Download PDF
In a move that could ease the burden on physicians who are seeking a compassionate use exemption for their patients, the FDA is in the process of streamlining the entire application process.1 As researchers and clinicians know all too well, the traditional process of bringing new drugs or medical devices to market is a long one. It often takes “years to move drugs and devices from the bench to the bedside,” said Andrew G. Lee, MD, at the Blanton Eye Institute in Houston. And physicians who want to accelerate the process and obtain a drug or device for an individual patient dread jumping through the necessary hoops.
Reducing the Burden
The FDA’s change can’t come soon enough for many physicians, as the process of completing the necessary forms has been a time-consuming one. For instance, the Office of Management and Budget (OMB) estimated that it took physicians from 8 to 16 hours to fill out and submit each Individual Patient Expanded Access form.1
And that’s only the beginning. For instance, if a cataract surgeon wants to procure a specialized lens for a patient but cannot buy that lens because it’s not FDA approved, the surgeon must follow a cumbersome 3-part course of action: 1) petition the FDA for permission to import the lens for the patient, 2) monitor the patient’s use of the lens, and 3) report back to the FDA.
Kevin M. Miller, MD, who has followed this route numerous times, expressed the frustration that so many of his colleagues feel. “Only a few of us have been able to crack the FDA’s code on this process, and it can be difficult to determine what that code is,” said Dr. Miller, at the Stein Eye Institute in Los Angeles. “The result is that some patients may need to wear a contact lens after cataract surgery because of their high degree of astigmatism. It’s not the end of the world for the patient, but it may not be the best treatment they could have achieved.”
New form = less time? The revised application form (Form FDA 3926, still in draft stage) is a 2-page document2 and the OMB has estimated that it will take a physician 45 minutes to fill it out.1 A supportive statement from a second physician is no longer required, but a letter of authorization (LOA) from the manufacturer may be needed in some circumstances.
Embrace the CUDE
It’s essential to note that filling out the submission form is only the beginning—the physician must still obtain institutional review board (IRB) approval and develop a plan for monitoring procedures.
But Samuel Masket, MD, at the Stein Eye Institute and in private practice in Los Angeles, said he believes that it’s important for all ophthalmologists to have at least a working understanding of the compassionate use device exemption (CUDE) process and learn how to navigate through the system. “For the very unusual situation, in which a CUDE would definitely benefit a patient, the ophthalmologist should know how to use the process and how to petition the FDA for a device for the patient. Obviously, the process is somewhat painstaking, but it’s very rewarding at the end of the day—for the patient and, therefore, for the physician as well.”
Dr. Masket said, “What one really needs to do in this process is to make a case for why that device is the best way to manage that particular patient and confirm that other alternatives have been tried or considered and were found to be ineffective.” He added, “If you provide a careful explanation of why that product is necessary for that particular patient, the chances of achieving a CUDE approval are very high.”
Multiple Pressures
Pressure to change the way the FDA does business is coming from several fronts:
Ebola. The recent Ebola virus pandemic provided a stunning example of the absolute need for speed when lives are at stake. “Ebola is the perfect example of how we didn’t have a multiyear time frame to wait for a vaccine, and we had to move quickly to human trials, especially when people were dying,” Dr. Lee said. “Testing and developing an Ebola vaccine would not have been feasible in the FDA’s traditional multiphase process.”
Right-to-try legislation. These controversial laws permit drug companies to provide experimental medications to terminally ill patients without FDA approval.1 More than 15 states have already passed right-to-try laws, and nearly 20 have the legislation on their dockets.2
International competition. Finally, there’s the pressure presented by global competition, as companies in other countries can bring new drugs and devices to market much more quickly than U.S. companies can.
___________________________
1 Darrow JJ et al. N Engl J Med. 2015;372(3):279-286.
2 www.raps.org/Regulatory-Focus/News/Right-to-Try/.
|
What to Expect
Although it’s impossible to foresee every potential scenario, here are some examples of what clinicians can expect during this time of transition.
No: Artificial iris. In the past, the CUDE process was used for artificial iris implants, Dr. Masket noted. However, now that there is an FDA trial with the HumanOptics custom iris implant, the CUDE strategy cannot be used for any artificial iris device.
Yes: Unusual IOLs. However, “one can use the CUDE process for unusual intraocular lenses [IOLs],” Dr. Masket said. “The highest-power IOL manufactured in the United States is a plus-40 D lens, but in very rare situations some eyes can require 60 D or greater. And it isn’t always a good idea to piggyback lenses in the same eye based on space, size, and other criteria.”
It’s complicated: Drugs and biologics. Nancy M. Holekamp, MD, said the FDA approval process for drugs and biologics is still long and difficult, and cutting-edge products that make it to the market are often prohibitively expensive for patients.
For instance, aflibercept (Eylea) should be used only on label to receive insurance reimbursement. Off-label use is financially out of reach for many patients, said Dr. Holekamp, at Washington University School of Medicine and Pepose Vision Institute in St. Louis, Mo. “We can’t expect insurance companies to pay for off-label use, and yet we have patients with very similar conditions who could benefit greatly from these drugs. In fact, we have orphan diseases or less-common indications in which we have found biologic plausibility that the injections do work in these conditions, and yet we are unable to give them.”
Fortunately, “patients with unmet medical needs do have options, and there are ways to get a request expedited,” Dr. Holekamp said.
Final Thoughts
“The FDA’s expedited processes are expected to bring innovation to people more quickly—at least, that’s the goal,” Dr. Lee said. At his institution, the early signs are promising, he said. But as he pointed out, safety will always be the preeminent driver of any decision-making regarding streamlining approvals for drugs and devices, because it only takes 1 headline in The New York Times to short-circuit the entire process.
For now, Dr. Lee encourages ophthalmologists to speak up on this subject. “We are future patients as well as doctors—and we are also voters—and we should encourage patients who have orphan or rare diseases that would benefit from compassionate use drugs or devices to speak with their members of Congress.” He added, “We obviously are not doing this type of advocacy work for ourselves or for the money. We are pushing the boundaries for investigational devices because we want to advance the knowledge base and help patients.”
___________________________
1 Kux L. Federal Register. 2015;80(27):7318-7321.
2 Individual Patient Expanded Access Applications: Form FDA 3926.
___________________________
Dr. Holekamp is professor of clinical ophthalmology at Washington University School of Medicine and in private practice at Pepose Vision Institute in St. Louis, Mo. Relevant financial disclosures: Regeneron: C,L.
Dr. Lee is chairman of ophthalmology at the Blanton Eye Institute, Houston Methodist Hospital. Relevant financial disclosures: None.
Dr. Masket is clinical professor of ophthalmology at the Stein Eye Institute and in private practice at Advanced Vision Care in Los Angeles. Relevant financial disclosures: None.
Dr. Miller is Kolokotrones Chair in Ophthalmology at the Stein Eye Institute in Los Angeles. Relevant financial disclosures: None.
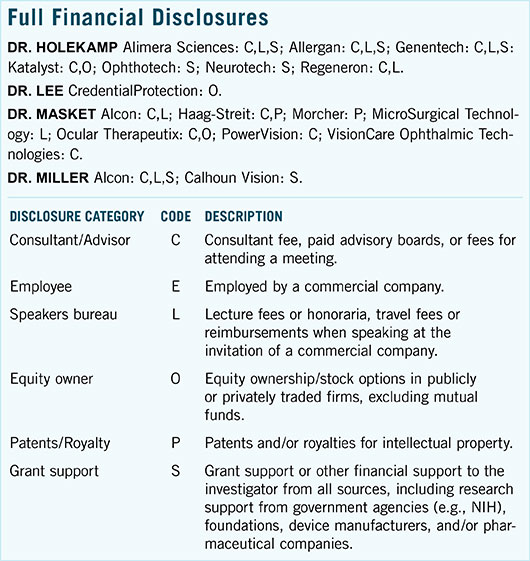
For full disclosures and the disclosure key, see below.