Download PDF
Correlating structure and function in the age of OCT.
When it comes to monitoring patients, “We glaucoma specialists have traditionally hung our hats on the visual field,” said Sanjay G. Asrani, MD. Then along came optical coherence tomography (OCT). Although both are used to monitor glaucomatous progression, automated perimetry tests show functional change, while OCT reveals structural changes. Now evidence is accumulating that functional change lags behind structural change, sometimes by years. In fact, there is a point in the early stages of glaucoma when OCT reveals structural changes, but the visual field (VF) remains stable.
Given these findings, how does the ophthalmologist correlate the structural changes seen on OCT with the VF? (All references in this article are to spectral-domain OCT; see “Time to Upgrade to SD OCT?” below) And which modality should drive treatment decisions?
“Nowadays, I’m not waiting for the VF to confirm progression” in glaucoma patients or suspects, said Dr. Asrani, at Duke University. He added a caveat, however: “When I see those changes [in retinal nerve fiber layer and macular thickness], I review the images and make sure there are no artifacts. Then I’m confident and can start or step up treatment.”
But when is that confidence warranted? Here’s what the experts have to say.
Lag Time Conundrum
Before OCT, ophthalmologists could make only a general estimate of glaucoma progression based on the appearance of the optic nerve, Dr. Asrani said. “We were looking for cupping that increases with loss of the retinal nerve fiber layer [RNFL]. With OCT, however, we can measure ganglion cell loss and RNFL thinning.”
The advent of SD-OCT made it possible to broadly sweep the entire posterior pole to map losses caused by glaucoma. Those losses are detectable by pattern recognition, specifically an arcuate shaped loss of thickness of the retina, Dr. Asrani explained. “This allowed us to detect glaucoma in the very early stages, before a change in the VF.”
However, many clinicians still wait for VF confirmation before intervening, Dr. Asrani said. “But the VF lags behind [structural change] by approximately 1 year. So we may need to start believing the OCT for structural change as long as we are sure it is real structural change. Then we can be more reliant on the OCT and treat based on that.”
Treatment challenges. However, using OCT to drive treatment decisions introduces other complexities. Say you start treatment based on OCT. Twelve months later, OCT reveals no further changes in structure. But now the function is changing. “We don’t know why that is,” Dr. Asrani said. “It could be that treatment wasn’t sufficiently aggressive, though in that case structure would have continued to change.”
More likely, the functional tests aren’t sensitive enough to pick up change early, Dr. Asrani continued. “Our VF testing is not accurate in the common way we do it because each spot is separated from another spot by 6 degrees. Intervening tissue can easily be lost, and you will not test it. Only when the tissue threshold drops in the area where we saw the structural change does function change.”
It’s possible that an emerging technology such as frequency doubling or flicker-defined perimetry might pick up concurrent changes in structure and function. In the interim, said Dr. Asrani, “The results in front of us are going to be initially confusing, until we realize that the change in VF that we’re seeing is the functional correlate of the structural change we were seeing 1 year ago.”
Gadi Wollstein, MD, agreed, though he said that the lag time—which he calls a window—when only structural changes are detected might be as long as 8 years. (A just-published study by Kuang et al. supports this time frame.1) He added that the window is dependent on highly subjective functional assessment. In the early disease stages, there is so much noise in VF testing that disease is hard to detect. With OCT, there is less noise in the beginning, he explained. “The lag time is probably related to the way we test function.”
Is there a tipping point? Dr. Wollstein, at the University of Pittsburgh, posits that there’s a tipping point, a threshold beyond which both structure and function change rapidly, and VF loss becomes clinically observable. He has estimated the tipping point to be around a 17% loss in RNFL thickness.2 That’s how much structural loss “appears to be necessary for functional loss to be detectable using the current testing methods.”
In very advanced disease, the situation is reversed, Dr. Wollstein said. At that stage, there’s a “floor effect,” where tissue is so damaged that OCT can no longer detect structural change, though perimetry is still registering functional changes.
“It’s difficult to detect change with objective structural testing” in advanced disease, agreed Steven L. Mansberger, MD, MPH, at the Devers Eye Institute in Portland, Ore. Different tests are good at different stages of the disease, he said. “OCT has greater sensitivity for detecting progression in early and moderate glaucoma.”
Pearls for OCT Use
Dr. Asrani: OCT is difficult to interpret in high myopes (greater than –8 or –9 D) because the structures of the retina do not conform to the normative database. These eyes are also associated with other artifacts, such as difficulty acquiring a good image due to excessively long axial length or myopic retinal schisis affecting peripapillary RNFL thickness. However, macular thickness and Bruch’s membrane opening measurements may still be useful in such eyes. Unfortunately, these are the eyes where clinical interpretation of the optic nerve is most difficult due to tilt and size of the nerve.
Dr. Chauhan: OCT can significantly enhance the clinical evaluation of the optic nerve head, especially when the initial optic disc examination is equivocal.
Mr. Hoffmeyer: If you see red on OCT printouts, ask: Did pathology skew the results? Was the signal strength strong? Was the OCT lens clean? Was it thrown off by media opacity—floaters or overlying retinal pathology, such as an epiretinal membrane?
Dr. Mansberger: At Devers Eye Institute, to improve the optics, we use an artificial teardrop in each eye before imaging. This makes the cornea clearer and improves the signal strength and quality of the scan.
Dr. Wollstein: When assessing patients, physicians need to consider that the relationship between structure and function is changing along the spectrum of the disease. There’s a period of time when one way of assessing changes might be more informative than another. We don’t want to miss that window of time when we can halt further progression of disease and preserve vision. We can wait, but that’s probably not best for our patients.
|
OCT in Clinical Practice
When to image? Any type of structural assessment requires several tests in a short period of time to establish a baseline, Dr. Mansberger said. With OCT, you need 5 to 8 scans, depending on the frequency of imaging, slope of loss, and variability of results.
Dr. Mansberger advised clinicians to consider performing OCT 2 or 3 times within the first year to determine progression as early as possible. “However, no one knows the exact number of tests needed because of individual rates of disease progression and variability.” He added that you don’t need to obtain OCTs in patients with severe glaucoma who already have a flat RNFL rather than a double-hump pattern. “They have already reached the floor of their testing.”
When to treat? “If the signal strength is similar, the segmentation algorithm is working, and the tissues appear to be thinning, then I’ll act, despite having no change in VF,” Dr. Mansberger said. But if the patient is elderly or sick, Dr. Mansberger may wait for VF confirmation before treating. Conversely, he’s more aggressive with younger patients.
“These are the most complicated situations,” Dr. Wollstein said, when only structural change is evident. “Do I start treating the patient? The answer is not clear-cut, partly because we can’t agree on what to call progression.” He added, “In the context of early stages of disease, I don’t expect much change in VF. But OCT gives me reliable information, so I can judge even small changes.”
Dr. Wollstein tends to rely on structural assessment. “I would not necessarily change the treatment right away, but I’d bring the patient in earlier, perhaps in 6 months. If it’s a repeatable and reliable test, I would consider changing, adding, or starting treatment, even without clear-cut VF change.”
How to get the best scan. OCT is not infallible. These structural tests can be unreliable up to 20% of the time, Dr. Mansberger said. “It’s important for the practitioner to look at the signal strength and the segmentation [for determining RNFL thickness] because someone may appear to be getting worse because of artifacts.”
Need for repetition. Dr. Mansberger stressed the importance of repeating the test. If you’re very concerned, repeat the test in a month. Otherwise, repeat at the next regular visit. “We never use these tests in isolation. So if somebody seems to be getting worse on OCT, and everything else looks good— pressure, optic nerve, VF—be aware that this may be artifact or something else going on.”
Need for proper placement. The optic nerve should be well centered, and the scan should be in the right place every time, said Gregory Hoffmeyer, imaging specialist with Carl Zeiss Meditec. Whether your machine uses automated eye tracking and/or autocentering or requires manual operator placement, “You don’t want to eye-track to the wrong place every follow-up visit,” he said.
It’s also important to steer around any opacities—cataracts, cloudy lens capsules, thick vitreous floaters—to get the best possible signal strength, Mr. Hoffmeyer said. “A lot of doctors make technicians go back again and again until they get high signal strength, but sometimes that’s not going to happen. You won’t get a 10 signal strength [or 100, depending on the device’s calibration] in a patient with a +4 cataract. This is a near-infrared light; it’s not ultrasound, CAT, or MRI,” he said. He added, “A 100% clean shot is not always possible.” But the opacity generally won’t block the entire scan, he added. “You’re still going to get some usable OCT data in most cases.”
Don’t be misled by red. Opacities and other artifacts can confound software algorithms, which color-code the data against normative databases: green for good; yellow for low end of normal; red, generally for below normal. Sometimes, though, when you see red, it’s not glaucoma.
It’s not uncommon for coexisting disease, such as AMD, to confuse the algorithms, Mr. Hoffmeyer said. “You have to be diligent. Is something else going on? There’s no easy button with OCT. It’s great, but it’s not going to tell you absolutely: This person has glaucoma.” He advised: “Beware of ‘red disease,’ as some have labeled these situations.”
Beware of confounders. Dr. Asrani looks for changes in the superotemporal and inferotemporal quadrants, where the earliest changes occur. “When I see both the RNFL and a macular change, I’m more confident that the change is real and not due to software error or coexisting pathology.”
But some diseases can cause substantial confounding on OCT, including epiretinal membranes, posterior vitreous traction and subsequent release, myopic schisis, and uveitis. In one study, Dr. Asrani found the likelihood of imaging artifacts in roughly 15% to 36% of scans obtained in patients being evaluated for glaucoma.3 Artifacts occurred in 28.2% of macular thickness scans (6 not obvious on the final printout). Among RNFL scans, 20% contained artifacts (7 not evident on the final printout).
Dr. Asrani and his colleagues have reported that in uveitic patients, RNFL parameters on OCT do not accurately reflect glaucoma severity.4 During periods of active uveitis and elevated IOP, patients with uveitis-associated glaucoma had relatively normal RNFL measurements. Conversely, when uveitis was controlled, OCT images showed a paradoxical thinning of the RNFL and increased cupping. This may appear as glaucoma progression.
He urged caution when interpreting normal-appearing RNFL measurements in these patients. Be aware that continued thinning of the RNFL and increased cupping, despite good IOP control, may be due to resolution of the uveitic edema, rather than any glaucomatous change, he said.
Handling challenging patients. OCT hasn’t replaced automated perimetry, but for some patients it may be the most viable option. For example, Dr. Asrani doesn’t do VFs in patients who can’t hold attention to a central fixation, are trigger-happy, have Parkinson’s or arthritis, or are old and infirm.
He has found that some people don’t return for a follow-up because the VF can be psychologically stressful. But if he tells patients, “Next time, I’ll just do an OCT,” they’re more likely to return, he said. When Dr. Asrani does use perimetry, he explains that he won’t recommend stepping up treatment until the results correlate with the structural test. This tends to help patients relax. And if he recommends a treatment based on both structural and functional tests, “They are more apt to believe me, because I’m presenting them with an objective measure of structural change.”
Time to Upgrade to SD-OCT?
Your office has time-domain OCT (TD-OCT). Is it time to upgrade?
The experts suggest that it is. SD-OCT far surpasses the capabilities of TD-OCT, Dr. Asrani said. It’s more reliable and 100 times faster than the original 1997 models. Today’s machines acquire 25,000 to 52,000 A-scans per second, compared with the first generation’s 400. “If someone has TD-OCT, it’s time to upgrade.” Mr. Hoffmeyer agreed: “TD-OCT had a good long run, but OCT is no different from all technology. With advances occurring at exponential rates, SD-OCT is essentially the de facto standard now.”
As Mr. Hoffmeyer pointed out, “You’re getting a small piece of the puzzle with TD-OCT. It’s still good data, but [the technology] is very limited in what it produces.” Moreover, “There’s little room for error with a TD-OCT,” he said. In contrast, SD-OCT is capable of obtaining an exponentially larger data cube of the optic disc or macular area, giving several million data points instead of a few thousand.
As for the newer swept-source OCT (SS-OCT), Dr. Asrani said it’s reasonable to hold off for the time being. While SS-OCT confers improved depth of range imaging and increases speed from 26,000 up to 300,000 axial scans/second, “We’re not yet seeing a tremendous advantage.”
|
New Anatomical Insights
Perhaps a new paradigm proposed by Balwantray C. Chauhan, PhD, and Claude F. Burgoyne, MD, will help to increase diagnostic accuracy.5 Using SD-OCT, they found that what the clinician interprets as the disc margin using conventional assessment methods doesn’t correspond to the anatomy.
This new information challenges assumptions underlying the traditional optic disc margin–based neuroretinal rim evaluation, said Dr. Chauhan, at Dalhousie University in Canada. The researchers’ SD-OCT studies show for the first time that the disc margin, as observed in clinical exams or in photographs, is rarely a single anatomic entity; rather, it varies within the eye and between eyes. And it is often not the true anatomic outer border of the neuroretinal rim because of regionally variable and invisible extensions of Bruch’s membrane.
Rather than looking at the RNFL, which is measured on the retina surface, this new paradigm suggests quantifying the neuroretinal rim from Bruch’s membrane opening in an anatomically and geometrically accurate manner. Dr. Chauhan explained that the retinal ganglion cells send their axons, like wires, out to the brain. The optic nerve head (ONH) supports these “wires” as they exit the eye.
“We’re proposing that Bruch’s membrane opening is a more logical place to measure the neuroretinal rim,” Dr. Chauhan said. A surrogate estimate of how many axons remain in the eye can be obtained by measuring the thickness of the RNFL in the retina or the neuroretinal rim at the ONH.
He added, “Everything we’ve published is available [as open access]. I’m hopeful that a lot of instrument manufacturers will embrace these ideas.”
What’s Next?
Dr. Mansberger envisions a future when “structural and functional testing will become more refined, precise, and interdependent.” Perhaps an all-purpose machine will be able to do all of the following: 1) perform highly sensitive perimetry and OCT testing in glaucoma suspects; 2) use standard achromatic automated perimetry and OCT testing in mild to moderate glaucoma patients; and 3) use perimetry that focuses on areas of remaining vision with larger-size stimuli for advanced glaucoma.
Sound improbable? Then consider the reaction, not so long ago, when early OCT captured 6 radial slices in just under 2 seconds. “We were astonished,” Mr. Hoffmeyer said. “But now, most SD-OCTs are capable of hundreds of scans/slices in a few seconds. It’s like going from ‘pizza cutter scanning’ at every clock hour to a copy machine covering the entire macular or ONH zone.”
___________________________
1 Kuang TM et al. Ophthalmology. July 18, 2015. [Epub ahead of print].
2 Wollstein G et al. Br J Ophthalmol. 2012;96(1):47-52.
3 Asrani S et al. JAMA Ophthalmol. 2014;132(4):396-402.
4 Moore DB et al. Ophthalmology. 2014;122(3):511-517.
5 Chauhan BC, Burgoyne CF. Am J Ophthalmol. 2013;156(2):218-227.
Meet the Experts
SANJAY G. ASRANI, MD Professor of ophthalmology at Duke University School of Medicine in Durham, N.C. Relevant financial disclosures: Heidelberg Engineering: L.
BALWANTRAY C. CHAUHAN, PHD Professor of ophthalmology and research director at the Department of Ophthalmology and Visual Sciences at Dalhousie University in Halifax, Nova Scotia. Relevant financial disclosures: Allergan: C; Heidelberg Engineering: C,S.
GREGORY HOFFMEYER Imaging specialist at Carl Zeiss Meditec. Relevant financial disclosures: Carl Zeiss Meditec: E.
STEVEN L. MANSBERGER, MD, MPH Vice-Chair and director of Glaucoma Services at the Devers Eye Institute and clinical associate professor of ophthalmology and public health and preventive medicine at Oregon Health & Science University in Portland, Ore. Relevant financial disclosures: Allergan: C,S; Bausch & Lomb: C; Envisia: C,S; NEI: S; Santen: C; Welch Allyn: C.
GADI WOLLSTEIN, MD Associate professor of ophthalmology and bioengineering and director of the Ophthalmic Imaging Research Laboratories at the University of Pittsburgh School of Medicine in Pittsburgh, Pa. Relevant financial disclosures: None.
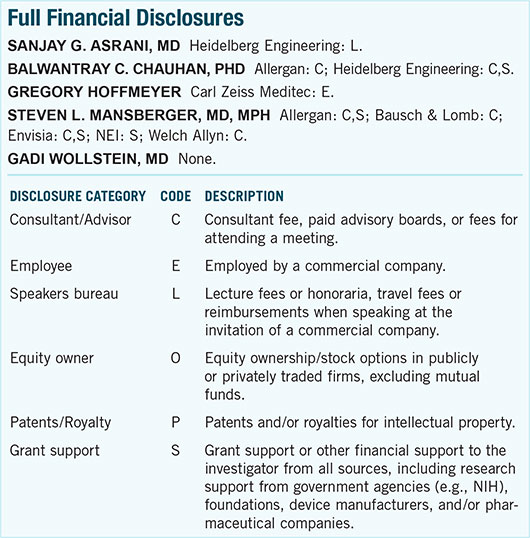
For full disclosures and the disclosure key, see below.
|