Download PDF
Make your diagnosis in the comments, and look for the answer in next month’s Blink.
Last Month’s Blink
PFO After Vitreoretinal Surgery
Written by Tarek Alasil, MD, and Omar Shakir, MD, MBA, both at the Department of Ophthalmology and Visual Sciences, Yale University, New Haven, Conn., and West Haven Veterans Affairs Eye Clinic, West Haven, Conn.; and Patrick A Coady, MD, MBA, at West Haven Veterans Affairs Eye Clinic and New England Retina Associates, Hamden, Conn. Photo by Patrick A. Coady, MD, MBA.
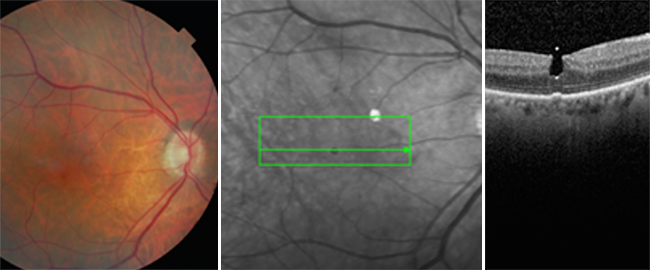
A 76-year-old man with a macula-on rhegmatogenous retinal detachment in his pseudophakic right eye underwent pars plana vitrectomy with perfluoropropane gas tamponade. Six weeks after surgery, his vision was 20/25 (back to baseline), the retina was attached, and the patient had no visual complaints. Spectral-domain optical coherence tomography (SD-OCT) imaging of the right macula demonstrated a hyporeflective (due to the scattering of light) oval-shaped vertically stretched area within the center of the fovea, with hyperreflective dots on the top and bottom tips of the oval area where light comes directly back to the OCT light detector. No retina material was detected overlying this bubble. This was consistent with retained preretinal perfluoro-n-octane (PFO) within the center of the foveal depression.
In addition, the OCT image of the retinal and choroidal material underneath the PFO bubble seems to be shifted upward, appearing closer to the light detector. This phenomenon is explained by light traveling more quickly through the PFO bubble compared to the surrounding aqueous. This happens because of the lower index of refraction of PFO (1.27) compared to that of humor/vitreous humor (1.336).
The PFO bubble appears to be vertically elongated in the portion within the retina, which is explained by the substance of the retina exerting a more horizontal compressive force compared to vertical. In the aqueous portion, the bubble takes a more rounded appearance, given the more even distribution of surface tension on this portion. The patient remained macula-on during the case, and given that the outer retina looks intact on OCT, it is unlikely that this bubble came from a subretinal location. It is possible that this preretinal PFO bubble got lodged into the foveal depression during a relatively high-pressure injection of PFO directed at the macula during the case.
Even though the bubble has no visible retinal roof (thin slice vertical and horizontal line scans show no overlying inner limiting membrane or epiretinal membrane material), it remains lodged within the central foveal depression at 12 weeks postoperatively. The patient remained asymptomatic, with no deficit on Amsler grid, and no change in refractive error or visual acuity at 7 months postoperatively.
Read your colleagues’ discussion.
| BLINK SUBMISSIONS: Send us your ophthalmic image and its explanation in 150-250 words. E-mail to eyenet@aao.org, fax to 415-561-8575, or mail to EyeNet Magazine, 655 Beach Street, San Francisco, CA 94109. Please note that EyeNet reserves the right to edit Blink submissions. |