Download PDF
It took the participation of cornea specialists from 21 countries; multiple rounds of Delphi-style questions, responses, and revisions; and face-to-face discussions. What emerged from that complex international project was worth the effort: a global consensus on keratoconus (KC) and ectatic diseases.1
Christopher J. Rapuano, MD, said that the idea was talked about at meetings for years, but he credits José A. P. Gomes, MD, PhD, in São Paulo, Brazil, for putting the talk into action. “He realized that there’s a disconnect between what’s in the literature and what people are doing, not only in South America, but around the world,” said Dr. Rapuano, who is chief of the cornea service at Wills Eye Hospital. “The idea was to assimilate all this information and make it useful to clinicians.” Here are some of the highlights of the consensus document.
To manage KC, first define it. In order to determine what interventions are effective—and when they should be attempted—the condition and its progression must be consistently defined.
Moderate to severe KC is easy to diagnose, said Dr. Rapuano: “You can see it at the slit lamp; you don’t even need topography.” But recognizing mild, subclinical disease depends on more recently developed technologies, such as Scheimpflug imaging or optical coherence tomography, which can detect posterior corneal abnormalities. Indeed, the panel agreed that the mandatory findings for KC diagnosis include posterior corneal elevation abnormalities, in addition to abnormal distribution of corneal thickness and noninflammatory corneal thinning.
The panel also identified risk factors for KC, including Down syndrome, family history, connective tissue disorders, ocular allergy, and mechanical factors such as eye rubbing and floppy eyelid syndrome.
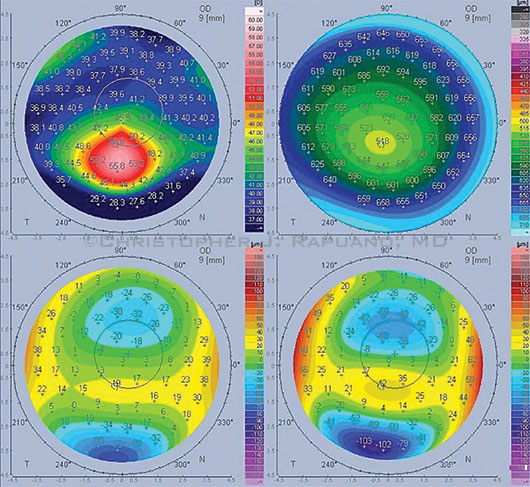 |
DUAL SCHEIMPFLUG. Imaging shows KC features, such as inferocentral anterior corneal steepening (top left) and inferocentral posterior elevation (bottom right).
|
Treatment algorithm. The group developed a treatment flowchart that proceeds from nonsurgical steps through corneal transplant surgery, as needed. Dr. Rapuano noted that, in this schema, the progression to more invasive therapy is based on whether the patient can achieve satisfactory vision. “One important point was that even though a patient can see 20/30 in your office with a contact lens, it’s not necessarily satisfactory BCVA. If the patient can’t tolerate the lens for more than an hour, surgery may be indicated.”
An underappreciated recommendation. Two nonsurgical measures were graded as “most important.” The first is deceptively simple: Counsel the patient to avoid eye rubbing. “I feel strongly, as do many cornea specialists around the world, that eye rubbing is an important component of either causing keratoconus or making it worse. But I think that message is not fully appreciated by the general ophthalmology community,” said Dr. Rapuano.
The second is to prescribe topical antiallergy medications and lubricants for patients with allergies, he said, because allergic itching promotes eye rubbing and, thus, contributes to KC progression.
Surgical choices. The group found that anterior lamellar keratoplasty (ALK), especially deep ALK, (DALK), and penetrating keratoplasty are the most commonly performed surgeries for KC. Some type of ALK is now attempted in more than 60 percent of KC patients eligible for surgery.
Role of cross-linking. Although corneal cross-linking (CXL) is not FDA approved in the United States, it is available to and performed by almost 85 percent of the panelists, who rated it “extremely important” for patients of any age who have progression. Consideration of CXL appears early in the treatment flowchart and is sometimes used together with other therapies for KC. “Out in the rest of the world, it’s a standard treatment for patients with keratoconus,” said Dr. Rapuano, “even before documented progression, if they are deemed to be at high risk for progression.”
—Peggy Denny
___________________________
1 Gomes JA et al. Cornea. 2015;34(4):359-369.
___________________________
Dr. Rapuano reports no related financial interests.
More from this month's News in Review