By Mary Wade, Contributing Writer, interviewing Wallace L. Alward, MD, John H. Fingert, MD, PhD, and Janey L. Wiggs, MD, PhD
Download PDF
When is genetic testing for glaucoma useful, and when should it be avoided? What should you tell patients who have a family history of glaucoma—or who might be contemplating direct-to-consumer testing (DCT)?
Researchers are delving into the genetics of all forms of glaucoma, aiming to better understand disease processes and clarify implications for detection and treatment, and they’re rapidly discovering gene variants that can cause—or increase the risk of developing—glaucoma.
However, just because you can order genetic testing for a patient doesn’t mean you should.
Current Recommendations
At present, genetic testing for any ophthalmic disease is warranted only if it will impact treatment or surveillance, according to the Academy’s guidelines on genetic testing.1 (Testing for research purposes is a separate matter.) For glaucoma, this typically means patients with juvenile-onset open-angle glaucoma (JOAG) or congenital glaucoma.
Testing also may be warranted based on a patient’s family history. “We saw a man whose clinical features differed somewhat from the classic presentation for Axenfeld-Rieger syndrome. Also, he has children. For both reasons, we used testing to confirm whether he had primary congenital glaucoma or Axenfeld-Rieger syndrome. With Axenfeld-Rieger syndrome, his children’s risk would be nearly 50%, but for primary congenital glaucoma, their risk would be much lower,” said Wallace L. Alward, MD, at the University of Iowa.
Janey L. Wiggs, MD, PhD, offered another example in which testing was driven by family history. “Our clinic was caring for a father with early-onset glaucoma. He knew that his 3 children were at higher risk,” said Dr. Wiggs, at Massachusetts Eye and Ear Infirmary in Boston. “Beginning when they were babies, he’d conscientiously bring all 3 in for several check-ups a year.” Once testing became available, the results showed that only 1 of the children carried the mutation; the other 2 no longer required close surveillance.
 |
|
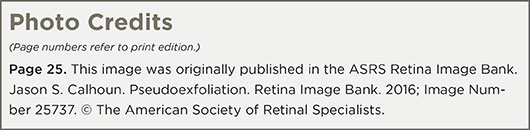
NEED FOR CAUTION. As with pseudoexfoliation glaucoma (shown here), most people who carry genetic risk factors for glaucoma never develop the disease.
|
Potential Benefits of Testing
When applied appropriately, genetic testing allows ophthalmologists to do the following:
- Identify those patients who carry genetic variants that cause JOAG or congenital glaucoma so that they can be followed closely and treated early—and, ideally, so that loss of sight can be prevented or minimized.
- Plan appropriate surveillance (including testing) for people who carry the same genetic variants as their relatives who already have JOAG or congenital glaucoma.
- Reassure family members who don’t carry causative variants that their risk for glaucoma is no higher than that of the general public. This has the potential to save both money and time, as these patients won’t need intensive follow-up.
- Tailor treatment based on genetic factors. At the moment, this is possible for only a few variants.
For the majority of patients who aren’t candidates for genetic testing but have a family history of glaucoma, extra assessment and follow-up are important. Patients and ophthalmologists should discuss their risks and make appropriate care plans. In addition, the immediate family members of these patients should be assessed for glaucoma.
Nuances Abound
As the genetic underpinnings of glaucoma are complex, testing is a complex endeavor as well. Many people who carry 1 or more genetic risk factors never develop glaucoma. One example of this involves LOXL1, a risk factor for exfoliation syndrome. It’s prevalent in many populations worldwide, but most carriers don’t develop glaucoma. Other environmental or genetic factors must be involved.
Here’s how this plays out for primary open-angle glaucoma (POAG) and early-onset glaucoma.
Testing for POAG. John H. Fingert, MD, PhD, at the University of Iowa, explained the differences between 2 categories of gene variants: those that only increase risk and those that can directly cause POAG.
Genes that increase risk. In many POAG cases, the combined action of a number of genetic risk factors contributes to disease development. More than a dozen such factors have already been identified. Each one causes a small increase in risk but, by itself, cannot cause disease.
“Due to the large number of independently inherited factors that must work in concert to promote disease, this form of POAG doesn’t have a discernable inheritance pattern,” said Dr. Fingert. “Instead, it tends to cluster in families or ethnic populations. We are working to discern patterns of genetic risk factors that would allow us to predict POAG.”
Genes that directly cause POAG. Other POAG cases appear to have simple inheritance patterns and are caused primarily by mutations in a single gene. Currently, 3 such genes have been identified. Mutations in these genes are highly predictive of disease, but they occur in less than 5% of POAG patients. Because the prevalence rate is so low, it is currently not feasible to test for these 3 genes in broad, unselected patient populations.
Drs. Alward, Fingert, and Wiggs agree that there’s strong evidence that mutations in the genes myocilin (MYOC), optineurin (OPTN), and TBK1 can be a primary cause of POAG. A number of genetic studies have confirmed these findings. Patients with causative mutations often belong to families with many members who have POAG.
Mutations in MYOC are associated with 3% to 4% of POAG that occurs with elevated intraocular pressure (IOP). Mutations in either OPTN or TBK1 are associated with 1% to 3% of POAG that occurs at low IOP (normal-tension glaucoma, or NTG).
Genetic testing is widely available for MYOC and OPTN (www.genetests.org). No test for TBK1 is available for clinical use at this time.
Treatment recommendations are available for patients with MYOC-related POAG. For instance, certain MYOC variants cause glaucoma that doesn’t respond well to medications, and patients with these variants often benefit from early surgical treatment. In contrast, patients with other MYOC variants do respond well to medications.
Testing for early-onset glaucoma. Mutations in 6 genes (MYOC, PITX2, FOXC1, PAX6, CYP1B1, and LTBP2) can cause early-onset glaucoma (congenital or JOAG), Dr. Wiggs said. “Collectively, these genes account for only about 20% of early-onset glaucoma. But for these patients, the impact of testing on genetic counseling and care can be significant.”
The inheritance patterns of these genes differ. Some cause dominant inheritance (50% of offspring will be affected, on average), while others cause recessive inheritance (only 1 offspring in 4 will be at risk). “An exam alone can’t tell us which inheritance pattern a patient’s glaucoma may carry,” said Dr. Wiggs.
How to Proceed
If you’re interested in ordering genetic tests for your glaucoma patients, here are some points to consider.
Genetic counseling. Only those ophthalmologists who are experienced in interpreting results or who work with genetics counselors should order tests for glaucoma patients, said Dr. Fingert.
Lab standards. Dr. Wiggs advised working only with laboratories that meet Clinical Labs Information Act (CLIA) standards. These labs are inspected regularly to validate testing practices and review reports provided to practitioners and counselors.
“Patients and doctors can rely on results from CLIA-certified labs,” she said. “Ophthalmologists can use the results interpretation section for communicating with patients and their families.” Her institution considers blood samples to be the best source for accurate DNA analysis, she added.
Test selection. Genetic tests can be ordered singly or in combination. For instance, a clinician can order tests for PITX2 and FOXC1 for Axenfeld-Rieger syndrome. Dr. Alward recommended www.genetests.org as a source of information.
Dr. Wiggs and her colleagues have developed a panel test that detects all of the variants involved in early-onset glaucoma.2 This ensures that relevant genes won’t be missed. “Suppose you have a patient who appears to have congenital glaucoma,” she said. “If you test only for the congenital glaucoma mutations in CYP1B1 and LTBP2, you’d miss mutations in genes found in other types of early-onset glaucoma. We’ve learned that these mutations can cause more than one disease.”
Some mutations in CYP1B1 cause JOAG, while others cause congenital glaucoma, she said. The correct diagnosis is also important for counseling family members.
Direct-to-Consumer Testing
While DCT is probably here to stay, the clinical utility of such testing remains murky. For instance, in a survey of 15 companies that offer such testing, researchers found “considerable variation in the cost, scope, and clarity of informational content of DCT for ophthalmic conditions.”3
Glaucoma genetic tests aren’t covered by the main DCT services in the United States. The U.S. Food and Drug Administration recently ruled that while the DCT company 23-and-Me can report allele information for a few heritable medical conditions, it is no longer permitted to include interpretive information. The company’s clients therefore must seek genetic counseling to understand their results.
This is a crucial point: Without professional guidance and support, people have no way of knowing how to use the information provided by DCT results. “I’d tell any patient who had a question about DCT that a result might indicate a slight risk, but not enough to change what the person should do regarding prevention, exams, and other follow-up care,” said Dr. Wiggs.
It’s worth noting that the field of DCT is in a fluid state and is undergoing rapid change on both the scientific and regulatory fronts. In the interim, the experts recommend following the Academy’s guidelines on genetic testing, which state that both clinicians and patients should avoid DCT services.1
Further Reading
Bailey JN et al. Genome-wide association study identifies TXNRD2, ATXN2, and FOXC1 as susceptibility loci for primary open-angle glaucoma. Nat Genet. 2016;48(2):189-194.
Khor CC et al. Genome-wide association study identifies 5 new susceptibility loci for primary angle-closure glaucoma. Nat Genet. Published online April 4, 2016. doi:10.1038/ng.3540
Kumar S et al. Candidate genes involved in the susceptibility of primary open-angle glaucoma. Gene. 2016;577(2):119-131.
Wiggs JL. Glaucoma genes and mechanisms. Prog Mol Biol Transl Sci. 2015;134:315-342.
AAO Task Force on Genetic Testing. Recommendations for genetic testing of inherited eye diseases–2014.
|
Next Steps: Gene-Based Tx
“Our ultimate goal is to understand precisely what’s ‘broken’ in various forms of glaucoma,” said Dr. Alward. “Instead of treating everyone with the same drugs, we’d have drugs that fix specific problems.”
One such drug may be on the horizon. Dr. Alward said that mice bred to develop myocilin-mutation glaucoma can be effectively treated using topical phenylbutarate.4 Patients who have participated in MYOC genetic studies will be eligible to be “first in line” when clinical trials of this treatment begin, Dr. Alward noted.
The opportunity to join clinical trials may soon be available to other participants in glaucoma genetic studies as well, he said.
___________________________
1 www.aao.org/clinical-statement/recommendations-genetic-testing-of-inherited-eye-d. Accessed May 9, 2016.
2 https://oculargenomics.meei.harvard.edu/index.php/gdt. Accessed April 25, 2016.
3 Sanfilippo PG et al. Clin Experiment Ophthalmol. 2015:43(6):578-590.
4 Zode GS et al. Invest Ophthalmol Vis Sci. 2012:53(3):1557-1565.
___________________________
Dr. Alward is the Frederick C. Blodi Chair in Ophthalmology, professor of ophthalmology and visual sciences, and director of the Glaucoma Service at the University of Iowa in Iowa City. Relevant financial disclosures: InnFocus: C. Dr. Fingert is associate professor of ophthalmology and visual sciences and director of the Glaucoma Genetics Laboratory at the University of Iowa in Iowa City. Relevant financial disclosures: None. Dr. Wiggs is the Paul Austin Chandler Professor of Ophthalmology at Harvard Medical School and is vice chair for clinical research in ophthalmology, associate director of the Howe Laboratory, and director of the genetic testing laboratory at the Massachusetts Eye and Ear Infirmary in Boston. Relevant financial disclosures: None.
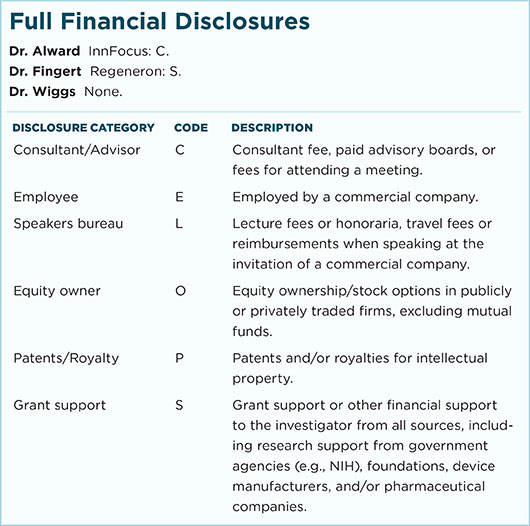
For full disclosures and the disclosure key, see below.