Download PDF
A handheld confocal microscope originally developed for dermatologists can be used to perform noninvasive “optical biopsies” to diagnose eyelid and conjunctival malignancies, Italian and French researchers have reported.
Viewing individual cells. The group, based at the University Hospital of Saint-Étienne in Saint-Priest-en-Jarez, France, reported that a handheld reflectance confocal microscope (VivaScope 3000; Caliber Imaging & Diagnostics) enabled them to see images of individual cells in the suspicious lesions, enabling diagnosis of melanoma and squamous cell carcinomas.1
Each image covers an area of 920 × 920 μm (more than double the field of view achieved by reflectance confocal microscopes that are not mobile) and up to 250 μm in depth. The horizontal optical resolution is 1.25 μm.
“The device offers you some information that is impossible to find with other devices. We observe the cells in vivo, which is amazing,” said Elisa Cinotti, MD, PhD, at the University of Siena in Siena, Italy. “You can come to a diagnosis very early compared to the clinical examination, which gives you only a macroscopical view.”
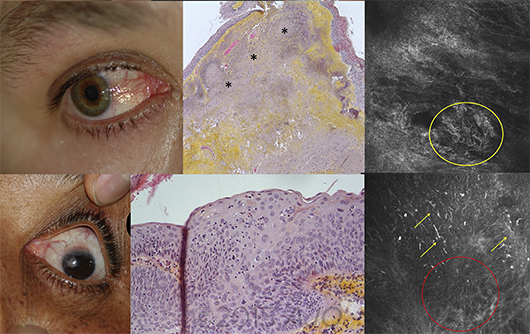 |
COMPARISON. Clinical (left), histologic (center), and handheld reflectance confocal microscopy (right) images in patients with pinquecula (top) and squamous cell carcinoma (bottom). (Note: These images are from an earlier study.)
|
Procedural details. The process of using handheld in vivo confocal microscopy (IVCM) to diagnose suspicious tissues takes 5 to 10 minutes, Dr. Cinotti said. The clinician begins by topically anesthetizing the eye, then applies a transparent ophthalmic gel to the area being examined. With the patient supine, the physician places the 5-mm tip lightly on the lesion to be examined and moves it around on the surface as needed to optimize the image. (Recently the tip was redesigned to be removable for sterilization, she said.) The biomicroscopic images are displayed on a nearby monitor.
To test the device for ophthalmic use, a team of 3 dermatologists and 3 ophthalmologists conducted a prospective, observational study on 298 consecutive patients with eyelid margin or conjunctival lesions. Patients underwent clinical examination at the slit lamp and with IVCM. Suspected malignancies were excised from 155 eyes, and histopathology was performed to verify the original diagnoses.
Better sensitivity. The researchers found that, compared to the slit-lamp exam, the handheld confocal microscope showed higher sensitivity for malignant tumors of the eyelid margin (98% vs. 92%) and conjunctiva (100% vs. 88%).
IVCM identified all the malignant conjunctival tumors and missed only 1 cancer on the eyelid margin, a basal cell carcinoma, the authors reported. In contrast, clinical examination with the slit lamp failed to identify 5 basal cell carcinomas of the eyelid margin and 3 malignant melanomas of the conjunctiva.
“I saw some cases in which there was hyperpigmentation of the conjunctiva of a few millimeters. With IVCM, it was clear that they were melanomas. On the clinical examination, it was impossible [to reach an accurate diagnosis],” Dr. Cinotti said.
Problems with specificity. The specificity results were mixed: They were higher compared to the slit-lamp exam for the malignant eyelid margin tumors (74% vs. 46%) but lower for malignant conjunctival tumors (78% vs. 88%). Although the IVCM correctly diagnosed 100% of the cases of conjunctival malignant melanoma, it misdiagnosed 7 benign conjunctival lesions as melanoma (74% specificity for melanoma), the authors reported. As for the eyelid lesions, 5 were misdiagnosed as melanoma (64% specificity for melanoma).
Dr. Cinotti explained that some types of tumors contain large cells that make the IVCM images difficult to interpret or ambiguous. “Our study had a large group of patients, but we still have a lot of work to do on this. It’s still quite new. We need more work on the criteria for diagnosis,” she said.
—Linda Roach
___________________________
1 Cinotti E et al. JAMA Ophthalmol. Published online June 22, 2017.
___________________________
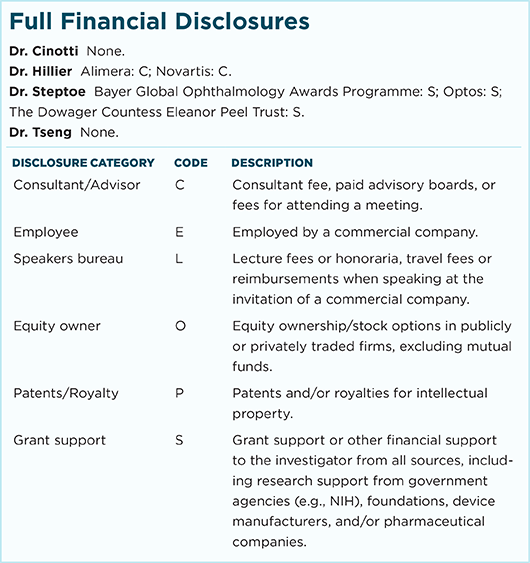
Relevant financial disclosures—Dr. Cinotti: None.
For full disclosures and disclosure key, see below.
More from this month’s News in Review