Download PDF
There’s a lot riding on the headache or facial pain syndrome patient,” said M. Tariq Bhatti, MD, at Duke Eye Center. Evaluating this type of patient, he said, is a precarious balancing act made all the more challenging by a vast differential diagnosis, subjective symptoms, and conditions ranging from benign to life threatening. If overly cautious, you might send a patient to the ER, only to waste the time of your emergency medicine colleague and unnecessarily utilize health care dollars. “But if you miss something, the patient might end up with a ruptured aneurysm with a devastating outcome.”
Regardless of your area of practice, when you assess such patients, you must be a truly comprehensive ophthalmologist. Signs or symptoms manifesting in virtually any part of the eye—and beyond—may provide the diagnostic clues for determining the source of the head or facial pain and, most important, for recognizing the red flags of vision- and life-threatening conditions.
The History: Gathering Clues
In many cases, patients with serious conditions will go straight to the ER, said Deborah I. Friedman, MD, MPH, at University of Texas Southwestern Medical Center. “But ophthalmology is often the first stop in the pathway patients take when experiencing headache.” Even without visual symptoms, she said, patients may think the source is their eyes because the pain is often located in the front of the head or around the eyes.
Ask the right questions. The history is key, said Dr. Bhatti; take the time to really listen. “Ask pointed questions so you don’t miss a vision- or life-threatening condition.” (See “Key Questions for Head and Facial Pain.”) Be sure to conduct a thorough review of systems, he said, checking for associated neurological symptoms and for other potential contributors such as medications or a history of trauma.
Robert C. Sergott, MD, at Wills Eye Institute, agrees that thorough questioning can provide invaluable clues, such as when the headache occurs. For example, “A headache that appears mostly in the morning could be due to increased intracranial pressure from a tumor or pseudotumor cerebri,” he said. Also, sleep apnea could be the culprit, or certain sleeping positions might exacerbate the pain of cervical spine disease.
Enlist the family. To get the full picture, you may need to ask questions of family members, as well. Remember that a pediatric patient or teen may be virtually nonverbal, said Dr. Sergott, so a parent may be your best source. Likewise, some adults will minimize their complaints—that’s where “matrimonial neuro-ophthalmology” comes in, he said. Geriatric patients may be slow to express themselves or struggle with memory, so talking to a spouse or adult child may be especially helpful.
But, regardless of the patient’s age, remember that communication may be impaired if a serious condition is present, such as high intracranial pressure or bleeding in the subarachnoid space, said Dr. Sergott.
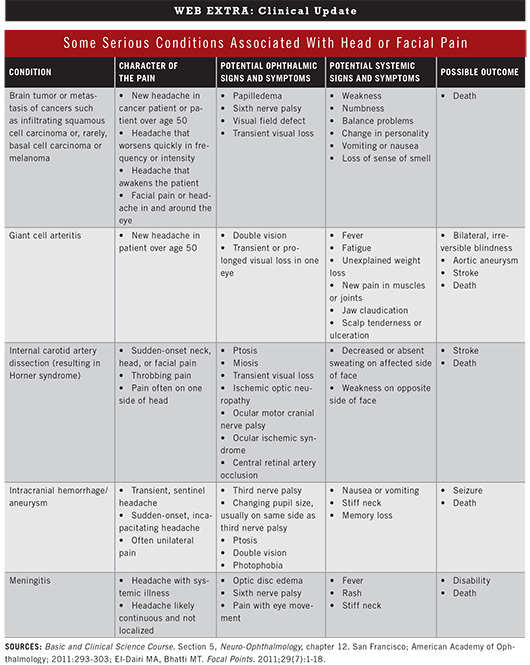
Pay attention! There are particular situations that should catch your attention, said Dr. Friedman. These include patients complaining of the first or worst headache they’ve ever had; a new headache in patients who are older than age 50 or have cancer or HIV; an accelerating pattern of headache; a headache with systemic illness and rash, fever, or stiff neck; or a headache with papilledema or focal neurological symptoms and signs other than typical migraine aura. (For more information, see the table “Some Serious Conditions Associated With Head or Facial Pain” below.)
Ophthalmologists may be too ready to attribute headache to ocular surface disease, said Dr. Sergott, but problems such as corneal dryness or blepharitis should be the last things to worry about. “First, rule out problems that can cause significant morbidity and mortality.”
Key Questions for Head and Facial Pain
When did the pain begin?
- Was the onset sudden or gradual?
- Is the pain constant or intermittent?
- Is it getting worse?
Where is the pain located?
- Unilateral or bilateral?
- Diffuse, focal, or radiating?
What is the quality of the pain: knifelike, boring, throbbing, dull?
How severe is the pain, on a scale of 1 to 10?
When does the pain get worse?
- In the morning or evening?
- When standing or bending?
- When exposed to certain foods or other triggers?
Is the pain associated with other symptoms such as numbness?
Is there a family history of headache?
___________________________
SOURCE: Basic and Clinical Science Course. Section 5, Neuro-Ophthalmology, chapter 12. San Francisco; American Academy of Ophthalmology; 2011:293-303.
|
The Exam: Ocular or Neurological?
“There is a handful of conditions you need to look for to see if the problem is coming from the eyes,” said Dr. Friedman. These include angle-closure glaucoma, dry eye, intraocular or orbital inflammation, and, rarely, an uncorrected refractive error. Be sure to take note of any symptoms that may be present in addition to the headache or facial pain.
Anatomic approach from front to back. After measuring the patient’s vision, Dr. Sergott takes an anatomic approach, starting with a slit-lamp exam of the front of the eye and working to the back of the brain. He first checks the cornea to assess the status of the epithelium and then the anterior chamber, looking for evidence of possible keratitis and uveitis.
He looks for signs of pigment dispersion syndrome, such as Krukenberg spindles and iris transillumination defects, and of angle-closure glaucoma. Is the angle narrowed? Did the patient complain about headaches that wax and wane? Because angle-closure glaucoma can be intermittent, there may be signs of previous increases in intraocular pressure (IOP) even if IOP is normal at the time of the exam, said Dr. Bhatti. One sign of past IOP spikes is glaukomflecken, small, anterior subcapsular opacities of the lens.
Next, Dr. Sergott checks for lens subluxation; an anteriorly displaced lens may cause angle closure, while a posteriorly displaced lens may be associated with vitritis. Or, if the patient is pseudophakic, he said, “The IOL could be malpositioned and chafing the iris.”
Back of the eye. A complete dilated exam gives a good view of the posterior pole—the optic nerve and retina, both central and peripheral. Are there signs of glaucoma or papilledema? A chalky white swelling of the optic nerve, in conjunction with head pain, raises suspicion for giant cell arteritis (see below under “Age makes a difference”).
Another condition you don’t want to miss, said Dr. Bhatti, is optic neuritis: Although its ocular symptoms generally resolve spontaneously over several months, optic neuritis is often associated with multiple sclerosis. If you suspect an optic nerve problem—a tumor or aneurysm compressing the optic nerve, for example—color vision testing may also be appropriate, he said.
After the optic nerve, Dr. Sergott checks the orbit and paranasal sinuses together, and then moves to the cavernous sinus and sphenoid sinus to rule out possible inflammatory or infectious disease. “This is an often-overlooked area,” he said, “but it’s important to remember that older patients or patients with diabetes, in particular, can be prone to fungal infections.”
Movement, reflexes, sensation. “Limitation of eye movements in either eye suggests an ocular motor cranial nerve problem,” said Dr. Bhatti. The pupil can provide crucial clues: Check the size of the pupils and the pupillary light reflex, and test for the presence of a relative afferent pupillary defect (RAPD). “An abnormality of the pupil can be a sign of a serious neurological or visual system problem. Ptosis along with a dilated pupil can be a sign of a third nerve palsy.” If there are signs of a problem, evaluate the function of other cranial nerves such as the trigeminal nerve further by checking the sensitivity of the cornea, forehead, and cheek. A pupil-involving third nerve palsy is a true red-flag finding that requires further investigation, as it may signal an aneurysm.1
Dr. Friedman advised paying special attention to the pupil, fundus exam, and visual fields. “Visual fields are especially important in patients with pseudotumor cerebri,” she said. If there are any abnormalities on confrontation visual field testing, you might double-check results with automated perimetry, added Dr. Bhatti.
Age makes a difference. For each anatomic area, Dr. Sergott’s list of possible causes varies according to the age of the patient. For example, in a pediatric patient with headache, the differential diagnosis includes papilledema and a brain tumor (Fig. 1); or in a child with retrobulbar pain and decreased vision, optic neuritis could be to blame.
However, if a patient over age 50 presents with a new headache, transient visual loss, and double vision, consider giant cell arteritis (GCA), which is a true ophthalmic emergency. “You need to order an erythrocyte sedimentation rate, a C-reactive protein test, and, possibly, a platelet count,” said Dr. Sergott. “If you have a high index of suspicion, put the patient on 80 mg of prednisone orally or admit him or her for IV corticosteroid therapy and arrange for a superficial temporary artery biopsy.” Without prompt treatment, GCA carries a high risk of causing bilateral blindness.
|
Ocular Sign of Brain Tumor
|
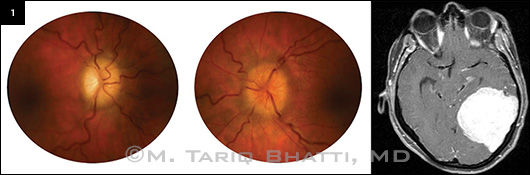 |
Eye findings may signal a serious neurological disorder, as seen in this patient with papilledema due to intracranial meningioma.
|
Imaging: Digging Deeper
If you can’t find an intraocular cause, you need to be concerned about the central nervous system or areas you can’t see on an eye exam, said Dr. Sergott. “When the eye exam is normal, it doesn’t mean there isn’t significant pathology in the skull or brain,” he said. “So if you are presented with a patient complaining of pain in or around the eye, you need to lower the threshold to get an MRI or CT scan.”
In many locations, CT scans are easier to obtain than MRIs, but “most patients with neuro-ophthalmic problems should get an MRI of the brain and orbits with contrast and fat suppression,” said Dr. Bhatti. “A CT scan without contrast is great if you’re looking for trauma or subarachnoid or intraparenchymal hemorrhage, but it will miss many neuro-ophthalmic problems, such as pituitary apoplexy, optic neuritis, aneurysm, or even a brain tumor.” Magnetic resonance angiography (MRA) may be necessary, he added, if you suspect a vascular abnormality such as a dissection or aneurysm, or magnetic resonance venography (MRV) if you suspect a venous problem such as venous sinus thrombosis.
If you suspect infiltration by a squamous cell carcinoma, for example, it is essential to carefully check for enlargement of the first division of the trigeminal nerve on MRI, said Dr. Sergott.
(click to expand)
Next Steps
If the patient shows signs of significant visual loss, GCA, bleeding, or a tumor, it makes sense to send him or her directly to the ER, said Dr. Friedman. The same is true for papilledema, unless you’re certain you can get outpatient imaging done very quickly. When in doubt, call a neurologist, neuro-ophthalmologist, or emergency physician, she said.
What you don’t want to do, said Dr. Sergott, is to send the patient back to the primary care physician. The patient needs a workup by a specialist more familiar with the central nervous system.
If the exam is normal, and a primary headache syndrome is the cause, the patient can be safely referred back to their primary care physician or neurologist. But in most other cases, it is important to ensure that any ocular problems found resolve over time, said Dr. Bhatti. Be sure to make arrangements for ophthalmic follow-up. “After an aneurysm has been treated, for example, you want to make sure the double vision goes away. If it doesn’t, you might help with prisms or refer the patient to a strabismus specialist. Or if there is permanent and profound visual loss, referral to a low vision specialist may be the best approach.”
___________________________
Head and Facial Pain, Part 2—An overview of the primary headache syndromes will appear in the next EyeNet.
___________________________
1 EyeNet. 2012;16(6):38-46.
___________________________
M. Tariq Bhatti, MD, is associate professor of ophthalmology and medicine (division of neurology) and chief of the neuro-ophthalmology service at Duke Eye Center, Duke University Medical Center, in Durham, N.C. Financial disclosure: None. Deborah I. Friedman, MD, MPH, is professor of neurology and neurotherapeutics and ophthalmology at the University of Texas Southwestern Medical Center in Dallas. Financial disclosure: None. Robert C. Sergott, MD, is director of neuroophthalmology at Wills Eye Institute, Wills Eye Health System, in Philadelphia. Financial disclosure: None.