Download PDF
With surgical and facility fees falling, it might look like financial suicide to buy and use a femtosecond laser for cataract surgery. But early adopters are striving to develop financial models that they believe will pave the way toward widespread use of this high-tech device within a few years.
Perplexity is the predominant reaction when ophthalmologists try to imagine a future in which the femtosecond laser is being widely used as a safe, cost-effective, and essential tool of cataract surgery.
Skeptics and proponents alike ask one overarching question: Is there an economic model for incorporating femtosecond laser into cataract surgery? Currently, the answer remains no. But the first amorphous outlines of organizational paradigms that could support wider adoption of laser cataract surgery are beginning to emerge. Unfortunately, most of them depend on the physician, governmental agencies, and/or the patient to pitch in financial resources to the complex and already costly tangle that is the American medical care system.
But, if the economics are precarious, why is there so much enthusiasm about the possible advantages of femtosecond lasers in cataract surgery?
William W. Culbertson, MD, director of cornea service and the refractive surgery center at Bascom Palmer Eye Institute, recalled the words of Juan Batlle, MD, an investigator in the Dominican Republic trials of the Catalys femtosecond laser (OptiMedica). Said Dr. Batlle: “It makes routine cataract surgery easier, it makes difficult cataract surgery routine, and it makes otherwise impossible cataract surgery possible.”
Other leading ophthalmologists contacted by EyeNet said they are intrigued by the laser’s potential as a tool for cataract surgery. But they pointed to obstacles posed by the complicated economics of using any of the four lasers available for performing capsulorrhexis or lens fragmentation in the United States. They also lamented the lack of well-designed, independent research studies comparing outcomes between laser-based surgery and conventional phacoemulsification.
“There’s pressure to purchase a femto laser—even though the business model doesn’t make sense because the laser is expensive, slow, and not clearly more safe. It seems like one of the best reasons now to get a laser is to ‘keep up with the Joneses’ rather than for any outcome or safety issue,” said Thomas A. Oetting, MD, associate professor of clinical ophthalmology at the University of Iowa. “From a business point of view, the laser seems like a high-overhead way of treating astigmatism compared with the use of toric IOLs [intraocular lenses] or limbal relaxing incisions with a blade, and it doesn’t seem to add any value to the patient or surgeon.”
Four Early Economic Models
Amid much uncertainty, laser cataract surgery in the united states appears to fit—so far—into four evolving and fluid models.
#1 Medicare-based practices and surgery centers: Limbal relaxing incisions and specialized IOLs with advanced imaging cost extra
This model could support the higher costs of femtosecond laser–assisted cataract surgery only in ophthalmic practices and surgery centers with patients who are able and willing to pay for refractive “extras” that Medicare does not cover, Dr. Oetting said.
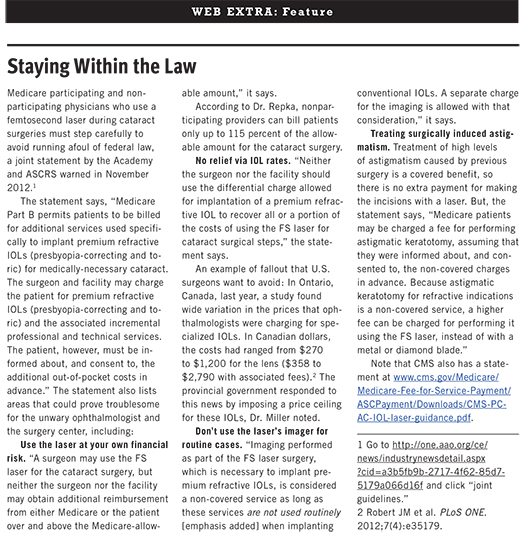
The only laser-related service for which a cataract patient can be charged extra in 2013 is the use of the laser’s built-in imaging system to optimize placement of specialized (presbyopia-correcting or toric) IOLs or limbal relaxing incisions (LRI). “The imaging for femtosecond laser is considered supplemental and a separately billable service when performed with premium lens implants,” said Michael X. Repka, MD, MBA, the Academy medical director for Governmental Affairs.
“In our practice, few patients opt for toric IOLs, so it seems unlikely that we would be able to generate enough revenue to pay for the fixed cost of the laser. I suppose as the fixed cost comes down it might make more sense, but only if it is safer and more predictable,” Dr. Oetting said.
But at Island Eye Surgicenter in Carle Place, N.Y., a gamble taken two years ago has begun to pay off. The center’s LenSx femtosecond laser (Alcon) no longer operates in the red, said Russell G. Fumuso, MD, a partner in the center. He also is a partner in Ophthalmic Consultants of Long Island, a group of 24 subspecialists who operate at the Long Island surgery center.
The center needs 363 femtosecond laser cases per year to cover the femtosecond laser’s annualized costs, Dr. Fumuso said. There were 220 cataract surgeries using the laser in 2011, when it was available for only seven months, and 515 cases in 2012, he said. “We’re actually making some money on it now. At first, we weren’t breaking even.”
(click to expand)
#2 Medicare opt out, with patients paying cash
By opting out of participation in Medicare, these practices say good-bye to all but the most well-heeled cataract surgery patients, who contract to pay the full cost of their planned surgeries (including specialized IOLs and LRIs) in advance. This model largely frees the practices from federal scrutiny.
Financial suicide? Not overseas. Although opting out of Medicare might seem like a step toward financial suicide, there are hints at the international level that the all-cash model can succeed because some consumers react enthusiastically to “bladeless” cataract surgery.
In Germany, where patients pay 100 percent of the costs of femtosecond cataract surgery, a clinic in Bochum acquired a femtosecond laser in December 2011 with the expectation that it would pay for itself in two years at the earliest; it took only six months—without any advertising.
And in Australia, where patients share the cost with public and private payers, patients in Sydney routinely agree to pay the extra cost of having a femtosecond laser used in their cataract surgeries, according to a member of a group of ophthalmic surgeons who reported outcomes in 1,500 patients this year.1
#3 University-based practice, supported by philanthropy and teaching funds
This model is how ophthalmologists at the University of Miami and Northwestern University, in Chicago, acquired their femtosecond lasers. But cataract surgeons at UCLA’s Jules Stein Eye Institute haven’t been as lucky.
At Bascom Palmer, Dr. Culbertson said he found a donor who paid 100 percent of the cost in return for having the refractive surgery center named in the contributor’s honor.
At Northwestern Memorial Hospital in Chicago, a significant portion of the laser’s cost was supported by a donor whose vision was to facilitate the modern evolution of cataract surgery technology at Northwestern. The hospital provided the remainder after a compelling case was made by faculty member Surendra Basti, MD. Dr. Basti helped convince administrators that the laser was vital to staying on the cutting edge in ophthalmic surgery, said Nicholas J. Volpe, MD, chairman of ophthalmology at Northwestern. “We wanted to really get ahead of the curve in this field within the Chicago area,” Dr. Volpe said.
But in Southern California, the downside of relying on philanthropy to fund a big-ticket item became evident during the last two years. Kevin M. Miller, MD, professor of clinical ophthalmology at UCLA, said that he has asked three potential donors for money to buy a femtosecond laser, and he was turned down all three times. This is despite the fact that about 35 percent of his cataract patients pay to have a toric or multifocal IOL, making them candidates to pay also for services related to femtosecond laser.
#4 Veterans Affairs (VA) and other federally subsidized facilities
Backed by their ongoing institutional funding, VA medical centers around the nation are beginning to acquire femtosecond lasers and to use them, without being hindered by reimbursement worries or Medicare-imposed limits on pricing and allowed uses, said Dr. Oetting, who divides his time between the university and the VA hospital in Iowa City.
The Challenges of Introducing Lasers Into Cataract Surgery
Costs of the laser
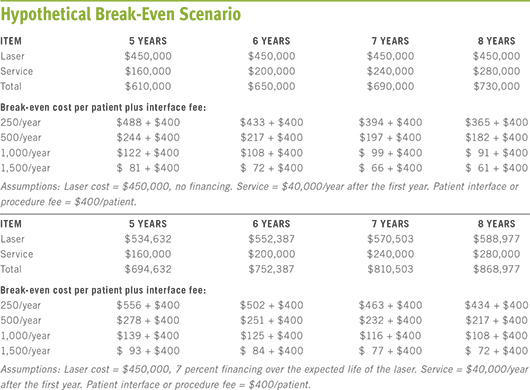
Before buying a laser, a practice may have difficulty estimating how many patients will choose a femtosecond laser procedure over conventional cataract surgery and determining whether that number will be sufficient to cover the costs of buying and using the laser, Dr. Miller said. His ballpark numbers on this topic, presented in 2011 to the International Conference on Femtosecond Lasers in Ophthalmology, in Dana Point, Calif., are still widely quoted. (See “Hypothetical Break-Even Scenario.”)
“You’re kind of throwing darts in the dark, at a dartboard you can’t see—hoping that you’re hitting your target, but you won’t know until the end of the year,” Dr. Miller said.
Of the break-even laser plans, Dr. Oetting said, “They do not seem like a fair comparison to me. Sure, in several years you may be able to pay off the laser, maybe even before it becomes obsolete. But the comparison should be between astigmatic correction with toric/LRI versus the femto laser. In the same time that you used the astigmatic fee to pay off the laser you could have charged less or put it in the bank. The question is: Which procedure is better for the patient? That is not clear.”
Acquisition and user fees. Dr. Culbertson, who oversaw the clinical trials that led to FDA approval of the OptiMedica laser for cataract procedures, said the purchase cost for the lasers available in the United States ranges from $350,000 to $500,000, and per-use fees (aka “click fees”) generally range from $175 to $400.
“There are all kinds of payment plans. You can lease the laser, lease to buy, or buy it, and some [femtosecond] companies give away the laser for a nominal sum and then charge a higher click fee. If you’re leasing the equipment and just paying per click, the fee could be $650 to $750 per treatment," he said.
Nonlaser operational costs. Ancillary costs of having a femtosecond laser must also be considered, said Jonathan M. Davidorf, MD, a West Hills, Calif., refractive and cataract surgeon who describes himself as having “an exceedingly high level of skepticism” about claims that the laser improves the refractive accuracy of cataract surgery. The decision about buying a laser should include not just the costs of buying and maintaining it but also the indirect operating costs, Dr. Davidorf said. He listed some of these: “The space the laser takes up; the cost of OR time; staffing costs not just in the OR, but also for the receptionists, preop nurses, recovery room nurses, and ancillary staff, all of whom will be at the surgery center longer because of increased surgical time; the cost of doctor’s time; and the opportunity costs. That is, revenue the doctor could be earning by performing another economically productive task.”
More capital spending? At Island Eye Surgicenter, one of the three surgery suites has been equipped with a LenSx femtosecond laser for two years, Dr. Fumuso said. The laser adds five to six minutes to cataract cases, and the center learned to minimize the impact by scheduling femtosecond laser cases toward the end of the day, he said. But administrators are considering adding more operating rooms to ease scheduling conflicts as the number of laser cases increases. “We have the femtosecond laser in one operating room, so all of those procedures have to be done in there. We might get three full cases an hour in that room,” he said.
Farewell to phaco? Although evidence for the demise of the phaco machine remains anecdotal or inferred, some surgeons foresee that one day the femtosecond laser can replace phaco machines entirely in the United States and other developed countries. “It looks like with the OptiMedica laser that we’re getting close to eliminating use of the phacoemulsification machine, and then we will have reduced one of the costs of cataract surgery,” Dr. Culbertson said.
In academia, the mission vs. the budget
Ophthalmic teaching hospitals must have access to new surgical technologies because of their role in training the ophthalmologists of tomorrow, according to Dr. Culbertson. “With resident and fellow training, you can’t just be stuck on yesterday’s technologies. You have to train your trainees,” he said.
Yet academic centers also are low-volume cataract centers to which difficult cases are referred and where federal limits on cataract reimbursement can take a special and unavoidable toll on the institution’s budget. “There’s usually not a volume sufficient to justify a large capital expense like a femtosecond laser,” Dr. Culbertson said. Nor can use of the laser for the basic steps in cataract removal be billed to anyone. “But here’s the catch-22: These lasers are probably very helpful in very difficult cases. So the institution just absorbs the extra expense,” he said.
Dr. Volpe said that Northwestern hospital administrators aren’t expecting to be repaid for their contribution toward buying a femtosecond laser for cataract surgeries last fall. “They’ll be happy to cover just the day-to-day costs,” he said.
He noted, however, that the hospital “open staff” policy could help recoup costs by increasing the number of potential laser users. Under the policy, community ophthalmologists are encouraged to consider an appointment to the clinical faculty and use of the hospital’s facilities.
Being ethical, avoiding liability traps
In addition to heeding Medicare’s billing rules (see “Staying Within the Law”), surgeons should assure that the patient is fully informed about their cataract surgery options, Dr. Repka said.
This means never overstating the merits of femtosecond laser surgeries and always maintaining transparency in pricing, he said. This communication with patients not only is an ethical imperative but it also helps safeguard the surgeon and practice against the financial impact of lawsuits based on what the patient was told to expect.
(click to expand)
What Does the Evidence Say About Safety and Outcomes?
From enthusiasm to dogma. When the earliest clinical research report about femtosecond laser–assisted cataract surgery was published more than three years ago,2 optimistic predictions about the technology sometimes morphed into oft-repeated, but generally unsupported, claims of superiority for the laser compared with phaco.
For instance, although laser-made capsulorrhexes in some studies have had more reproducible shapes and dimensions than the manual version,3-6 proof that this improves the refractive predictability of outcomes is lacking, according to Dr. Miller. “Claims about the rhexis are premature,” he said.
Dr. Davidorf agreed. He reported at the 2012 Academy Annual Meeting on a study he conducted comparing his better manual capsulotomies with his poorer ones, and he found no statistically significant refractive differences in outcomes.
Less phaco energy during nuclear disassembly. Some researchers have reported that laser prefragmentation of the lens lowered the amount of phacoemulsification energy required to remove the lens.1,7-9 Presumably, this would reduce the risk of damage to the corneal endothelium. However, it is unclear how large this purported benefit would need to be in order to justify the added costs to society of femtosecond laser cataract surgery—especially as the number of elderly Americans balloons during the next two decades.
Complications and the surgical learning curve. Dr. Basti, who has been working with an OptiMedica laser at Northwestern since last fall, said that he found the learning curve less daunting for laser-assisted cataract surgery than it was for phaco.
But Dr. Oetting contends that the femtosecond laser is being welcomed into the cataract surgery suite without sufficient scrutiny of its safety claims. “The driving force for the laser should be safety or better outcomes, not the ability to bill extra or market more effectively. What seems odd to me is how many devices have been sold without unbiased evidence of increased safety. The learning curve studies coming out now are a bit unsettling, too,” he said.
For instance, an Australian group reported last year that there was an “unacceptably high” number of complications in their initial femtosecond laser cataract cases. There were eight anterior radial capsular tears and seven posterior capsular tears, with vitreous loss, in 200 cases, compared with a total of 11 capsular tears (eight anterior) in 1,000 phaco-only cases by the same surgeons just before the laser arrived (p < 0.001).10
A follow-up study published this year1 confirmed the surgeons’ initial impression that the excess of complications fell sharply as the surgeon gained experience.
Likewise, concern about high intraocular pressure (IOP) from applanation of the cornea arose during early clinical trials, but modifications to the lasers have reduced concern over this issue, Dr. Basti said.
Wanted: prospective, industry-independent studies. Dr. Oetting said he hopes that having the laser in the VA medical system will result in well-designed and unbiased studies to evaluate laser cataract surgery. Several academic medical centers also have talked about conducting multicenter prospective clinical trials that would be randomized, controlled, and free of commercial bias, Drs. Miller and Volpe said.
“I think it is important for academic medical centers to have femtosecond lasers,” Dr. Basti said. “Pertinent questions need to be answered scientifically, and academic institutions should be part of it. Our firsthand experience with these lasers will help provide an unbiased view of the technology.”
Predictions: The Future of Femtosecond Procedures
Despite the many questions that remain, these cataract surgeons said they expect femtosecond lasers to become a commonly used cataract surgical tool, probably within the next five years.
Dr. Oetting is watching with trepidation, hoping that the increased safety and increased predictability promised by the laser become a reality.
Dr. Culbertson said he isn’t worrying about what lies ahead. “I’ve gone through the era when phaco was introduced and replaced extracapsular surgery, and the same process is going on now. It’s coming. It’ll be mainstream in the not too distant future.”
Dr. Volpe agreed, and he predicted that in a few years competition will have lowered the price of femtosecond lasers enough to make them a realistic acquisition for ambulatory surgery centers and hospitals.
__________________________
1 Roberts TV et al. Ophthalmology. 2013;120(2):227-233.
2 Nagy Z et al. J Refract Surg. 2009;25(12):1053-1060.
3 Kránitz K et al. J Refract Surg. 2012;28(4):259-263.
4 Kránitz K et al. J Refract Surg. 2011;27(8):558-563.
5 Nagy Z et al. J Refract Surg. 2011;27(8):564-569.
6 Masket S et al. J Cataract Refract Surg. 2010;36(6):1048-1049.
7 Abell RG et al. Ophthalmology. 2013;120(5):942-948.
8 Conrad-Hengerer I et al. J Refract Surg. 2012;28(12):879-883.
9 Conrad-Hengerer I et al. J Cataract Refract Surg. 2012;38(11):1888-1894.
10 Bali SJ et al. Ophthalmology. 2012;119(5):891-899.
Meet the Experts
Surendra Basti, MD Associate professor of ophthalmology, Northwestern University, Chicago. Financial disclosure: None.
William W. Culbertson, MD Professor of ophthalmology, Lou Higgins Distinguished Chair in Ophthalmology, and director of the cornea service and the refractive surgery center at Bascom Palmer Eye Institute, University of Miami. Financial disclosure: Helped develop the OptiMedica laser and oversaw the FDA trial, heads the firm’s medical advisory board, and owns company stock. Consults for Abbott Medical Optics and Alcon; receives research grants and speaking fees from Carl Zeiss Meditec.
Jonathan M. Davidorf, MD Refractive and cataract surgeon and director of the Davidorf Eye Group, West Hills, Calif. Financial disclosure: On the speakers bureau for Al-con and receives grant support from Abbott Medical Optics.
Russell G. Fumuso, MD Comprehensive ophthalmologist at Ophthalmic Consultants of Long Island, N.Y. Financial disclosure: Is an equity partner in Island Eye Surgicenter.
Kevin M. Miller, MD Kolokotrones Professor of Clinical Ophthalmology at Jules Stein Eye Institute, University of California, Los Angeles. Financial disclosure: Consults for Abbott Medical Optics and Alcon.
Thomas A. Oetting, MS, MD Associate professor of clinical ophthalmology, University of Iowa, Iowa City. Financial disclosure: None.
Michael X. Repka, MD, MBA Professor of ophthalmology and pediatrics, Wilmer Eye Institute, Johns Hopkins University, Baltimore; Academy medical director for Governmental Affairs. Financial disclosure: Receives a stipend for serving as a paid physician member consultant to the Academy.
Nicholas J. Volpe, MD Chairman and George and Edwina Tarry Professor of Ophthalmology, Northwestern University, Chicago. Financial disclosure: Consults for Allergan and is a data monitor for Edison Pharmaceuticals.
|