By Arthur Stone, Contributing Writer, interviewing Lynn K. Gordon, MD, PhD, Andrew G. Lee, MD, Ronald W. Pelton, MD, PhD, and Alfredo A. Sadun, MD, PhD
Download PDF
Given the potential for loss of vision and other severe complications, giant cell arteritis (GCA) is a diagnosis that you don’t want to miss. In the second installment of this two-part series: some malpractice lessons from the Ophthalmic Mutual Insurance Company (OMIC) and three case studies to consider.
Malpractice Lessons
In 2015, OMIC published a report on GCA claims.1 The report assessed OMIC claims involving 18 patients diagnosed with GCA between 1993 and 2014.
Key findings. Essential points included the following:
- In 12 of the 18 cases (66%), no physician included GCA in the differential diagnosis. Although GCA was considered by ophthalmologists in each of the remaining six cases, symptoms progressed in five patients when either the treating ophthalmologist or another physician did not follow through to confirm the diagnosis and coordinate treatment.
- Four of the patients were seen only by an ophthalmologist; the remainder were examined by both an eye surgeon and one to three additional physicians.
- All 18 patients experienced severe vision loss, often bilaterally.
Costly to defend. OMIC had to settle twice as many of these claims as it did for claims overall, and the settlements were considerably higher, said study coauthor Ronald W. Pelton, MD, PhD, a board member of OMIC and oculoplastics specialist in Colorado Springs, Colorado.
Red flags to watch for. The OMIC analysis flagged several potential pitfalls that can lead to missed diagnoses and poor outcomes:
Patients presenting with only visual problems. It’s critical to note that the patient may not experience the classic constitutional symptoms. “It can be difficult to diagnose GCA when the only symptom is a change of vision,” Dr. Pelton noted. Four of the 18 patients in the OMIC study presented in this way.
Failure to obtain a thorough and accurate history. In one case, the patient reported a two-day headache and a visual “curtain.” The ophthalmologist erroneously presumed that the patient meant that the curtain was transparent—but during the investigation, the patient described the curtain as dark.
Exploring the precise nature of the vision change might have helped pin down a GCA diagnosis, Dr. Pelton said, and he emphasized the importance of asking older patients about a complete range of constitutional symptoms. “A careful review of signs, symptoms, and systems can help distinguish the few patients who could have GCA from the large number of older patients with eye problems seen daily in ophthalmic practice.”
All told, 15 of the 18 patients (83%) in the OMIC study were experiencing systemic GCA symptoms at the time of their initial ophthalmic assessment, Dr. Pelton said.
However, the ophthalmologists “failed to elicit non–vision-related symptoms in 10 of these 15 patients,” and these inadequate histories “contributed to the delay in diagnosis and were below the standard of care,” he said.
Poor coordination of care. In one claim, the ophthalmologist did not get a thorough history or include GCA in the diagnosis. However, the neurologist to whom he referred the patient did ask the correct questions, made what Dr. Pelton described as a “robust differential diagnosis,” and ordered magnetic resonance imaging (MRI), computed tomography (CT) scanning, and laboratory work, including erythrocyte sedimentation rate (ESR).
A week later, the neurologist realized the lab had yet to perform the ESR, so he mailed the patient a prescription to have it done the next day. The patient never went. Six days later, the patient took the results of the MRI, CT, and lab work to his second visit with the ophthalmologist, who skimmed the report—and failed to confirm whether the ESR had been performed.
Dr. Pelton reported that the experts who reviewed the claim reasoned that “had the ophthalmologist asked the patient, he would have learned that no ESR had been done. This information, combined with [the patient’s] new symptom of fever, could have prompted him to consider GCA and order a stat ESR.”
Need for a checklist. “This constellation of incomplete history, poor coordination of care among physicians, and problems with patient adherence occurred in many of the claims,” Dr. Pelton said.
A potential solution: the use of a “robust appointment and test tracking system,” which can play a pivotal role in preventing diagnostic error, Dr. Pelton said. He developed a GCA checklist to prompt ophthalmologists to ask key questions and document findings. (See www.omic.com/giant-cell-arteritis-checklist.)
 |
|
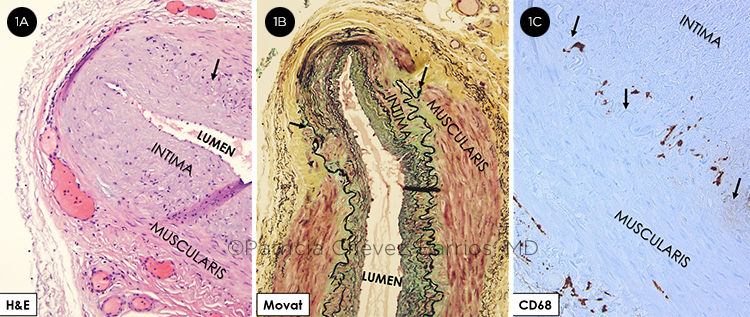
PATHOLOGY CLUES. (1A) Routine hematoxylin and eosin (H&E) stain shows a medium-sized artery with irregular intimal hyperplasia associated with segmental absence of the elastic lamina (arrow) and focal duplication of the lamina. The muscularis has an area of thinning. (1B) Movat pentachrome shows the segmental absence of the elastic lamina (arrows) and fibrosis (blue/green) of the muscularis under this area. (1C) CD68 by immunohistochemistry shows enlarged histiocytes at the level of the internal elastic lamina (arrows).
|
Three Case Studies
As examples of the nuances—and challenges—of GCA diagnosis and treatment, consider the following three cases.
A case of no further loss or gain. In this case, from Andrew G. Lee, MD, at Houston Methodist Hospital, an 80-year-old woman presented with headache, scalp tenderness, jaw pain with chewing, and acute unilateral loss of vision to no light perception (NLP) in her right eye.
Exam and diagnosis. On examination, a right relative afferent pupillary defect (RAPD) was noted; pallid disc edema also was evident in the patient’s right eye.
Lab testing revealed that her ESR was elevated at 100 mm/hour, and her C-reactive protein (CRP) was elevated at 55 mg/dL. A temporal artery biopsy (TAB) showed CD68+ cells on immunohistochemical staining at the level of the internal elastic lamina. A diagnosis of GCA was made, and corticosteroid therapy (methylprednisolone, 1 g/day) was given intravenously for three days. This was followed by oral steroids with a slow taper of 10 mg/month.
Treatment. Although the patient’s symptoms and serum acute phase reactants (i.e., ESR and CRP levels) improved, vision in her right eye remained NLP.
In addition, the patient developed significant steroid-related side effects, including increased blood pressure, blood sugar, and weight. As a result, she was put on tocilizumab (Actemra), with gradual reduction of the steroid dose over the next year. (For more on tocilizumab, see Part 1 of this story in last month’s issue.)
Results. To date, the patient has experienced no recurrence of GCA symptoms or loss of visual acuity in her fellow eye.
A case of an unfortunate outcome. In this case, offered by Alfredo A. Sadun, MD, PhD, at the Doheny Eye Institute in Los Angeles, a 78-year-old woman presented to her ophthalmologist with sudden vision loss in her right eye. The patient denied having typical systemic symptoms of scalp tenderness, jaw claudication, or myalgias. However, she admitted to a loss of appetite and mild weight loss, which she attributed to her grief following the recent death of her husband.
Exam and diagnosis. On presentation, the patient’s visual acuity was hand motions (HM) in her right eye and 20/20 in her left. Her local ophthalmologist noted optic disc edema with hemorrhages in the right eye and concluded that this was probably nonarteritic anterior ischemic optic neuropathy (NAION).
He did consider GCA and, to be safe, ordered ESR and CRP testing, but he did not order a complete blood count (CBC). The ESR came back 46 mm/hr. He applied the empiric formula of age plus 10 (for a woman) divided by 2—and as this equaled 44 mm/hr, he concluded that her ESR was “close enough” to normal. However, the patient’s internist saw the ESR flagged as abnormal and called the ophthalmologist in alarm.
The ophthalmologist reassured the internist that 46 mm/hr for this patient was not very high and that her risk of GCA was low, as she denied the constitutional signs most specific for GCA. The ophthalmologist declined the suggestion that the patient also should have a TAB done.
Symptoms worsen. One week later, the patient noted a severe headache. Two days after that, she experienced jaw claudication that prevented her from being able to chew a bagel. The next day, she lost vision in her left eye.
Treatment. The patient saw her ophthalmologist the following day; at this point, her visual acuity (VA) was HM in both eyes. Pallid disc edema was noted in her left eye.
The ophthalmologist consulted with neuro-ophthalmology at Doheney Eye, and it was suggested that he order another ESR and CRP as well as a CBC. He also followed the suggestion to immediately start her on a course of corticosteroids and then obtain a TAB. Three days later, her ESR was 66 mm/hr, her platelets were 438,000, and her TAB results were positive.
Results. The patient has remained bilaterally blind.
Additional thoughts. This case offers several lessons, Dr. Sadun said, including the following:
- Not all GCA cases present classically. Initially, the patient did not have the specific constitutional symptoms that clearly suggested GCA. Her ESR was only modestly raised.
- Getting all three key lab values is much better than obtaining just one or two.
- HM vision is a red flag. Most patients with NAION have better vision.
- The trajectory of the disease can lead to other systemic symptoms and blindness in the fellow eye. Any patient suspected of having GCA should be cautioned to look for any progression of symptoms—and if this occurs to seek immediate consultation or to visit an emergency department (ED).
A case of misleading lab values. In this case, offered by Lynn K. Gordon, MD, PhD, at the University of California, Los Angeles (UCLA), a 73-year-old woman noted blurred vision and jaw pain while chewing food.
Nineteen days later, she noted the sudden loss of the inferior visual field in her right eye. She also had experienced some weight loss, which she attributed to the recent increase in pain while eating. She did not seek urgent ophthalmic care. Nine days later, the patient went to a nearby ED, where she underwent magnetic resonance angiography and CT angiography; the results of these studies were reported to be unremarkable.
Exam and diagnosis. The following day, the patient sought treatment at UCLA’s ophthalmology clinic. At this point, 29 days had elapsed following the initial symptoms of pain while she was eating.
The patient denied any relevant past medical history. Her best-corrected VA was 20/50 in her right eye and 20/25 in her left, with a 3+ RAPD of the right eye. The funduscopic examination showed pale optic nerve edema in each eye and patchy choroidal ischemia that was documented with fluorescein angiography.
Treatment. The patient was admitted to the hospital. Lab results showed that her ESR was 38 mm/hr, CRP was 7.0 mg/L, and platelet count was 462,000. Visual field testing showed a generalized loss of visual fields in her right eye and a superior and inferior arcuate defect in her left. She received three days of IV methylprednisolone (1 g/day), followed by slow taper of oral prednisone. A TAB was done and was positive with active transmural inflammatory infiltrates.
Results. Three months after her initial presentation, the patient’s VA returned to 20/20 in each eye. However, a 2+ RAPD remained in her right eye, along with a constricted visual field in that eye.
Additional thoughts. Dr. Gordon noted that this case raises the following points:
- It is essential to elicit symptoms, both ophthalmic and systemic. The initial ED presentation should have been highly suspicious for GCA.
- Lab values can be misleading. ESR is not always elevated in GCA—and, for that matter, neither is CRP. The clinical constellation of findings (swollen optic disc along with choroidal ischemia or any retinal artery occlusion) should be considered to be vasculitis until proven otherwise.
- Finally, recovery is possible. Although this happens rarely, it is possible to recover some visual function in GCA. The key is to protect the as-yet-unaffected eye.
___________________________
1 Pelton RW, Menke AM. The Ophthalmic Risk Management Digest. 2015;25(3):1-8, vi.
___________________________
Dr. Gordon is senior associate dean in the Office of Equity and Diversity Inclusion and professor of ophthalmology at the David Geffen School of Medicine at UCLA. Relevant financial disclosures: None.
Dr. Lee is chair of ophthalmology at the Blanton Eye Institute, Houston Methodist Hospital. Relevant financial disclosures: None.
Dr. Pelton practices oculofacial plastic surgery in Colorado Springs, Colo. He is a board member of OMIC and Academy Trustee-at-Large. Relevant financial disclosures: OMIC: C.
Dr. Sadun is the Flora L. Thornton Endowed Chair at the Doheny Eye Center–UCLA and vice chair of ophthalmology at UCLA. Relevant financial disclosures: None.
For full disclosures and the disclosure key, see below.
Full Financial Disclosures
Dr. Gordon None.
Dr. Lee Horizon: C.
Dr. Pelton OMIC: C.
Dr. Sadun GenSight: S; Santhera: S; Stealth BioTherapeutics: S.
Disclosure Category
|
Code
|
Description
|
| Consultant/Advisor |
C |
Consultant fee, paid advisory boards, or fees for attending a meeting. |
| Employee |
E |
Employed by a commercial company. |
| Speakers bureau |
L |
Lecture fees or honoraria, travel fees or reimbursements when speaking at the invitation of a commercial company. |
| Equity owner |
O |
Equity ownership/stock options in publicly or privately traded firms, excluding mutual funds. |
| Patents/Royalty |
P |
Patents and/or royalties for intellectual property. |
| Grant support |
S |
Grant support or other financial support to the investigator from all sources, including research support from government agencies (e.g., NIH), foundations, device manufacturers, and/or pharmaceutical companies. |
|