Download PDF
Painful and disabling, primary headache syndromes affect people of all ages and races and are among the most common disorders of the nervous system. Not only do chronic primary headache syndromes directly impair quality of life but they may also be accompanied by comorbidities such as depression, which is three times more common in those with severe chronic headaches.1
Because they may attribute their pain to eye problems or have visual symptoms along with head pain, many patients initially seek help from an ophthalmologist. The clinician’s critical first task is to rule out ocular or orbital pathology and life-threatening neurological conditions, as discussed last month in Part 1, “.” Beyond that, ophthalmologists can play an important role in identifying and appropriately referring patients with primary headaches.
|
Headache With Horner
|
 |
|
Horner syndrome may occur in primary headache disorders, especially the trigeminal autonomic cephalgias.
|
Migraine Headaches
Often experienced as pain in, around, and behind the eye, migraine is the most common primary headache disorder seen in physicians’ offices, said Benjamin M. Frishberg, MD, at the Neurology Center of Southern California.
These patients often have ophthalmic complaints, such as blurred vision or unilateral dilated pupil, said Deborah I. Friedman, MD, MPH, at University of Texas Southwestern Medical Center. In addition, visual auras, often lasting five to 20 minutes—but sometimes up to an hour—may precede, accompany, or follow the headache.2
Migraine diagnosis and misdiagnosis. “You need to be circumspect about diagnosing migraine, however, especially when the headache is severe and new,” said Dr. Frishberg. “When ophthalmologists don’t find an eye problem, I’ve noticed that they tend to jump to migraine too quickly.”
But, on the other hand, many migraine patients are missed because their condition is mistaken for tension or sinus headaches, said Kathleen B. Digre, MD, at the University of Utah. Light sensitivity, disability from the pain, and nausea are hallmarks of migraine, she said. If these patients’ headaches last four to 72 hours and they’ve had them before, added Dr. Frishberg, by definition, that’s migraine.
Dr. Frishberg said that a diagnosis of migraine is likely if a patient experiences two or more of the following pain symptoms:
- Unilateral pain
- Throbbing or pulsating quality
- Moderate or severe in intensity
- Increasing pain with movement or exertion
Plus one or more of the following:
- Nausea and/or vomiting
- Sensitivity to light and sound
Who gets migraine? Migraine is often triggered by alterations in homeostasis, said Dr. Frishberg, such as changes in stress, sleep, time zones, or altitude. Anyone, including children, can get migraines, but they are three times more common in women than in men, said Dr. Friedman. About 80 percent of people with migraine have a family history of headaches. “Adults with migraine often also have a history of motion sickness and unexplained vomiting, nausea, abdominal pain, or vertigo in childhood,” she said.
Migraine mechanisms. Migraine is a neurovascular disorder causing vasoconstriction of meningeal blood vessels, said Dr. Frishberg. But the mechanism of migraine is complex, involving local sterile inflammation, the interaction of multiple neurotransmitters, and cortical spreading depression via trigeminovascular pathways.2
“The speed at which this cortical spreading depression marches across the cortex correlates perfectly with the speed of the most characteristic visual aura as it spreads across the visual field,” said Dr. Friedman.
Ophthalmic contributors. To confirm any contributors to migraine, listen carefully to the patient’s complaint, said Dr. Digre. First, rule out eye diseases that can cause secondary headache, such as herpes zoster or angle-closure glaucoma. Then consider ophthalmic issues that may initiate or exacerbate headaches in people who are genetically predisposed to chronic migraine, she said, including:
- Improper refraction. Eyestrain can result when people fight their refraction, which can worsen headache.
- Dryness. The cornea has a high density of trigeminal nerve endings that project straight into the trigeminal nuclei—which are thought to be involved in the pain processing of headaches, she said. A poorly lubricated cornea can make matters worse.
- Subtle diplopia. For most people, a little convergence or divergence insufficiency causes no problem. “But for people predisposed to headache, double vision can add discomfort, and then they’re off to the races with more migraine,” said Dr. Digre.
- History of eye injury. A corneal scar or even a scleral buckle used to treat retinal detachment can contribute to migraine—again, due to trigeminal input from the cornea and the eye.
Classic auras. Most people who have migraines have no aura, said Dr. Frishberg, but when they do, 9 in 10 patients have visual auras, which are usually binocular and appear either centrally or in one visual field. “Patients often interpret the disturbance as being monocular when it occurs peripherally,” he said.
The classic visual aura produces a zigzag scintillating scotoma, usually with a shimmering quality at the edges, said Dr. Friedman. Sometimes it is silver and white, sometimes in color. “It gradually expands and takes on a C shape, marching across the visual field, getting larger, and then breaking up within 15 to 30 minutes.”
Other types of auras. More unusual variations include spots or sparkles, tunnel vision, kaleidoscopic vision, loss of color, “heat waves,” and Alicein-Wonderland syndrome, in which objects appear too big or too small. “Patients may also have episodes of transient monocular visual loss, often occurring in midlife,” said Dr. Friedman. “These are clinically impossible to distinguish from a transient ischemic attack [TIA], so they need to be worked up, even if the patient has a history of migraine.”
As migraine sufferers age, they sometimes lose the headache but continue—or even start—to have auras, said Dr. Digre. There are many causes of aura without headache, so this, too, may warrant a workup. However, she emphasized, the tip-off for an embolic phenomenon is abrupt onset, whereas with migraine auras, the progression is gradual.
Rarely, patients experience nonvisual auras, such as tingling in the face and hands, weakness, or trouble with speech, said Dr. Frishberg. As with transient monocular visual loss, these symptoms may look like a TIA, “in which case the patient would need to be seen immediately by a neurologist or go to the emergency room,” he said.
Mimics of migraine. Another possible masquerader of migraine is arteriovenous malformation, which can cause episodic headaches with aura, said Dr. Frishberg. In addition, said Dr. Friedman, intermittent angle-closure glaucoma can mimic a migraine headache without an aura.
(click to expand)
Trigeminal Autonomic Cephalgias
The trigeminal autonomic cephalgias (TACs) are another, less common, group of primary headaches ophthalmologists may see. Although primary TACs cause no complications, there are many secondary causes of TACs, so all require imaging, added Dr. Frishberg.
Common themes. TACs share common characteristics, said Dr. Friedman: pain in or around the eyes, associated with autonomic symptoms. “The headache is one sided and side locked—always occurring on the same side—and is generally severe and episodic,” she said. Autonomic symptoms, which occur on the same side as the headache, may include tearing, conjunctival injection, ptosis, eyelid swelling, miosis, and stuffy or runny nose.
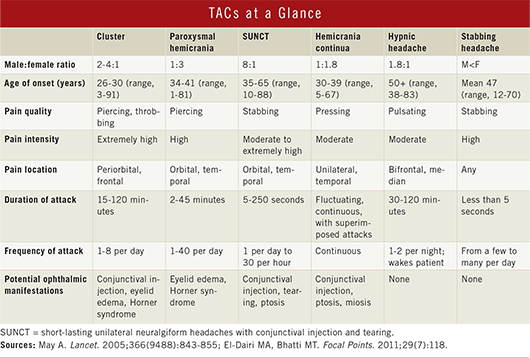
TACs vary in their intensity, duration, and frequency (see “TACS at a Glance”). For example, the pain of cluster headache is intense, lasting 15 minutes to a couple of hours, and usually occurs a few times a day. However, short-lasting unilateral neuralgiform headaches with conjunctival injection and tearing (SUNCT) last only for seconds to minutes, but they cause very intense pain that can strike dozens or even hundreds of times a day, said Dr. Frishberg.
Cluster headache. The most common type of TAC, cluster headache is diagnosed two to four times more frequently in men than in women. However, they may be underdiagnosed in women, said Dr. Friedman. “If a patient walks in and says, ‘These headaches are so bad I want to kill myself when they happen,’ it’s probably cluster.”
Cluster headaches typically start in the third or fourth decade of life and often occur at the same time every year, said Dr. Frishberg. As well as this circannual rhythm, there is typically a circadian pattern, and patients may get these headaches at the same time of day, often two or three hours after falling asleep.
Hemicrania continua. This rare type of TAC may be missed by ophthalmologists, said Dr. Friedman. “Every time I lecture about this, someone tells me they think they’ve seen several of these patients and didn’t know what it was. The other TACs are more obvious due to their dramatic features.”
This headache is just what its name suggests: a constant headache that is present on one side of the head. It may be localized around the eyes or at the back of the head, said Dr. Friedman. Although fluctuating in intensity, the pain persists and is accompanied by autonomic features when the intensity increases.
“You can be a real hero or heroine by considering indomethacin for these patients,” said Dr. Digre. In fact, one of the diagnostic pointers for hemicrania continua is its response to treatment with indomethacin, said Dr. Friedman, adding that the medication is like magic for these patients. “You will probably need to enlist an internist or neurologist to prescribe it, however—it’s a tough drug to take because of gastrointestinal side effects,” she added.
Primary stabbing headache. “This one scares patients,” said Dr. Friedman. “It’s a benign headache disorder, but the pain is so severe—out of the blue—that they think something is horribly wrong with them. Patients may say, ‘It’s like a bolt of lightning or an ice pick stabbed me in the head.’”
Lasting seconds or minutes, the pain is very focal and localized, occurring anywhere in the head, but it sometimes feels as if it’s in the eyes, Dr. Friedman said. “I think many of these people get misdiagnosed with dry eye.” Like hemicrania continua, these episodic, stabbing headaches are also responsive to indomethacin.
Other TACS. A discussion of all the TACS is beyond the scope of this article; see “TACS at a Glance” for the major characteristics of other types.
Tension Headaches
Even though tension headaches are extremely common, with a lifetime prevalence of up to 90 percent, people rarely see a doctor for these headaches, said Dr. Frishberg. They are usually mild and respond to over-the-counter medication. They tend to cause diffuse, bilateral, mild to moderate pressure-like pain, and sometimes light or sound sensitivity.
When severe, tension headaches may also cause throbbing and pain in or behind the eyes, said Dr. Friedman, which may suggest migraine. “The thing that separates them best from migraine is that tension headaches don’t worsen with activity, but migraines do.”
___________________________
1 World Health Organization. Headache disorders. October 2012. www.who.int/mediacentre/factsheets/fs277/en/. Accessed May 9, 2013.
2 El-Dairi MA, Bhatti MT. Focal Points. 2011;29(7):118.
___________________________
Kathleen B. Digre, MD, is professor of neurology and ophthalmology at the University of Utah School of Medicine in Salt Lake City. Financial disclosure: None.
Deborah I. Friedman, MD, MPH, is professor of neurology and neurotherapeutics and ophthalmology at University of Texas Southwestern Medical Center in Dallas. Financial disclosure: Is a speaker for Allergan; is on MAP Pharmaceuticals advisory board and Neurology Reviews’ editorial board; and has received grant support from GammaCore, Merck, and the National Eye Institute.
Benjamin M. Frishberg, MD, is in practice at the Neurology Center of Southern California in Encinitas. Financial disclosure: Is on the speakers bureau for Allergan.