Download PDF
Researchers have demonstrated the feasibility of directly targeting and editing a gene mutation in the trabecular meshwork to treat the leading genetic cause of primary open-angle glaucoma (POAG).1 This novel approach delivers a one-two punch that both rescues cell function and prevents further glaucomatous damage—and it has implications for persons with mutations in the myocilin gene (MYOC), which have been reported in some 4% of POAG patients, most notably juveniles.
CRISPR to the rescue. “We found that reduction of myocilin gene and protein lowered intraocular pressure [IOP] and prevented vision loss in a mouse model of myocilin glaucoma,” said cell biologist Gulab Zode, PhD, at North Texas Eye Research Institute in Fort Worth, who conducted the study in collaboration with Val C. Sheffield, MD, PhD, at the University of Iowa in Iowa City.
The rescue mission deployed CRISPR-Cas9 technology, a biological cut-and-paste method that homes in on a gene defect, makes a double cut in the DNA, and then deletes, replaces, or repairs the damaged gene. For this study, the researchers used CRISPR (which stands for Clustered Regularly Interspaced Short Palindromic Repeats) to delete the MYOC gene in mice as well as in cultured trabecular meshwork (TM) cells and human donor eyes.
Building on earlier studies. Previously, the researchers found that mutant myocilin is not secreted into the aqueous humor. Instead, it accumulates in the endoplasmic reticulum (ER) of TM cells. ER stress leads to TM damage, resulting in increased outflow resistance and IOP elevation, Dr. Zode said. “We also found that normal myocilin is not required for regulation of IOP. Therefore, deleting the gene completely works in this case.”
Proof of concept. In the murine portion of this study, the researchers injected the MYOC gene intravitreally with the virus Ad5-crMYOC to halt expression of the mutant gene. In young asymptomatic mice, gene deletion prevented IOP elevation compared with controls. In older mice with MYOC ocular hypertension, treatment lowered pressure.
Treatment also significantly increased outflow facility, demonstrating that disruption of mutant MYOC also improves TM cell function in vivo.
Beyond mice. Although the study also demonstrated feasibility of human genome editing in cultured human eyes, additional research is needed before the treatment can be taken to the clinic, Dr. Zode said. “We hope that it translates in humans, but the main purpose was to demonstrate that genome editing is possible in vivo—and, especially, that human donor eyes can be used to study genome editing.”
—Miriam Karmel
___________________________
1 Jain A et al. PNAS. 2017;114(42):11199-11204.
___________________________
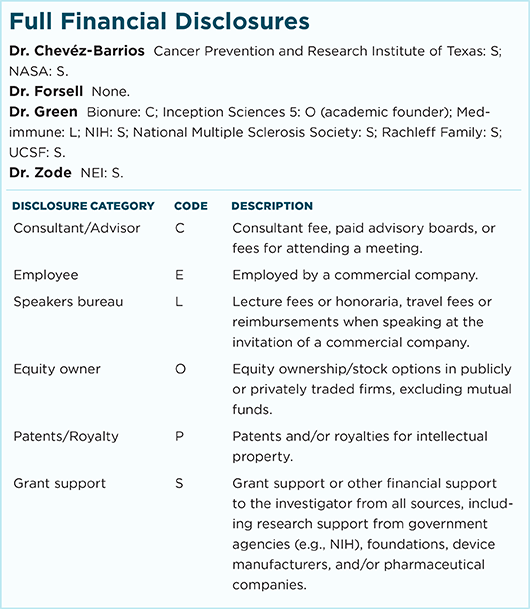
Relevant financial disclosures—Dr. Zode: NEI: S.
For full disclosures and disclosure key, see below.
More from this month’s News in Review