 2018, President Xi Jinping announced a national myopia program7 in China, a country with half the kids in the world who are visually impaired by uncorrected myopia, said Dr. Congdon. “Led by the Ministry of Education and involving six different federal agencies, that national project has set specific targets and created accountability for reducing the prevalence of myopia.”
The program employs a broad-based approach, said Prof. Yam, including time outdoors as well as a reduction in the reading burden on very young kids, such as less homework time for kindergarteners. “I think that level of national attention is quite crucial,” he said, adding that he hopes Hong Kong initiates something similar.
Call for Collaboration
Within ophthalmology, Dr. Miller believes myopia management will see greater involvement by pediatric ophthalmologists. Moreover, he added, “There will be too many patients to be entirely managed by either optometry or ophthalmology, so we’ll need greater collaboration.” He noted that he is already getting referrals from optometrists and other physicians outside of ophthalmology.
Finally, he noted, “We can also partner with other medical groups such as family practice and pediatrics to encourage healthier lifestyles, including more time outdoors.”
___________________________
1 World Health Organization. The High Impact of Myopia and High Myopia. WHO; 2017. Accessed Nov. 14, 2019.
2 Pineles SL et al. Ophthalmology. 2017;124(12):1857-1866.
3 www.clinicaltrials.gov. NCT03334253: Low-Dose Atropine for Treatment of Myopia (MTS1). Accessed Nov. 14, 2019.
4 www.clinicaltrials.gov. NCT03942419: Microdosed Atropine 0.1% and 0.01% Ophthalmic Solutions for Reduction of Pediatric Myopia Progression. Accessed Nov. 14, 2019.
5 Vanderveen DK et al. Ophthalmology. 2019;126(4):623-636.
6 Wu PC et al. Ann Eye Sci. 2018;3(2):12.
7 Jan CL, Congdon N. Lancet Child Adolesc Health. 2018;2(12):845-846.
Landmark Atropine Trials in East Asia
It’s difficult to directly compare the two landmark atropine randomized controlled trials that have been conducted in East Asia, said Prof. Yam. That’s because the eyedrop formulations, study cohort, and study design differed between the studies. Different formulations may partly explain why ATOM’s 0.01% concentration appeared to have twice the effect of LAMP’s 0.01% concentration, said Dr. Tan.
ATOM 1 and 2. “Our group was the first to look at 0.01% concentration of atropine,” Dr. Tan said. ATOM 1 established the clinical efficacy of atropine 1% in the short term, but it concluded that this dose caused visual side effects from cycloplegia and mydriasis. ATOM 2 had two phases, but it concluded that 0.01% eyedrops were more effective in slowing progression over five years than higher doses of 0.1% and 0.5%—and with fewer visual side effects.1
In addition, ATOM 1 and 2 revealed a rebound effect upon cessation of atropine treatment. Both refractive error and axial elongation tended to increase upon cessation of treatment, but this phenomenon mainly occurred with the higher concentrations, said Dr. Tan. There did not appear to be any significant rebound effect when treatment with 0.01% atropine was stopped.
LAMP. “Our study2 was the first randomized controlled trial to make a direct comparison between a placebo group and low-concentration groups of 0.05%, 0.025%, and 0.01%,” said Prof. Yam. “Compared to placebo, we found that all three groups of low-concentration atropine were effective in preventing myopic progression,” he said, “but there was a concentration-dependent response,” with 0.05% proving to be most effective in slowing progression in year 1, he said. “We also found a significant concentration-dependent response in axial length.” The second-year results, which were presented at the 2019 meeting of ARVO, were similar.
Although side effects were also concentration dependent, they were not clinically significant, said Prof. Yam. “For example, pupil dilation increased by 1 mm for the 0.05% concentration compared to placebo, but this was not enough to cause problems such as glare.”
The LAMP phase 3 study will address the rebound phenomenon with the 0.05%, 0.025%, and 0.01% doses, said Prof. Yam. In addition, it will assess whether treatment should be stopped after two years of usage.
ATOM 3. The conventional approach has been to start atropine when a child has become myopic and is starting to progress, said Dr. Tan. “But new studies have shown that the earlier the age of onset, the higher the myopia will eventually become.” Dr. Tan is leading a new study, ATOM 3, which is examining whether it is possible to prevent the onset of myopia by starting treatment earlier, just before myopia actually occurs in premyopic children, or at least delay the disease in the hopes of preventing high myopia.
___________________________
1 Chia A et al. Ophthalmology. 2016;123(2):391-399.
2 Yam JC. Ophthalmology. 2019;126(1):113-124.
|
Meet the Experts
Nathan G. Congdon, MD, MPH Chair of Global Eye Health at Queen’s University Belfast in Northern Ireland. He is also professor of preventive ophthalmology at the Zhongshan Ophthalmic Center, Sun Yat-sen University, in Guangzhou, China. Relevant financial disclosures: None.
Aaron M. Miller, MD, MBA, FAAP Pediatric ophthalmologist at Houston Eye Associates in The Woodlands and Tomball, Texas, and adjunct assistant professor of ophthalmology at Houston Methodist Hospital’s Blanton Eye Institute. He is also president of the American Orthoptic Council. Relevant financial disclosures: None.
Michael X. Repka, MD, MBA Professor of ophthalmology and chief of Pediatric Ophthalmology and Adult Strabismus at Johns Hopkins University and vice chair for clinical practice at the Wilmer Eye Institute in Baltimore. Relevant financial disclosures: None.
Sarwat Salim, MD, FACS Professor of ophthalmology, vice chair of clinical and academic affairs, and director of the Glaucoma Service at Tufts University in Boston. Relevant financial disclosures: None.
Donald Tan, MD, FRCS, FRCOphth Adjunct professor of ophthalmology and visual sciences at the Duke–National University of Singapore Medical School, senior scientific advisor at the Singapore Eye Research Institute, and visiting senior consultant at the Singapore National Eye Centre. He is also partner and senior consultant ophthalmic surgeon at Eye & Retina Surgeons, Camden Medical Centre, Singapore. Relevant financial disclosures: None.
Jason C.S. Yam, FHKAM, FCOphHK, MBBS, MPH, FRCS Associate professor of ophthalmology and visual sciences at The Chinese University of Hong Kong. Relevant financial disclosures: None.
Full Financial Disclosures
Dr. Congdon Ulverscroft Foundation: S.
Dr. Miller NEI: S.
Dr. Repka AAO: S; NEI: S.
Dr. Salim Aerie Pharmaceutical: C,L.
Dr. Tan Eye Lens: C; Network Medical: P; Santen: C,L,S.
Prof. Yam None.
Disclosure Category
|
Code
|
Description
|
| Consultant/Advisor |
C |
Consultant fee, paid advisory boards, or fees for attending a meeting. |
| Employee |
E |
Employed by a commercial company. |
| Speakers bureau |
L |
Lecture fees or honoraria, travel fees or reimbursements when speaking at the invitation of a commercial company. |
| Equity owner |
O |
Equity ownership/stock options in publicly or privately traded firms, excluding mutual funds. |
| Patents/Royalty |
P |
Patents and/or royalties for intellectual property. |
| Grant support |
S |
Grant support or other financial support to the investigator from all sources, including research support from government agencies (e.g., NIH), foundations, device manufacturers, and/or pharmaceutical companies. |
|